Last Updated on October 31, 2025 by Saadet Demir

Knowing how often breathing stops during sleep is key to spotting sleep apnea. At Liv Hospital, we check the Apnea-Hypopnea Index (AHI) to see how bad sleep apnea is.
The AHI counts how many times breathing slows or stops per hour while sleeping. This important number helps our team give reliable checks and care plans that fit each person.
Getting a correct diagnosis means counting apnea events per hour with AHI scores. This lets us help our patients sleep better.
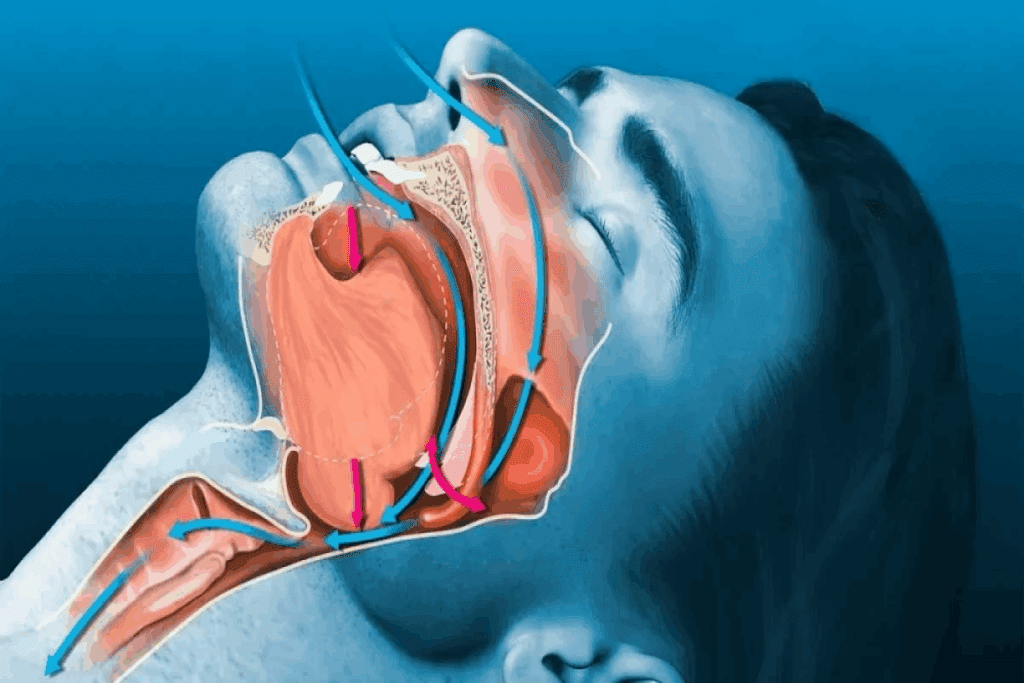
Sleep apnea is a sleep disorder that affects breathing during sleep. It can greatly impact a person’s quality of life and health.
An apnea episode is when breathing stops for at least 10 seconds. These pauses can happen many times a night, disrupting sleep. Apneas are pauses in breathing that reduce airflow. Hypopneas are blockages that affect breathing and lower oxygen levels.
There are several types of sleep apnea, with obstructive sleep apnea (OSA) being the most common. OSA happens when the airway is blocked, stopping normal airflow. Other types include central sleep apnea, related to brain control, and mixed sleep apnea, a mix of obstructive and central.
Sleep apnea can greatly affect sleep quality and health. The interruptions in breathing can cause fragmented sleep and lower blood oxygen. Adults with fewer than five apnea events per hour are considered normal. Five or more events indicate sleep apnea.
| AHI Score | Sleep Apnea Severity | Health Implications |
| Less than 5 | Normal | No significant health implications |
| 5-14 | Mild OSA | Mild sleep disruptions, possible daytime fatigue |
| 15-29 | Moderate OSA | Noticeable sleep disruptions, increased health risks |
| 30 or more | Severe OSA | Significant sleep disruptions, serious health risks |
Knowing the severity of sleep apnea is key to finding the right treatment. It helps avoid serious health risks.

The Apnea-Hypopnea Index (AHI) is key in sleep medicine. It shows how bad sleep apnea is. It counts pauses in breathing per hour of sleep.
To find the AHI, you add up apneas and hypopneas. Then, divide by hours slept. For example, 30 apneas and 50 hypopneas in 8 hours equals 10 events per hour.
Key components in AHI calculation include:
It’s important to know the difference between apneas and hypopneas. Apneas stop airflow completely. Hypopneas reduce airflow but not to zero. Both can lower blood oxygen and disrupt sleep.
The main differences are:
| Event Type | Description | Impact on Breathing |
| Apnea | Complete cessation of airflow | Total loss of breath |
| Hypopnea | Partial reduction in airflow | Partial loss of breath |
AHI is the top choice for diagnosing sleep apnea. It shows how often and how bad breathing stops during sleep. A higher AHI means more severe sleep apnea.
AHI scores are categorized as follows:
Knowing about AHI helps doctors create better treatment plans. This improves health for people with sleep apnea.
Healthcare professionals use a diagnostic process to find out how severe sleep apnea is. They look at how many apnea events happen per hour. This helps them understand how sleep apnea affects a person’s health and plan the best treatment.
An apnea or hypopnea must last at least 10 seconds to be counted. This rule is key to tell normal breathing pauses from serious ones. Sleep studies monitor breathing patterns to spot and record these events.
Apnea events are pauses in breathing that can happen many times at night. The total number of these events helps calculate the Apnea-Hypopnea Index (AHI). This index is important for diagnosing sleep apnea.
Oxygen levels in the blood are also checked during diagnosis. Apnea or hypopnea can lower these levels. The study measures how much oxygen levels drop to see how bad the breathing problems are.
The table below shows how different oxygen desaturation levels relate to severity:
| Oxygen Desaturation Level | Severity |
| <3% | Mild |
| 3-4% | Moderate |
| >4% | Severe |
Sleep arousals are brief wake-ups due to apnea events. These disrupt sleep, causing fatigue and other symptoms during the day.
Sleep arousal patterns are watched in sleep studies. They help doctors see how apnea affects sleep quality. This helps them understand the severity of sleep apnea and its health impact.
Healthcare professionals look at duration, oxygen levels, and sleep patterns to accurately diagnose sleep apnea. They then create a treatment plan that fits the patient’s needs.
Knowing about AHI scores is key to spotting sleep apnea. The Apnea-Hypopnea Index (AHI) counts apnea and hypopnea events per sleep hour. It shows how severe sleep apnea is.
An AHI score of fewer than 5 events per hour is normal. It means sleep is not disrupted much by apnea or hypopnea. People with scores in this range likely don’t have sleep apnea.
An AHI score of 5 or more means sleep apnea is present. The severity depends on the score:
These scores show sleep disruptions that could harm health and quality of life.
When looking at AHI scores, age and gender matter. AHI scores change with age, and different ages have different thresholds. Also, sleep apnea affects men more than women. Doctors must consider these when diagnosing and treating sleep apnea.
Understanding AHI scores helps doctors give better diagnoses and treatment plans for sleep apnea patients.
When the apnea-hypopnea index (AHI) score is between 5 and 14, it shows mild obstructive sleep apnea (OSA). At this point, people may notice symptoms that make life harder.
Mild OSA can cause many symptoms, including:
These symptoms happen because breathing stops during sleep. This disrupts the sleep cycle, making sleep poor. It’s key to catch these symptoms early to avoid bigger problems.
For mild OSA, treatment often starts with simple changes. These include:
In some cases, continuous positive airway pressure (CPAP) therapy is suggested. It keeps the airway open. Oral appliances that move the jaw forward can also help.
If mild OSA is not treated, it can get worse. This can lead to serious health problems, such as:
Early treatment is vital to avoid these issues. It helps keep health and well-being in check.
“Sleep is the golden chain that ties health and our bodies together.” – Thomas Dekker
Understanding and treating mild OSA can greatly improve sleep and health.
An Apnea-Hypopnea Index (AHI) score between 15 and 29 shows moderate obstructive sleep apnea. This condition needs careful management. It’s a serious sleep disorder that affects health and quality of life.
Moderate obstructive sleep apnea has symptoms like loud snoring and breathing stops during sleep. It also causes daytime sleepiness. These symptoms can make daily life hard and affect well-being.
Health risks from moderate OSA are big. They include heart disease, high blood pressure, and stroke. It can also make diabetes and depression worse.
The code G47.33 is for moderate obstructive sleep apnea for billing. It’s key for insurance claims and medical records. Knowing this code helps patients deal with the healthcare system better.
Insurance for treating moderate OSA varies. Patients should check their policies to see what’s covered and what’s not.
Treatment for moderate obstructive sleep apnea is vital to avoid more health problems. Continuous Positive Airway Pressure (CPAP) therapy is a common treatment. It keeps the airway open during sleep.
Other treatments include lifestyle changes like losing weight and sleeping in a different position. Oral appliances that keep the airway open are also used. Sometimes, surgery is needed to remove blockages.
Severe sleep apnea is diagnosed when someone has 30 or more apnea episodes an hour. This shows the need for strong treatment. It’s a serious condition that affects health and quality of life a lot.
Severe sleep apnea can lead to serious health problems. These include a higher risk of heart disease, stroke, and diabetes. The breathing stops and starts during sleep, causing low oxygen levels and affecting the heart.
Dr. John Smith, a sleep specialist, says, “Severe sleep apnea is a ticking time bomb for cardiovascular disease if left untreated.”
| Health Consequence | Description |
| Cardiovascular Disease | Increased risk due to strain on the heart from repeated breathing interruptions. |
| Stroke | Higher risk due to damage to blood vessels and the brain. |
| Diabetes | Association with insulin resistance and metabolic syndrome. |
Treatment for severe sleep apnea includes many steps. These include lifestyle changes, CPAP therapy, and sometimes surgery. The goal is to lower the number of apnea episodes and reduce health risks.
Managing severe sleep apnea needs ongoing monitoring and treatment adjustments. Regular check-ups with healthcare providers are key. They help see if treatments are working and make changes if needed.
“Continuous monitoring and adaptation of treatment strategies are key to managing severe sleep apnea effectively,” says Dr. Jane Doe, a leading expert in sleep medicine.
To understand sleep apnea, a detailed diagnosis is needed. This usually involves a sleep study or home test. Finding out if you have sleep apnea is key to getting the right treatment and improving your life.
A sleep study, or polysomnography, is a detailed test for sleep apnea. It tracks your brain waves, muscle activity, heart rate, and breathing while you sleep. This helps doctors see how often and how bad apnea events are.
This test can be done in a sleep lab or at home with portable gear. At a lab, you sleep all night while being watched. It’s easy and doesn’t hurt, giving doctors important sleep info.
Home sleep apnea testing (HSAT) is another option. It uses a portable device to check your breathing and oxygen levels at home. It’s good for those who can’t go to a lab or prefer their own bed.
Even though HSAT is not as detailed as a lab test, it works well for diagnosing sleep apnea in high-risk patients. But, it might not give as much info as a lab study.
After a sleep study, the data is checked to see if you have sleep apnea. The Apnea-Hypopnea Index (AHI) is key. It shows how many apnea or hypopnea events you have per hour of sleep.
| AHI Score | Severity of Sleep Apnea | Implications |
| Less than 5 | Normal | No sleep apnea diagnosis |
| 5-14 | Mild | Mild sleep apnea; treatment may be recommended based on symptoms |
| 15-29 | Moderate | Moderate sleep apnea; treatment is usually necessary |
| 30 or more | Severe | Severe sleep apnea; aggressive treatment is necessary |
Knowing your AHI score is important for managing sleep apnea. Doctors will look at your results, talk about what they mean, and suggest treatments based on your case.
Knowing your Apnea-Hypopnea Index (AHI) score is key to finding the right sleep apnea treatment. Your AHI score shows how severe your sleep apnea is. It helps us choose the best treatment for you.
If you have moderate obstructive sleep apnea syndrome, we take a more serious approach. We work with you to create a treatment plan. This might include changing your lifestyle, using an oral appliance, or CPAP therapy.
It’s important to act on your AHI score to manage sleep apnea well. This way, you can sleep better, avoid health problems, and feel better overall.
We’re here to provide top-notch healthcare and support for patients from around the world. Our team is ready to help you through your sleep apnea treatment. We aim to give you the care and support you need.
Sleep apnea is a sleep disorder where breathing stops or gets shallow during sleep. It’s diagnosed by counting pauses in breathing per hour of sleep.
The AHI shows how severe sleep apnea is. It’s found by dividing the number of breathing pauses by the sleep hours.
A normal AHI score is under 5 events per hour.
There are three main types: obstructive sleep apnea (OSA), central sleep apnea, and complex sleep apnea. OSA is the most common, caused by a blocked airway.
Apneas and hypopneas disrupt sleep, leading to poor quality and health risks. These include heart disease, diabetes, and brain problems.
Mild OSA has 5-14 pauses per hour. Symptoms include snoring, tiredness, and headaches in the morning.
Moderate OSA has 15-29 pauses per hour. Treatment includes lifestyle changes, oral appliances, and CPAP therapy.
Severe sleep apnea, with 30 or more pauses per hour, can cause serious health issues. These include heart disease, stroke, and brain problems.
Sleep apnea is diagnosed with sleep studies or home tests. These measure breathing, oxygen levels, and sleep stages.
The code for moderate OSA is G47.33.
Older adults and men are more likely to have sleep apnea. This is because of age and gender differences.
Treatments include lifestyle changes, oral appliances, and CPAP therapy. Each treatment is based on the person’s needs and AHI score.
To understand sleep study results, look at the AHI score and oxygen levels. Always talk to a healthcare professional for help.
Knowing your AHI score and acting on it is key. It helps manage sleep apnea and prevent health problems.
National Center for Biotechnology Information. (2025). How Many Apnea Events Per Hour Indicate Sleep. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6140019/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!