Many men worry that an enlarged prostate means cancer. But, medical studies show this isn’t true. Having Benign Prostatic Hyperplasia (BPH) doesn’t raise the chance of getting prostate cancer.
At Liv Hospital, we get why men are worried about prostate health. BPH and prostate cancer can both cause urinary problems and high PSA levels. Yet, they are different diseases needing different tests.
It’s key to know the differences between BPH and prostate cancer. We use the latest tech and care with kindness to meet each patient’s needs.
Learn the key differences between BPH vs prostate cancer. We explain if an enlarged prostate is a sign of cancer and the need for a diagnosis.
Key Takeaways
- BPH and prostate cancer are distinct conditions affecting the prostate gland.
- Having BPH does not increase the risk of developing prostate cancer.
- Both conditions can cause similar urinary symptoms and elevated PSA levels.
- Distinct diagnostic approaches are required for BPH and prostate cancer.
- Understanding the differences between BPH and prostate cancer is essential for making informed health choices.
Understanding the Prostate Gland: Anatomy and Function

The prostate gland is a key part of the male body. It surrounds the urethra and helps make seminal fluid. This small gland is below the bladder and is vital for fertility and sexual health.
What is the Prostate Gland?
The prostate gland is a vital organ in the male body. It sits between the bladder and penis, around the urethra. The gland has glandular and muscular tissues. It produces fluid for sperm and helps expel it during ejaculation.
Normal Prostate Function
The prostate gland mainly makes a lot of the fluid in semen. This fluid, called prostatic fluid, feeds and protects sperm. The gland’s muscles also help push this fluid into the urethra during ejaculation.
Age-Related Changes in the Prostate
As men get older, the prostate gland changes. One common change is the prostate getting bigger, known as benign prostatic hyperplasia (BPH). BPH isn’t cancer but can cause urinary problems. Knowing about these changes helps keep the prostate healthy.
What is Benign Prostatic Hyperplasia (BPH)?

Many aging men deal with Benign Prostatic Hyperplasia, or BPH. This condition makes the prostate gland grow bigger. We’ll look into what BPH is, how common it is, and what causes it.
Definition and Prevalence
BPH is a non-cancerous growth of the prostate gland. It’s a common problem for older men, affecting their daily life. Research shows that over half of men over 60 have BPH.
As men get older, BPH becomes more common. It’s a big health issue worldwide. With more people living longer, BPH cases are expected to increase.
Causes of BPH
The exact reason for BPH isn’t known, but hormonal changes are thought to play a part. The balance between estrogen and testosterone is important.
Other things that might contribute to BPH include:
- Genetic predisposition: Men with a family history of BPH are more likely to get it.
- Lifestyle factors: Diet, exercise, and other lifestyle choices can affect BPH risk.
Risk Factors for Developing BPH
Several factors increase the risk of BPH, including:
- Age: The risk grows after 40.
- Family history: Men with a family history of BPH are at higher risk.
- Obesity and lack of physical activity: Lifestyle choices can contribute to BPH.
Knowing these risk factors helps men prevent BPH and seek treatment early if symptoms appear.
What is Prostate Cancer?
Prostate cancer is a big health issue for men around the world. Knowing the basics is key for catching it early and treating it. We’ll look at what it is, how common it is, its types, and risk factors to give you a full picture.
Definition and Prevalence
Prostate cancer happens in the prostate gland, a small gland in men. It’s when abnormal cells grow out of control. The American Cancer Society says it’s the second most common cancer in men in the U.S., after skin cancer.
In the U.S., about 1 in 8 men will get prostate cancer. It’s more common in older men, with most being diagnosed around age 66.
Types of Prostate Cancer
There are many types of prostate cancer, but adenocarcinoma is the most common. It starts in the glandular cells of the prostate. Other types include small cell carcinoma and sarcomas.
Prostate cancer can grow fast or slow. Knowing the type helps doctors choose the best treatment.
Risk Factors for Prostate Cancer
Several things can raise a man’s chance of getting prostate cancer. Age is a big one, with most cases happening in men over 65. Family history also matters, with a higher risk if a first-degree relative has it.
Being African American increases the risk too. Genetic factors, like BRCA1 and BRCA2 mutations, can also play a part. Lifestyle and environment might also affect the risk, but more research is needed.
BPH vs Prostate Cancer: Understanding the Fundamental Differences
Knowing the difference between BPH and prostate cancer can ease worries and help choose the right treatment. Both affect the prostate gland but in different ways. This knowledge is key for men’s health.
Cellular Changes and Growth Patterns
The main difference is in how cells grow and change. BPH is a non-cancerous enlargement of the prostate gland, caused by too many prostate cells. On the other hand, prostate cancer grows from bad cells that don’t stop.
Let’s look at how these two conditions differ in cell structure and growth:
Characteristics | BPH | Prostate Cancer |
Cellular Growth | Non-cancerous overgrowth | Malignant cell growth |
Potential for Metastasis | No | Yes |
Long-term Implications | Urinary symptoms, quality of life | Life-threatening if not treated |
Potential for Metastasis
Another big difference is metastasis. BPH is benign and does not metastasize. But prostate cancer can spread to other areas like bones, lymph nodes, and organs.
Long-term Health Implications
The health effects of BPH and prostate cancer are quite different. BPH can cause urinary problems and affect daily life but is not deadly. Prostate cancer, if not caught and treated early, can be deadly.
It’s important for men to understand these differences. It helps in making the right treatment choices and reduces worries about cancer in men with BPH.
Common Symptoms: How to Recognize Warning Signs
As men get older, they face a higher risk of prostate problems. Knowing the symptoms can help improve health outcomes. Both BPH and prostate cancer can greatly affect a man’s life, so it’s important to understand their symptoms.
Urinary Symptoms in BPH
BPH, or benign prostatic hyperplasia, causes urinary issues due to prostate enlargement. This can block urine flow, leading to symptoms like:
- Frequent urination, often at night
- Weak or interrupted urine flow
- Difficulty starting urination
- Dribbling of urine
These symptoms can be uncomfortable and affect daily life. But, they usually don’t mean cancer.
Warning Signs Specific to Prostate Cancer
Prostate cancer might not show symptoms early on. But, as it grows, men may notice:
- Blood in the urine or semen
- Pain or burning while urinating
- Pain in the back, hips, or pelvis that lasts
- Erectile dysfunction
These signs can mean advanced prostate cancer and need quick medical check-ups.
When Symptoms Overlap and When to Worry
BPH and prostate cancer can share similar urinary symptoms, making it hard to tell them apart. But, if you notice:
- Severe or lasting urinary symptoms
- Blood in the urine or semen
- Painful urination or ejaculation
- Unexplained weight loss or tiredness
Seeing a doctor early is vital for treating both BPH and prostate cancer. If you’re worried about symptoms, talk to your healthcare provider.
Does an Enlarged Prostate Lead to Cancer?
Many men wonder if an enlarged prostate means they’ll get prostate cancer. This is a common worry, as both Benign Prostatic Hyperplasia (BPH) and prostate cancer are common in older men.
The Scientific Evidence
Research has shed light on the link between BPH and prostate cancer. It shows that BPH itself doesn’t raise the risk of prostate cancer. But, both conditions can happen together, making diagnosis tricky.
A study in the Journal of Urology found no increased risk of prostate cancer in men with BPH. This means BPH and prostate cancer are different, even though they both affect the prostate.
“The presence of BPH does not appear to increase the risk of prostate cancer, but it can complicate the diagnosis due to overlapping symptoms.”
Medical Expert, Urologist
Common Misconceptions
Many think an enlarged prostate means they’ll get prostate cancer. But, BPH is not a cancer and doesn’t lead to it. Prostate cancer is a different issue, involving cancerous cell growth.
Some also believe BPH symptoms mean they’re at higher risk for cancer. But, studies show this isn’t true. The severity of BPH symptoms doesn’t predict cancer risk.
What Research Tells Us About the Relationship
Research shows BPH and prostate cancer share some risk factors like age and hormones. But, they are not the same. Having BPH does not increase the risk of getting prostate cancer.
Condition | Nature | Risk Factors |
BPH | Non-cancerous enlargement | Age, hormonal changes |
Prostate Cancer | Malignant growth | Age, family history, genetics |
It’s important to know the difference between BPH and prostate cancer. If you’re experiencing symptoms, see your doctor. They can figure out what’s going on and help you.
Diagnosis Methods: Differentiating BPH from Prostate Cancer
To tell BPH from prostate cancer, doctors use many tests. Finding the right diagnosis is key to choosing the best treatment.
Initial Screening and Physical Examination
The first step is a detailed medical history and physical check-up. A doctor might do a digital rectal exam (DRE) to feel the prostate gland.
A DRE can spot problems like nodules that might mean cancer. But, it’s not enough to say for sure if you have cancer.
Blood Tests and PSA Levels
Blood tests, like the prostate-specific antigen (PSA) test, are very important. High PSA levels can mean BPH or cancer.
The PSA test checks PSA levels in your blood. High levels mean you might need more tests.
PSA Level | Interpretation |
0-4 ng/mL | Generally considered normal |
4-10 ng/mL | May indicate BPH or prostate cancer |
>10 ng/mL | May indicate prostate cancer |
Imaging Studies and Their Limitations
Tests like ultrasound and MRI can look at the prostate gland. They show its size and shape.
But, these tests can’t always tell BPH from cancer. We use them with other tests to get a clearer picture.
Biopsy and Confirmatory Testing
A biopsy is the best way to find prostate cancer. It takes small tissue samples from the prostate for a microscope check.
The biopsy results show if there’s cancer, how serious it is, and what treatment to use. A biopsy is key for cancer diagnosis but not for BPH.
In summary, diagnosing BPH and prostate cancer needs many steps. We use initial checks, blood tests, imaging, and biopsy together. This way, we can accurately find out what’s wrong with the prostate.
Treatment Approaches for BPH
Understanding the different ways to treat Benign Prostatic Hyperplasia (BPH) is key. The right treatment depends on how bad the symptoms are, your overall health, and what you prefer.
Watchful Waiting and Lifestyle Changes
For those with mild BPH symptoms, watchful waiting is often suggested. This means regular check-ups to keep an eye on symptoms and prostate health. Making lifestyle changes can also help manage BPH symptoms. These changes include:
- Limiting fluids before bedtime to reduce nighttime urination
- Avoiding caffeine and alcohol, which can irritate the bladder
- Exercising regularly to improve overall health
- Maintaining a healthy weight to reduce the risk of BPH progression
Lifestyle modifications can greatly improve symptoms and quality of life. By making these changes, men can delay or avoid more serious treatments.
Medication Options
When symptoms are more severe, medication might be needed. There are two main types of medications for BPH: alpha-blockers and 5-alpha-reductase inhibitors.
Alpha-blockers relax the muscles in the prostate and bladder neck, making it easier to urinate. 5-alpha-reductase inhibitors shrink the prostate by blocking DHT, a hormone that makes the prostate grow.
Minimally Invasive Procedures
For those who don’t respond to medication or prefer not to take it long-term, there are minimally invasive options. These include:
- Transurethral microwave therapy (TUMT)
- Transurethral needle ablation (TUNA)
- Laser therapy
- Prostatic urethral lift
These procedures aim to improve urine flow and reduce prostate size. They often have fewer side effects than traditional surgery.
Surgical Interventions
When other treatments fail or symptoms are severe, surgery might be needed. The most common surgery for BPH is transurethral resection of the prostate (TURP).
Surgical options can offer significant relief for men with BPH, even for those with complicated cases or urinary retention. But, as with any surgery, there are risks and possible side effects to think about.
Treatment Strategies for Prostate Cancer
The treatment for prostate cancer varies based on the cancer’s type and the patient’s health. Knowing these details is key to picking the right treatment.
Active Surveillance
For those with low-risk prostate cancer, active surveillance is often suggested. This method involves regular PSA tests, clinical exams, and biopsies. It avoids immediate treatment.
Active surveillance is great for men with low-grade cancer. It helps avoid the side effects of aggressive treatments. But, it’s important to keep a close eye on the cancer to make sure it doesn’t grow.
Radiation Therapy Options
Radiation therapy is a treatment for prostate cancer. It uses high-energy rays to kill cancer cells. There are two main types: external beam radiation therapy (EBRT) and brachytherapy.
- EBRT sends radiation from outside the body to the prostate gland.
- Brachytherapy places radioactive seeds in the prostate for a stronger dose of radiation.
Radiation therapy can be used alone or with other treatments like hormone therapy. This depends on the cancer’s stage and the patient’s health.
Surgical Approaches
Surgery is a common treatment for prostate cancer, mainly for localized disease. The most common surgery is a radical prostatectomy. This removes the prostate gland and some surrounding tissue.
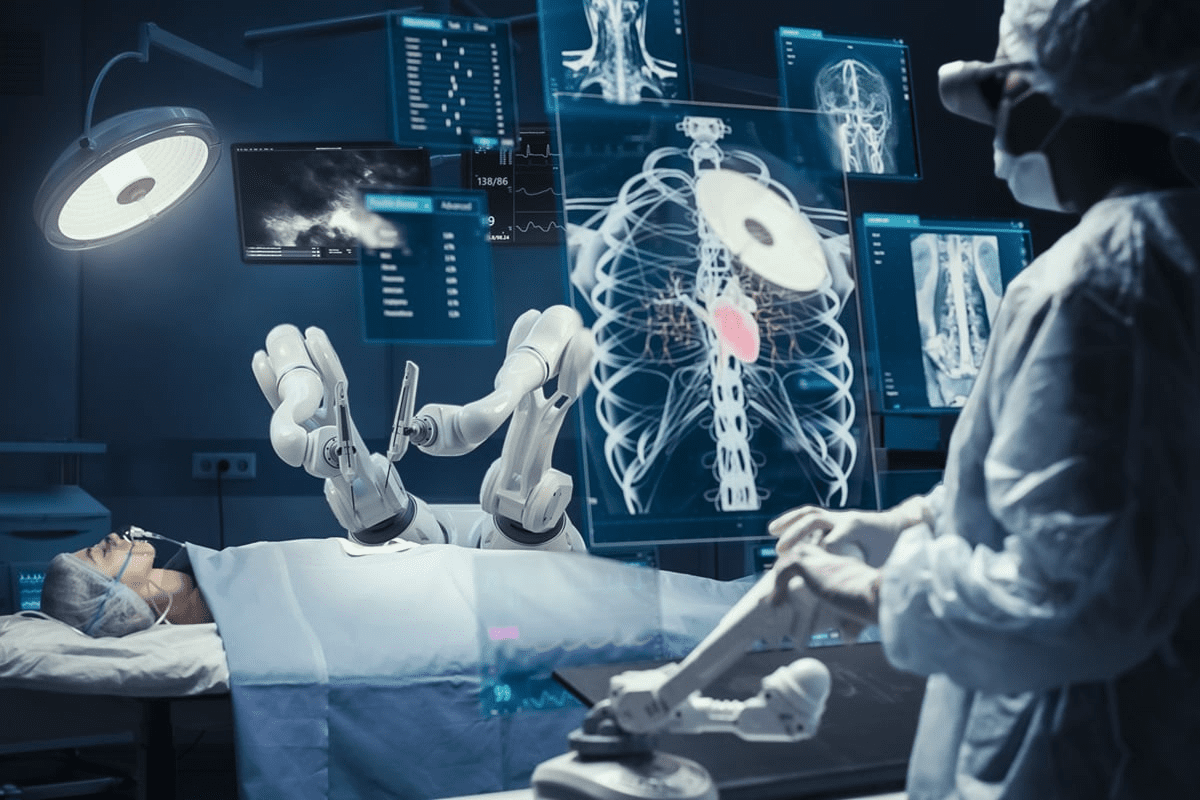
Surgical methods have improved, with options like open surgery, laparoscopic surgery, and robot-assisted surgery. The choice depends on the surgeon’s skill and the patient’s condition.
Hormone Therapy and Advanced Treatments
Hormone therapy, or androgen deprivation therapy (ADT), treats prostate cancer by lowering male hormones. This therapy can be used alone or with other treatments.
For advanced prostate cancer, treatments like chemotherapy, immunotherapy, and targeted therapy are considered. These aim to control the cancer, manage symptoms, and improve quality of life.
In conclusion, prostate cancer treatment is tailored to each patient. It considers the cancer’s type, the patient’s health, and personal preferences. Understanding the treatment options helps patients make informed decisions about their care.
Living with Prostate Conditions: Quality of Life Considerations
Men with prostate conditions face a big challenge in keeping their quality of life good. Conditions like Benign Prostatic Hyperplasia (BPH) and prostate cancer need medical care and lifestyle changes. We’ll look at how to manage symptoms, the emotional side of these conditions, and where to find help.
Managing Symptoms Day-to-Day
It’s key to manage symptoms well to keep a good quality of life. For BPH, making lifestyle changes helps a lot. This includes eating right, drinking the right amount of water, and doing pelvic floor exercises. For prostate cancer, dealing with symptoms from treatment, like not being able to control urine or having trouble getting an erection, is very important.
- Monitoring and adjusting fluid intake
- Pelvic floor exercises to improve bladder control
- Dietary adjustments to reduce urinary symptoms
Psychological Impact and Coping Strategies
The mental side of prostate conditions is just as important as the physical. Many patients feel anxious, depressed, or stressed. Counseling and cognitive-behavioral therapy can really help. Also, having support from loved ones and joining support groups is very important.
It’s good for patients to try different ways to cope and find what works for them.
Support Resources for Patients
Having access to support is key for those with prostate conditions. This includes support groups, counseling services, and online resources. These offer emotional support, practical tips, and a sense of community.
- Local support groups for men with prostate conditions
- Professional counseling services
- Online forums and resources
Conclusion: Maintaining Prostate Health and When to Seek Help
Keeping the prostate healthy is key for men’s well-being, more so as they get older. Regular health checks and screenings are important for catching problems early. Knowing the difference between BPH and prostate cancer helps make better health choices.
Knowing the signs and risks of prostate issues is important. It helps people get medical help when they need it. We urge readers to take care of their prostate health and see doctors if they notice any odd symptoms. This way, they can get the right care on time and live better.
Prostate health is a big part of men’s health. Staying informed and knowing when to get help is vital. By doing regular health checks, men can manage their health better and avoid serious problems.
FAQ
Does an enlarged prostate mean I have prostate cancer?
No, an enlarged prostate usually means you have Benign Prostatic Hyperplasia (BPH). This is a non-cancerous condition. BPH and prostate cancer are different, with BPH being non-cancerous and prostate cancer being cancerous.
Can an enlarged prostate lead to prostate cancer?
There’s no direct link between an enlarged prostate and prostate cancer. Studies show BPH and prostate cancer are separate issues. Having one doesn’t mean you’ll get the other.
What is the difference between BPH and prostate cancer?
BPH is a non-cancerous growth of the prostate gland. Prostate cancer is a malignant tumor in the prostate. They differ in cell changes, growth, and spread.
Are the symptoms of BPH and prostate cancer the same?
Both can cause urinary problems like trouble starting or stopping urination. But, prostate cancer often doesn’t show symptoms early. Later stages may bring pain or trouble with ejaculation.
How is BPH diagnosed, and how is it different from prostate cancer diagnosis?
BPH is diagnosed with medical history, physical exam, and tests like uroflowmetry. Prostate cancer is found with PSA tests and biopsies to check for cancer cells.
Can I have both BPH and prostate cancer at the same time?
Yes, it’s possible to have both BPH and prostate cancer. Both are more common with age, so many men get both as they get older.
How do treatment options differ for BPH and prostate cancer?
BPH treatment aims to manage symptoms with lifestyle changes, meds, or procedures. Prostate cancer treatment varies by stage and may include surveillance, surgery, radiation, or hormone therapy.
Is an enlarged prostate a sign of something serious?
An enlarged prostate usually means BPH, which is not serious. But, seeing a doctor is key to rule out prostate cancer.
Can lifestyle changes help manage BPH symptoms?
Yes, changes like diet, exercise, and bladder training can help with BPH symptoms.
What are the risk factors for developing prostate cancer?
Risk factors include age, family history, ethnicity, and genetic mutations. Knowing these can help with screening and prevention.
Reference
Government Health Resource. (2025). Is Enlarged Prostate a Sign of Cancer BPH. Retrieved from https://www.cancer.org/cancer/prostate-cancer.html