Benign prostatic hyperplasia with lower urinary tract symptoms (LUTS) affects millions of aging men. It can greatly reduce a man’s quality of life. Symptoms include needing to urinate often, having a weak urine flow, and waking up to urinate at night.
At Liv Hospital, we focus on the patient to help men understand this condition. We look at evidence-based treatments. Accurate diagnosis and coding are key, and the ICD-10 code for BPH with LUTS is N40.1.
Knowing what BPH with LUTS is is the first step to managing it. We will give an overview of the condition, its symptoms, and why accurate ICD-10 coding is important. This will prepare us for a deeper look into the condition’s prevalence, symptoms, and how to manage them.
Key Takeaways
- Benign prostatic hyperplasia with LUTS is a common condition in aging men.
- Accurate ICD-10 coding is key for effective management.
- The ICD-10 code for BPH with LUTS is N40.1.
- Symptoms include frequent urination, weak urine flow, and nocturia.
- Understanding the condition is the first step toward effective management.
Understanding BPH With LUTS: Definition and Pathophysiology
To understand BPH with LUTS, we need to know what each term means. We also need to see how they are connected.
Defining Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia (BPH) is when the prostate gland grows too big. This happens more often as men get older. The prostate is around the urethra, and when it gets too big, it can block the flow of urine.
BPH is not prostate cancer, even though both can cause urinary problems. The exact reason for BPH is not known, but it’s thought to be due to hormonal changes with age.
What Lower Urinary Tract Symptoms (LUTS) Encompass
Lower Urinary Tract Symptoms (LUTS) include a range of urinary issues. These can be caused by BPH or other conditions. LUTS symptoms are divided into three main types.
- Storage symptoms include daytime frequency, nocturia (getting up at night to urinate), urgency, and incontinence.
- Voiding symptoms encompass weak stream, straining to urinate, prolonged urination, and feeling like you haven’t fully emptied your bladder.
- Post-micturition symptoms include the feeling of incomplete bladder emptying and post-micturition dribble.
The Relationship Between BPH and LUTS
The link between BPH and LUTS is complex. BPH is a common cause of LUTS, but not all men with LUTS have BPH. Also, not all men with BPH have significant LUTS. But, as the prostate grows, it can block the urethra, causing LUTS symptoms.
The pathophysiology of BPH with LUTS has both static and dynamic parts. The static part is the physical blockage from the enlarged prostate. The dynamic part involves the muscle contractions and relaxations in the prostate and bladder neck.
Symptom Category | Examples of Symptoms | Possible Causes |
Storage Symptoms | Daytime frequency, nocturia, urgency | Bladder overactivity, BPH |
Voiding Symptoms | Weak stream, straining, prolonged urination | BPH, urethral stricture, bladder neck obstruction |
Post-micturition Symptoms | Incomplete bladder emptying, post-micturition dribble | BPH, detrusor underactivity |
Understanding BPH and LUTS helps us see how complex these conditions are. It shows why we need to manage them thoroughly.
Prevalence and Demographics of BPH With LUTS

BPH with LUTS affects more men as they get older. It impacts their quality of life, affecting millions worldwide. As men age, the chance of getting BPH with LUTS increases, making it a big health issue for older men.
Age-Related Prevalence Statistics
Research shows BPH with LUTS is more common with age. About 50% of men aged 50-59 have some LUTS symptoms. This number jumps to around 90% for men aged 70-79.
Age-related prevalence statistics show BPH with LUTS is a big health problem for older men. It affects not just urine symptoms but also overall health and well-being.
Risk Factors for Developing BPH With LUTS
Several factors can increase the risk of getting BPH with LUTS, including:
- Genetic predisposition: Family history can play a part in getting BPH.
- Lifestyle factors: Diet, exercise, and lifestyle choices can affect risk.
- Comorbid conditions: Having other health issues, like diabetes, can raise the risk.
Global and US-Specific Epidemiology
The spread of BPH with LUTS varies worldwide. In the United States, it’s a top reason for urologist visits and surgeries.
Studies show BPH with LUTS isn’t just age-related. It’s also affected by where you live and your ethnicity. Knowing these differences helps in making better public health plans.
Mechanisms Behind BPH With LUTS
BPH with LUTS involves prostate growth and increased muscle tone. Knowing these mechanisms helps us understand how BPH causes LUTS.
Static Mechanism: Prostate Enlargement
Prostate growth is key in BPH and LUTS. As the prostate gets bigger, it can block the urethra. This static obstruction is a main cause of BPH with LUTS. The enlarged prostate also distorts the urethral lumen, making urine flow harder.
Dynamic Mechanism: Smooth Muscle Contraction
Prostate growth isn’t the only issue. The contraction of smooth muscle in the prostate and bladder neck also plays a role. This smooth muscle tone is affected by alpha-adrenergic receptors. Muscle contraction can block urine flow, making BPH symptoms worse.
Bladder Adaptation to Obstruction
The bladder adapts to prostate enlargement in BPH with LUTS. At first, the bladder muscle (detrusor muscle) gets thicker and stronger. But, this can lead to detrusor overactivity or a decompensated bladder with weak contractility. Understanding these changes is key to managing BPH with LUTS.
Healthcare providers can now target treatments for BPH with LUTS. They know how prostate growth, muscle contraction, and bladder changes work together.
Recognizing Symptoms of BPH With LUTS
The symptoms of BPH and LUTS can be broken down into several main areas. Each area has its own set of symptoms that can greatly affect a person’s life.
LUTS linked to BPH fall into three main groups: storage, voiding, and post-micturition symptoms. Knowing these symptoms is key for a correct diagnosis and treatment plan.
Storage Symptoms
Storage symptoms deal with how urine is stored in the bladder. Common symptoms include:
- Urinary frequency: Needing to urinate more often than usual.
- Urinary urgency: A sudden, strong need to urinate.
- Nocturia: Waking up to urinate at least once a night.
These symptoms can really mess up your daily life and sleep, affecting your overall health.
Voiding Symptoms
Voiding symptoms happen when you’re trying to urinate. Key symptoms include:
- Weak or slow urinary stream: A decrease in urine flow.
- Straining to urinate: Needing to push hard to start or keep urinating.
- Prolonged urination: Taking longer than usual to empty the bladder.
These symptoms can be annoying and may show that there’s an obstruction, making it important to see a doctor.
Post-Micturition Symptoms
Post-micturition symptoms happen after you’ve finished urinating. Common symptoms include:
- Dribbling: Losing urine involuntarily right after you’ve finished urinating.
- Sensation of incomplete bladder emptying: Feeling like your bladder isn’t fully empty after you’ve urinated.
These symptoms can be upsetting and may show there’s an underlying problem that needs to be looked at.
It’s very important to accurately record these symptoms for diagnosis and treatment planning. Doctors use symptom scoring systems to measure how severe LUTS are. This helps them come up with the best treatment plan.
Diagnostic Approaches for BPH With LUTS
To diagnose BPH with LUTS, we need to look at the patient’s medical history, score their symptoms, and do a physical exam.
Initial Assessment and Medical History
First, we take a detailed medical history to find out the symptoms and rule out other possible causes. We check the patient’s overall health and any past urological issues or surgeries.
Symptom Scoring Systems
We use symptom scoring systems like the International Prostate Symptom Score (IPSS) to measure LUTS severity. The IPSS asks about symptoms like how often you pee, how urgent it is, and if your stream is weak. This score helps us understand how bad the symptoms are and what treatment might work best.
Physical Examination
A physical exam is key for diagnosing BPH with LUTS. We do a digital rectal exam (DRE) to check the prostate’s size, feel, and texture. This, along with the patient’s history and symptom score, helps us make a correct diagnosis.
Laboratory and Imaging Studies
We run lab tests like PSA, urinalysis, and serum creatinine to check the prostate’s health and rule out other issues. Imaging, like ultrasound, helps us see the prostate and bladder size. Uroflowmetry, a non-invasive test, measures urine flow rate to see how bad the blockage is.
By using these methods together, we can accurately diagnose BPH with LUTS. Then, we can create a treatment plan that fits the patient’s needs.
ICD-10 Coding for BPH With LUTS
Understanding ICD-10 codes for BPH with LUTS is key for healthcare providers. It helps in accurate diagnosis and planning treatment. Accurate coding is important for treatment, insurance, and tracking health trends.
Primary ICD-10 Codes for BPH With LUTS
The main ICD-10 code for BPH with LUTS is N40.1. This code classifies benign prostatic hyperplasia with lower urinary tract symptoms. It’s vital for keeping patient records accurate and tracking the condition well.
- N40.1: Benign prostatic hyperplasia with lower urinary tract symptoms
Healthcare providers also use secondary codes for more detailed patient information.
Secondary and Related Diagnostic Codes
Secondary codes report related symptoms or complications. For BPH with LUTS, codes for urinary retention, infections, or other issues might be used.
- R33.9: Retention of urine, unspecified
- N30.0: Acute cystitis
- N39.0: Urinary tract infection, site not specified
Using these secondary codes with the primary code N40.1 gives a full view of the patient’s health. It helps in treatment and administrative tasks.
Importance of Accurate Coding for Treatment and Insurance
Accurate ICD-10 coding is vital for both patient care and administrative tasks. It ensures patients get the right treatment and helps in insurance reimbursement.
Accurate coding leads to better health outcomes by ensuring consistent care. It also aids in tracking BPH with LUTS, helping in research and public health.
Treatment Options for BPH With LUTS
There are many ways to treat BPH with LUTS. These range from simple changes to surgery. The right choice depends on how bad the symptoms are, what the patient wants, and if there are any complications.
Watchful Waiting and Lifestyle Modifications
For those with mild symptoms, waiting and watching is a good start. This means keeping an eye on symptoms and PSA levels. Making lifestyle changes can also help manage symptoms.
- Fluid management: Adjusting fluid intake to reduce nocturia.
- Dietary changes: Avoiding caffeine and alcohol, which can exacerbate symptoms.
- Exercise: Regular physical activity can help improve urinary flow.
Pharmacological Interventions
When symptoms get worse, medicine is needed. There are two main types of drugs:
Alpha-blockersand5-alpha-reductase inhibitors.
- Alpha-blockers relax the muscles in the prostate and bladder neck, making it easier to urinate.
- 5-alpha-reductase inhibitors shrink the prostate over time, reducing symptoms.
Using both types of drugs together can work well for some patients.
Medication Class | Mechanism of Action | Examples |
Alpha-blockers | Relax prostate and bladder neck muscles | Tamsulosin, Alfuzosin |
5-alpha-reductase inhibitors | Shrink the prostate | Finasteride, Dutasteride |
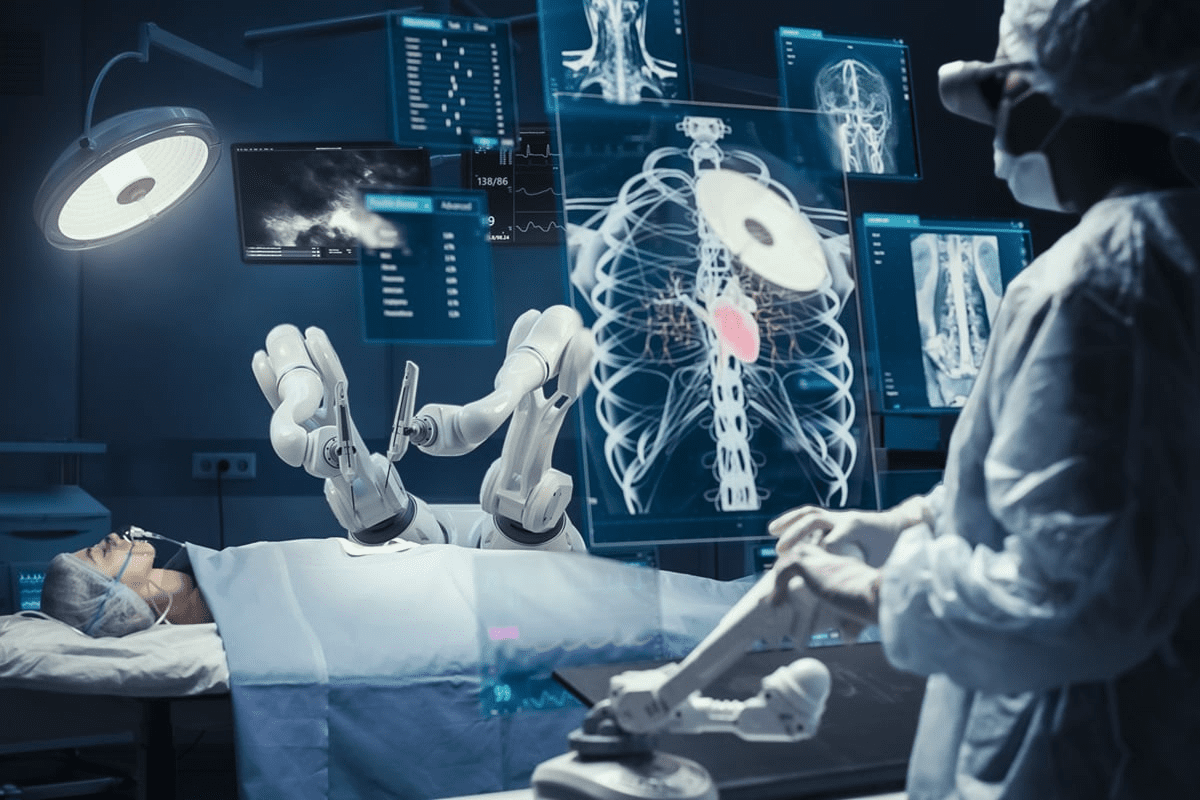
Surgical and Minimally Invasive Procedures
For severe symptoms or when medicine doesn’t work, surgery is an option. There are several types:
- Transurethral resection of the prostate (TURP)
- Laser surgery
- Open prostatectomy
Less invasive options like UroLift and Rezum also exist. They have fewer side effects.
Living With BPH With LUTS: Management Strategies
Living with BPH and LUTS can be tough, but the right strategies can make a big difference. A good plan includes medical treatment, lifestyle changes, and self-care. These steps can greatly improve your life quality.
Self-Management Techniques
Self-management is key when dealing with BPH and LUTS. Techniques like timed voiding help manage symptoms. Keeping a bladder diary also helps track habits and patterns.
Fluid management is another important technique. It involves watching and adjusting how much you drink. For example, drinking less before bed can reduce nighttime trips to the bathroom.
Dietary Considerations
Your diet is also important in managing BPH with LUTS. Some foods can make symptoms worse, while others can help. Cutting down on caffeine and alcohol can reduce how often you need to urinate.
Eating a balanced diet with lots of fruits, vegetables, and whole grains is best. Some research shows that a low-fat, high-fiber diet can help with BPH symptoms.
Exercise and Physical Activity
Regular exercise and physical activity are good for your health and can help with BPH symptoms. Activities like walking, cycling, or swimming can improve your symptoms and overall health.
Pelvic floor exercises, or Kegel exercises, are also helpful. They strengthen the muscles that support the bladder, improving urinary control.
When to Seek Medical Attention
While lifestyle changes and self-management can help, knowing when to see a doctor is important. If symptoms get worse or if you have signs of complications, like urinary retention or infection, get medical help right away.
Regular check-ups with your healthcare provider are also vital. They help monitor your condition and adjust your treatment plan as needed.
Conclusion: The Future of BPH With LUTS Management
As we learn more about Benign Prostatic Hyperplasia (BPH) with Lower Urinary Tract Symptoms (LUTS), the future looks bright. New research and treatments are on the horizon. These advancements aim to better manage symptoms and improve life quality for those affected.
We’re moving towards more tailored care for each patient. New treatments are not just helping patients; they’re also deepening our understanding of BPH with LUTS. This ongoing research is key to finding new ways to manage the condition.
New therapies are showing great promise for managing BPH with LUTS. These treatments are designed to tackle the complex issues of the condition. This means better symptom control for patients. It’s vital to keep investing in research and development to enhance patient care.
By adopting the latest in BPH with LUTS treatment, we’re on the path to better care for patients. The future of managing BPH with LUTS is exciting, thanks to ongoing research and new therapies. This will change the field for the better.
FAQ
What is BPH with LUTS?
BPH with LUTS is a condition where the prostate grows too much. This growth causes urinary symptoms.
What are the symptoms of BPH with LUTS?
Symptoms include trouble storing and emptying urine. They can also cause problems after you’ve finished urinating. These symptoms can really affect your life.
How is BPH with LUTS diagnosed?
Doctors use many steps to diagnose BPH with LUTS. They start with a check-up, ask about your health, and use special tests. They also do physical exams and imaging studies.
What is the ICD-10 code for BPH with LUTS?
The ICD-10 code helps doctors and insurance companies know how to handle BPH with LUTS. It’s important for treatment and billing.
What are the treatment options for BPH with LUTS?
Doctors have many ways to treat BPH with LUTS. They might suggest waiting and watching, changing your lifestyle, or using medicine. They might also suggest surgery or less invasive procedures.
How can I manage BPH with LUTS?
You can manage BPH with LUTS by taking care of yourself. Eat right, exercise, and stay active. Knowing when to see a doctor is also important.
What is the prevalence of BPH with LUTS?
BPH with LUTS is common in men, getting more common with age. It’s found more often in some places than others.
What are the risk factors for developing BPH with LUTS?
Risk factors include getting older, having a family history, and other factors. These can increase your chance of getting BPH with LUTS.
How does BPH cause LUTS?
BPH causes LUTS by making the prostate too big. This blocks urine flow. It also involves muscle contractions that make it harder to urinate.
What is the importance of accurate ICD-10 coding for BPH with LUTS?
Accurate ICD-10 coding is key for getting the right treatment and insurance coverage. It helps make sure you get the care you need.
References
National Center for Biotechnology Information. (2025). What Is BPH With LUTS Understanding Symptoms and. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK558920/