Many people wonder if their sore throat is from a virus or bacteria. Knowing the difference between viral and bacterial pharyngitis is key to getting better.
Is acute pharyngitis viral or bacterial? Learn how to differentiate between the two, which is crucial for determining treatment (antibiotics).
At Liv Hospital, we stress the need to tell these two apart. Up to 80 percent of sore throats are caused by viruses. Common viruses include rhinovirus, influenza, and adenovirus. But, bacterial pharyngitis, often caused by Group A Streptococcus (GAS), needs antibiotics.
Getting the right diagnosis is vital. It stops overuse of antibiotics and avoids bad side effects. Our team works hard to give each patient the best care based on science.
Key Takeaways
- Distinguishing between viral and bacterial pharyngitis is key for the right treatment.
- Viral pharyngitis is more common, with viruses like rhinovirus and influenza leading the way.
- Bacterial pharyngitis, mainly caused by Group A Streptococcus (GAS), needs antibiotics.
- Correct diagnosis stops too much antibiotic use and its risks.
- Liv Hospital’s team uses science to guide diagnosis and treatment.
Understanding Acute Pharyngitis
Acute pharyngitis is a common illness that affects the throat. It can be caused by viruses or bacteria. Symptoms include a sore throat, difficulty swallowing, and a feeling of pain when swallowing.
It’s important to know the causes of acute pharyngitis. Viruses like the common cold or flu can cause it. Bacteria, such as strep throat, can also lead to this condition.
Knowing the symptoms of acute pharyngitis is key to getting the right treatment. A sore throat is the most common symptom. You might also have difficulty swallowing or feel pain when swallowing.
It’s important to seek medical help if you have these symptoms. A doctor can diagnose acute pharyngitis and recommend the best treatment. They may prescribe antibiotics if it’s caused by bacteria.
Preventing acute pharyngitis is also important. Good hygiene practices can help. Washing your hands regularly and avoiding close contact with people who are sick can reduce the risk.
By understanding acute pharyngitis, its causes, symptoms, and prevention, you can take steps to protect your health. If you have concerns or symptoms, always seek medical advice.
Epidemiology of Acute Pharyngitis
It’s important to know about acute pharyngitis to fight it better. This illness leads to over 40 million doctor visits in the U.S. each year. It’s a big problem for public health.
Prevalence and Healthcare Impact
Acute pharyngitis is very common, with viruses being the main cause. Most cases of pharyngitis are caused by viral pathogens. This affects how we treat it and use antibiotics.
Here are some key facts about its impact on healthcare:
Condition | Annual Healthcare Visits | Primary Cause |
Acute Pharyngitis | 40 million+ | Viral Infections |
Viral Pharyngitis | Majority of cases | Common cold viruses, Influenza |
Bacterial Pharyngitis | Minority of cases | Group A Streptococcus (GAS) |
Seasonal Variations and Risk Factors
Acute pharyngitis has a pattern, with viral pharyngitis peaking in winter and early spring. This is when colds and flu are most common. Knowing this helps doctors plan better.
“The seasonal pattern of viral pharyngitis highlights the need for targeted public health interventions during peak seasons.”
Things that increase your chance of getting it include being close to someone who’s sick, not washing your hands well, and having health issues. These can weaken your immune system.
By knowing these facts, we can fight acute pharyngitis better. This helps reduce its effect on healthcare and improves patient care.
Acute Pharyngitis Viral Etiology
It’s important to know the viral causes of acute pharyngitis to treat it well. Viruses are a big reason for this illness. Finding out which virus is causing it helps us know how to treat it.
Common Viral Causes
Many viruses can cause acute pharyngitis. Here are some of them:
- Rhinovirus: This virus is often behind the common cold and can also cause pharyngitis.
- Influenza: Influenza viruses can lead to severe pharyngitis, more so during flu seasons.
- Adenovirus: Adenovirus infections can cause many respiratory problems, including pharyngitis.
- Coronavirus: Coronaviruses, like SARS-CoV-2, can cause pharyngitis and other respiratory issues.
- Parainfluenza: Parainfluenza viruses are common causes of respiratory infections, including pharyngitis.
These viruses can cause a range of symptoms. They can be from mild to very painful. They can really affect someone’s life quality.
Viral Pathogen | Common Symptoms | Seasonality |
Rhinovirus | Mild pharyngitis, runny nose | Year-round, peaks in spring and fall |
Influenza | Severe pharyngitis, fever, body aches | Typically winter months |
Adenovirus | Pharyngitis, conjunctivitis, fever | Year-round, outbreaks in close quarters |
Coronavirus | Pharyngitis, cough, shortness of breath | Year-round, varies with outbreaks |
Parainfluenza | Pharyngitis, croup in children | Typically late summer to fall |
Knowing which viruses cause acute pharyngitis is key for treatment. It also helps in preventing the illness. We will look more into this in the next sections.
Pathophysiology of Viral Pharyngitis
Viral pharyngitis happens when viruses infect the oropharynx. This leads to symptoms like sore throat. Knowing how this works helps us find better ways to treat it.
Viral Invasion Mechanisms
Viral pharyngitis starts when viruses enter the oropharynx’s mucosal cells. Rhinovirus, coronavirus, and adenovirus are common culprits. They use cell surface receptors to take over the host cells.
These viruses can spread through close contact or in the air. Once inside, they multiply, releasing more viruses to infect more cells.
Mucosal Cell Damage and Inflammation
As viruses multiply, they damage mucosal cells. This leads to cell death and the release of inflammatory cytokines. The oropharyngeal mucosa becomes inflamed, showing signs of redness, swelling, and pain.
The inflammation is part of the body’s fight against the virus. But it also causes symptoms like a sore throat and trouble swallowing.
Host Immune Response to Viral Infection
The immune system is key in fighting viral pharyngitis. Both innate and adaptive immunity play roles. The innate immune system acts quickly, producing interferons and activating natural killer cells.
The adaptive immune system, with T cells and B cells, is vital for clearing the virus. Adequate immune response helps control the illness. A weak response can lead to worse symptoms or complications.
In summary, viral pharyngitis is a complex battle between viruses and the immune system. Understanding this is essential for creating effective treatments.
Bacterial Pharyngitis: Causes and Prevalence
It’s important to know what causes bacterial pharyngitis to treat it well. This type of pharyngitis is a big part of the cases in kids and teens.
Group A Streptococcus (GAS) as Primary Cause
Group A Streptococcus (GAS) is the main cause of bacterial pharyngitis. GAS pharyngitis hits school-aged kids and teens the hardest. It’s key to treat GAS infections right to avoid serious problems like rheumatic fever.
GAS infections stick to the throat thanks to special proteins. These proteins help the bacteria stay in the throat and avoid being caught by the immune system.
Other Bacterial Pathogens
While GAS is the main culprit, other bacteria can also cause throat infections. These include:
- Arcanobacterium haemolyticum, seen more in young adults
- Neisseria gonorrhoeae, common in sexually active people
- Mycoplasma pneumoniae and Chlamydia pneumoniae, linked to unusual cases
Epidemiological Distribution
The spread of bacterial pharyngitis changes with age, where you live, and your social status. GAS pharyngitis is more common in crowded places and during late winter or early spring.
Knowing how and where bacterial pharyngitis spreads helps doctors make better choices. They need to think about the local spread of GAS and other bacteria when treating throat infections.
Pathogenic Mechanisms of Bacterial Pharyngitis
Bacterial pharyngitis is caused by a mix of virulence factors. These factors help bacteria stick to and invade host tissues. Group A Streptococcus (GAS) is the main culprit behind this infection. Its ways of causing harm are complex.
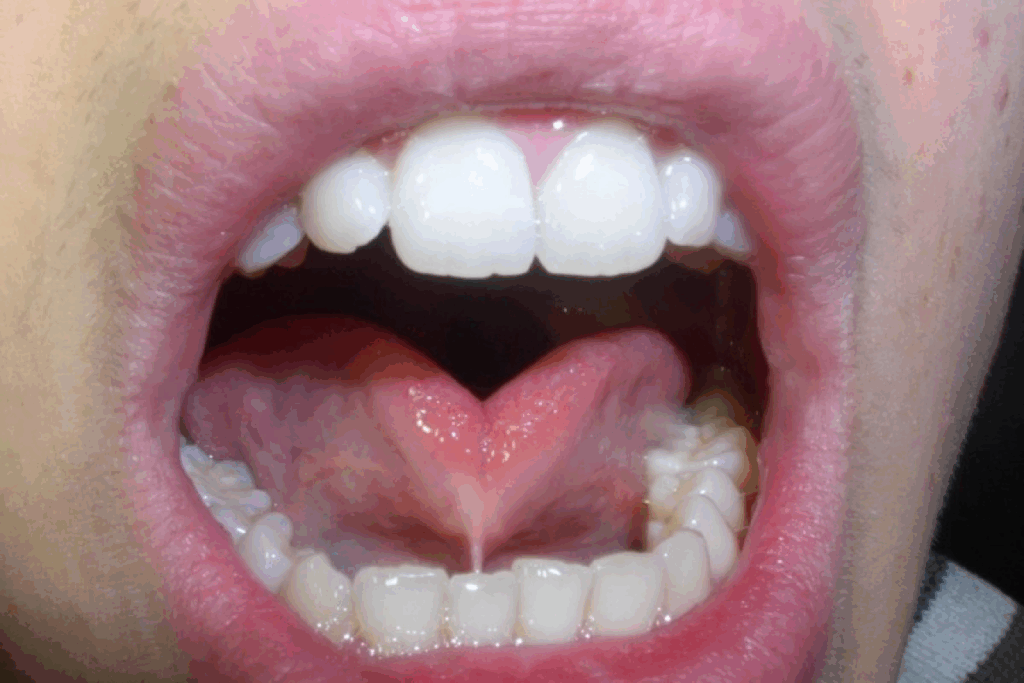
M Protein Attachment
The M protein is a key virulence factor of GAS. It helps the bacteria stick to host cells. This protein inhibits phagocytosis by binding to host fibrinogen. This keeps the bacteria safe from being destroyed by host immune cells.
Lipoteichoic Acid Interactions
Lipoteichoic acid (LTA) is vital for GAS to stick to host cells. It binds to host cell receptors, helping GAS colonize the pharynx. This is key for starting an infection.
Hyaluronic Acid Capsule Formation
The hyaluronic acid capsule is a big deal for GAS. It helps the bacteria avoid the host’s immune response. The capsule is anti-phagocytic, stopping host immune cells from attacking the bacteria. This lets GAS stay in the host and cause infection.
Bacterial Toxin Production
GAS makes toxins that help it cause harm. These include streptolysins, which break down red blood cells and other host cells. Also, pyrogenic exotoxins can cause fever and other symptoms. The toxins play a big role in how severe GAS infections are.
In summary, bacterial pharyngitis, mainly caused by GAS, involves many virulence factors. Knowing how these factors work is key to fighting this common infection.
Clinical Differentiation Between Viral and Bacterial Pharyngitis
It’s important to know if pharyngitis is caused by a virus or bacteria. This helps us choose the right treatment. We need to look at the signs of each to give the best care.
Characteristic Features of Viral Pharyngitis
Viral pharyngitis has its own set of symptoms. These can help us tell it apart from bacterial pharyngitis. Common signs include:
- Cough
- Rhinorrhea
- Hoarseness
- Mild sore throat
These symptoms often come with other signs of a cold or flu. The presence of cough and rhinorrhea is a strong sign of a virus.
Hallmarks of Bacterial Pharyngitis
Bacterial pharyngitis, like that from Group A Streptococcus (GAS), has more serious symptoms. Key signs are:
- Sudden sore throat
- High fever
- Tender cervical lymphadenopathy
- Exudative tonsillitis
A study found, “GAS pharyngitis often has a more severe presentation. This includes high fever and exudative tonsillitis”
“GAS pharyngitis can be quite distinct. Patients often have severe sore throat and fever.”
Clinical Features | Viral Pharyngitis | Bacterial Pharyngitis |
Cough | Common | Rare |
Rhinorrhea | Common | Rare |
Fever | Mild | High |
Tonsillar Exudate | Less common | Common |
Limitations of Clinical Assessment
While symptoms can guide us, they’re not always clear-cut. The symptoms of viral and bacterial pharyngitis can overlap. This makes it hard to tell them apart. We often need tests to confirm the cause and choose the right treatment.
We use a mix of clinical judgment and tests to diagnose and treat pharyngitis.
Diagnostic Approaches and Testing
Diagnosing pharyngitis involves both clinical checks and tests. We use different methods to find out if it’s caused by a virus or bacteria. This is important because it affects how we treat it.
Centor Criteria and Modified Centor Score
The Centor criteria and modified Centor score help figure out if you might have a bacterial infection. They look at things like tonsillar exudates, swollen lymph nodes, fever, and if you have a cough. Doctors use these signs to guess if you have a bacterial infection and decide what to do next.
Rapid Antigen Detection Tests
Rapid Antigen Detection Tests (RADT) are used to find bacterial infections quickly. They give results fast, usually in minutes. But, they’re not always right, so sometimes a throat culture is needed to confirm.
Throat Culture
Throat culture is the most reliable test for bacterial infections. It takes a swab from your tonsils and throat. It’s more accurate than RADT but takes longer, usually 24 to 48 hours. This delay can slow down treatment but ensures a correct diagnosis.
Molecular Diagnostic Methods
Molecular tests like PCR are becoming key in diagnosing pharyngitis. They’re very accurate and can give results in a few hours. These tests can also find other pathogens, helping doctors choose the right treatment.
By using clinical checks and these tests together, we can find out what’s causing your pharyngitis. The right test depends on your symptoms, risk factors, and how fast you need results.
Treatment Strategies for Viral vs. Bacterial Pharyngitis
Knowing why someone has pharyngitis is key to picking the right treatment. It’s not just about knowing the cause. It affects how we treat the patient and their outcome.
Management of Viral Pharyngitis
Viral pharyngitis is treated with supportive care. This includes:
- Hydration: Drinking enough water to avoid dehydration.
- Rest: Resting to help the body heal.
- Over-the-counter pain relievers: Using drugs like acetaminophen or ibuprofen to ease pain and lower fever.
- Throat lozenges or gargling with salt water: To ease throat pain.
Antiviral drugs are not usually needed for viral pharyngitis. They are only used for certain viruses like herpes simplex virus.
Antibiotic Therapy for Bacterial Pharyngitis
Bacterial pharyngitis, like that from Group A Streptococcus (GAS), needs antibiotics. Antibiotics aim to:
- Shorten and lessen symptoms.
- Stop serious problems like ear infections or abscesses.
- Stop GAS from spreading to others.
- Prevent rheumatic fever, a serious condition from untreated GAS infections.
Penicillin or amoxicillin are usually the first choice for GAS pharyngitis. If someone can’t take penicillin, doctors might use azithromycin or clarithromycin instead.
Consequences of Inappropriate Antibiotic Use
Using antibiotics too much or wrongly can cause big problems. These include:
- Antibiotic resistance, making infections harder to treat.
- Side effects, from mild stomach issues to severe allergic reactions.
- Changes in the patient’s microbiome, leading to more health problems.
So, it’s vital to follow antibiotic guidelines. It’s also important to teach patients about the dangers of not finishing antibiotics and the risks of misuse.
Special Considerations for Different Populations
Understanding the needs of different patient groups is key to treating acute pharyngitis. While the basics of diagnosis and treatment are the same, some groups need special care. This is because of their unique characteristics and risks.
Pediatric Patients
Children are often hit hard by acute pharyngitis, with Group A Streptococcus (GAS) being a big culprit. Pediatric patients need careful checks to tell if it’s a virus or bacteria. This is because bacteria might need antibiotics.
We also have to watch out for complications like ear infections and abscesses in kids. The Centor criteria help doctors figure out if a child has GAS pharyngitis. Treatment choices are based on how the child looks, rapid tests, and sometimes a throat culture.
Elderly and Immunocompromised Individuals
The elderly and those with weak immune systems face special challenges with acute pharyngitis. They might get sicker and face more serious problems because their immune system isn’t strong. Health issues like diabetes and COPD can make things worse.
When treating these groups, we have to think about the risk of other infections. Keeping a close eye on them is key to catch and treat any problems early.
Recurrent Pharyngitis Management
Dealing with recurrent pharyngitis is tough. It needs a detailed plan to find the cause and prevent it. Possible reasons include always having GAS, GERD, and allergies. We also look at how the environment and lifestyle play a part.
For recurrent cases, preventive antibiotics might be used in some cases. Fixing any underlying issues is also important. Teaching patients how to manage symptoms and prevent future episodes is vital.
Conclusion: The Importance of Accurate Diagnosis
Getting a correct diagnosis is key. It helps tell apart viral and bacterial pharyngitis. This guides the right treatment and stops bad outcomes.
Knowing the causes and signs of these illnesses helps doctors make better choices. This leads to better care for patients.
Accurate diagnosis is very important. It affects how well treatment works and how fast patients get better. As healthcare workers, we must focus on getting the diagnosis right. This ensures we give the best care possible.
FAQ
What is the difference between viral and bacterial pharyngitis?
Viral pharyngitis is caused by viruses like rhinovirus and influenza. Bacterial pharyngitis is usually caused by Group A Streptococcus (GAS). Knowing the cause is key for the right treatment.
What are the common symptoms of acute pharyngitis?
Symptoms include a sore throat, pain when swallowing, and fever. Swollen lymph nodes are also common. Cough and rhinorrhea often point to viral infections. High fever and tender lymph nodes suggest bacterial infections.
How is the cause of pharyngitis diagnosed?
Doctors use a combination of clinical checks and tests. These include the Centor criteria, Rapid Antigen Detection Tests (RADT), throat culture, and molecular diagnostics.
What is the treatment for viral pharyngitis?
For viral pharyngitis, treatment focuses on hydration and pain relief. Antibiotics won’t help because they target bacteria, not viruses.
Why is accurate diagnosis of pharyngitis important?
Accurate diagnosis helps avoid unnecessary antibiotics. It also reduces complications and improves patient care.
What are the possible complications of untreated bacterial pharyngitis?
Untreated bacterial pharyngitis, like GAS, can cause serious issues. One risk is rheumatic fever.
How does the pathophysiology of viral pharyngitis occur?
Viral pharyngitis happens when viruses attack the oropharynx’s mucosal cells. This causes cell damage and an inflammatory response.
Are there special considerations for diagnosing and treating pharyngitis in different populations?
Yes, kids are more at risk for GAS pharyngitis and its complications. Older and immunocompromised people may need different treatments due to their unique health challenges.
What is the role of the host immune response in viral pharyngitis?
The immune system, including innate and adaptive immunity, is vital in fighting viral pharyngitis. It determines the infection’s outcome.
How does bacterial pharyngitis, like GAS, evade the host immune response?
GAS uses several tricks to avoid the immune system. It expresses M protein, interacts with lipoteichoic acid, and produces a hyaluronic acid capsule.
What are the consequences of inappropriate antibiotic use in pharyngitis?
Using antibiotics when not needed can lead to antibiotic resistance. It also causes unnecessary side effects.
What is the epidemiology of acute pharyngitis?
Acute pharyngitis is a big reason for doctor visits. Viral infections are the main cause, with a spike in winter and early spring.
How is bacterial pharyngitis treated?
Bacterial pharyngitis, like GAS, needs antibiotics. This is to prevent complications and stop the spread of the infection.
What are the limitations of clinical assessment in diagnosing pharyngitis?
Relying only on clinical assessment has its limits. Tests are often needed to confirm the cause of pharyngitis.
References
National Center for Biotechnology Information. (2025). Is Acute Pharyngitis Viral or Bacterial Key Differences. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559007/










