Last Updated on October 31, 2025 by
Knowing about carcinoma in situ is key to catching cancer early. Carcinoma in situ (CIS) is a group of abnormal cells that stay in one place. They haven’t spread to other tissues, making it stage 0 cancer.
CIS is very important in cancer diagnosis. It gives us a chance to act early. At this stage, cancer hasn’t invaded nearby tissues. This makes it very treatable.
When we understand CA in situ, we can stop cancer from getting worse. Finding CIS early is important. With the right treatment, we can manage it well.
Carcinoma in situ is a key stage in cancer where abnormal cells stay in their original spot. To get it, we must explore its roots, medical meaning, and why it’s seen as precancerous.
The term “in situ” comes from Latin, meaning “in its original place.” This is key to understanding carcinoma in situ. It shows the cancer cells haven’t spread to other areas. This term is used in many medical fields to describe tumors that stay in one place.
Carcinoma in situ is a cancer that only exists in the cells where it began. It hasn’t spread to nearby tissues. This is an early stage, often called stage 0 cancer. It’s a critical time when treatment can greatly change the disease’s path.
Cells in carcinoma in situ are precancerous because they could turn into invasive cancer if not treated. They haven’t spread but can get worse. Their main trait is staying in the original spot, showing they’re in an early cancer stage.
| Term | Definition | Implication |
| In Situ | Latin for “in its original place” | Indicates localized cancer cells |
| Carcinoma In Situ | Cancer that has not spread from its original location | Precancerous condition, possible invasive cancer |
| Precancerous Cells | Abnormal cells that could become cancerous | Need watching and possibly treatment to stop cancer growth |
Exploring carcinoma in situ shows us the detailed changes at the cell level. This condition, known as CA in situ, has abnormal cells but they haven’t spread. Knowing what is ca in situ is key for catching it early and treating it.
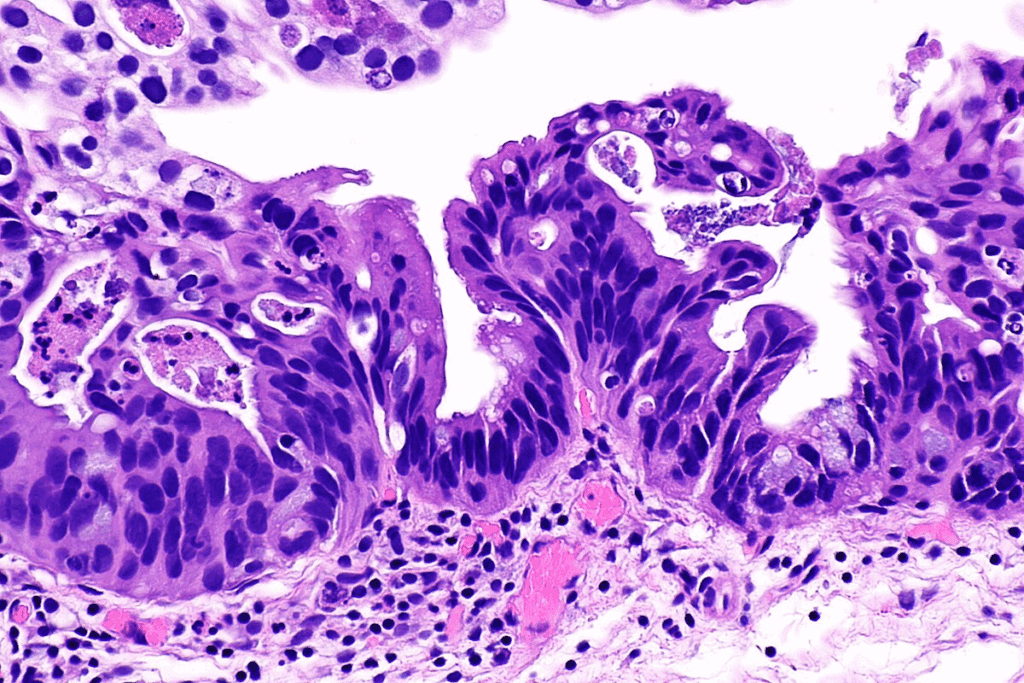
In CA in situ, cells change a lot. They look different, grow faster, and have genetic issues. Even though they look like cancer cells, they’re not invasive.
Normal cells divide in a controlled way. Precancerous cells, like those in CA in situ, grow out of control. Cancer cells have spread and can move to other parts of the body. Knowing the difference helps doctors treat cancer carcinoma in situ right.
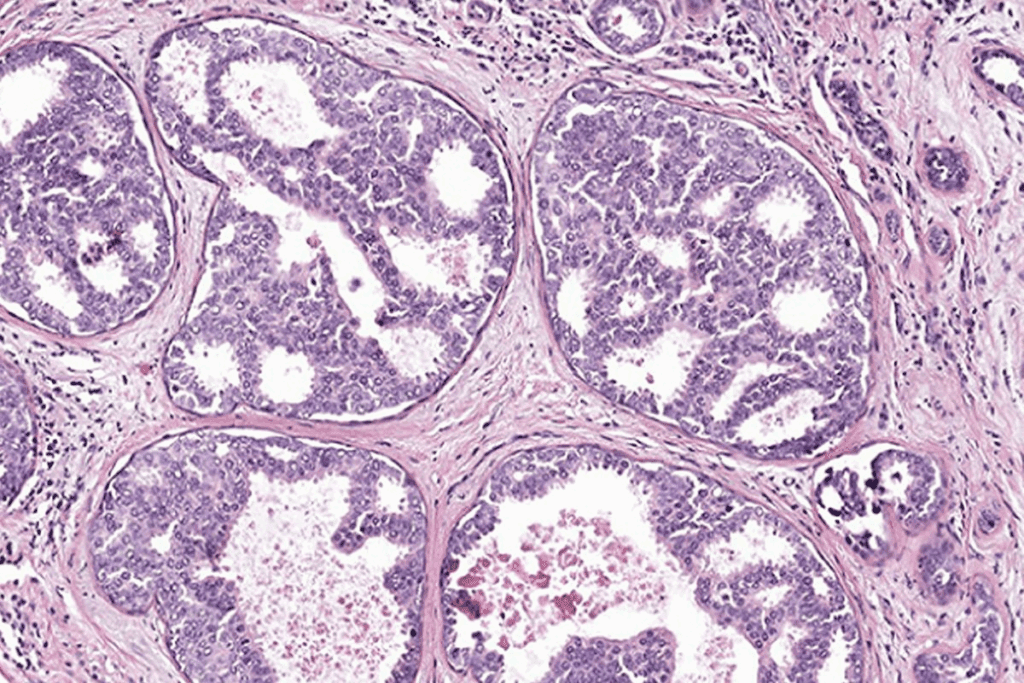
Looking at cells under a microscope is key to spotting CA in situ. Doctors search for signs like unusual nuclei and cell shapes. Finding these signs helps tell CA in situ apart from normal cells and cancer. This is important for choosing the right treatment and understanding carcinoma situ meaning.
Learning about carcinoma in situ helps us see why catching it early is so important. This knowledge lets doctors give better treatments, helping patients get better.
CA in situ, also known as stage 0 cancer, is a key point in cancer growth. At this stage, cancer cells are present but haven’t spread to nearby tissues. This makes it a non-invasive condition.
The cancer staging system helps describe how far cancer has spread. It goes from stage 0 to stage 4. Stage 0 is non-invasive, and stages 1 to 4 are more invasive. Knowing this system is key to finding the right treatment.
CA in situ is called stage 0 because cancer cells stay in their original place. They haven’t spread to nearby tissues. This is important because it shows the cancer is in its earliest stage and hasn’t become invasive.
Finding CA in situ early is vital for good treatment and stopping cancer from spreading. Regular checks can spot cancer early, leading to quick action. The main benefits of early detection are:
Understanding CA in situ as stage 0 cancer highlights the need for early detection. Regular screenings and knowing cancer risk factors are key to staying healthy and stopping cancer from getting worse.
It’s important for patients and doctors to know about CA in situ. This includes different conditions that are not yet cancer but could become it. These conditions have abnormal cells that haven’t spread to other tissues.
DCIS is a common type of in situ carcinoma in women. It makes up 20-25 percent of all new breast cancer cases. It starts in the milk ducts but hasn’t spread to other parts of the breast.
Because the abnormal cells are only in the ducts, it’s called non-invasive or pre-invasive cancer. This means it hasn’t invaded the surrounding breast tissue.
Cervical carcinoma in situ, or CIN, is when abnormal cells are found on the cervix but haven’t invaded. It’s often found during regular Pap smear screenings. If not treated, it could turn into invasive cervical cancer.
Squamous cell carcinoma in situ affects squamous cells that are only in the top layer of tissue. It can happen in the skin, esophagus, and cervix. Finding it early is key to stopping it from becoming invasive squamous cell carcinoma.
There are other in situ carcinomas like lobular carcinoma in situ (LCIS) in the breast. LCIS is not a true cancer but shows a higher risk of breast cancer. In situ carcinomas can also happen in the bladder, lung, and gastrointestinal tract. Each has its own features and treatment plans.
Knowing about these types of CA in situ is vital for the right treatment. Early detection and action can greatly help patients.
Diagnosing carcinoma in situ early is key to stopping cancer before it spreads. We’ll look at how doctors find this condition and why it’s so important to catch it early.
Screening for carcinoma in situ uses different methods based on where and what type of cancer it is. For example, mammograms often find ductal carcinoma in situ (DCIS). It’s a good idea for people at high risk or over a certain age to get screened regularly.
Screening works by finding problems before symptoms show up. For DCIS, mammograms can spot tiny signs that can’t be felt during a check-up.
When a screening finds something suspicious, a biopsy is usually done to confirm the diagnosis. The biopsy sample is then checked by a pathologist to see if the cells are abnormal or cancerous.
A biopsy is key because it gives a clear diagnosis. Pathologists look for signs of carcinoma in situ, like abnormal cell growth that stays in the epithelial layer.
Imaging is also important in finding carcinoma in situ. Mammograms are just the start. Ultrasound and MRI are used too, mainly when mammograms aren’t clear or to see how big the disease is.
These tools help find out how big and where the lesions are. This info is vital for planning treatment.
Even with better screening and diagnosis, finding carcinoma in situ can be tough. There’s a chance of finding and treating something that might not turn into real cancer, like with DCIS.
Studies show about 40 percent of DCIS lesions could become invasive cancer without treatment. So, getting a correct diagnosis and knowing the risk of it becoming invasive is very important.
| Diagnostic Method | Description | Use in CA In Situ Diagnosis |
| Mammography | Imaging technique using low-energy X-rays | Primary method for detecting DCIS |
| Biopsy | Removal of tissue for pathological examination | Confirms diagnosis of CA in situ |
| Ultrasound | Imaging using high-frequency sound waves | Assesses extent and characteristics of lesions |
Several factors can increase the risk of getting carcinoma in situ. These include genetics, lifestyle, and the environment. Knowing these factors is key to catching it early and preventing it.
Genetics play a big role in getting carcinoma in situ. If your family has a history of cancer, you might be at higher risk. Certain genes, like BRCA1 and BRCA2, can raise the risk of breast and ovarian cancers, including DCIS.
Lifestyle and environment also affect your risk. Some chemicals and radiation can increase cancer risk. For example, long-term exposure to pesticides and heavy metals can raise the risk of many cancers.
Age and gender are also important. The risk of many cancers, including in situ carcinomas, goes up with age. Some cancers, like breast cancer in women and prostate cancer in men, are more common in certain genders.
Having had cancer before can raise your risk of getting carcinoma in situ. For instance, having LCIS can increase your risk of invasive breast cancer. Studies show a risk of about 25% to 30%.
Knowing these risk factors can help you take steps to prevent carcinoma in situ. Regular screenings can also help lower the risk of it turning into invasive cancer.
Carcinoma in situ treatment involves several methods to stop it from becoming invasive cancer. We’ll look at the different treatments, their uses, and benefits.
Surgery is a key treatment for carcinoma in situ, aiming to remove the precancerous cells. Lumpectomy, or breast-conserving surgery, is common for ductal carcinoma in situ (DCIS). It removes just the affected part of the breast. Sometimes, a mastectomy is needed if the DCIS is widespread.
For cervical carcinoma in situ, treatments like loop electrosurgical excision procedure (LEEP) or cold knife cone biopsy are used. The choice depends on the carcinoma’s extent and location.
After lumpectomy, radiation therapy is used to kill any remaining cancer cells. External beam radiation therapy is the most common method. It uses high-energy beams from outside the body.
Whether to use radiation therapy depends on the DCIS’s size, grade, and the patient’s health and preferences.
For hormone receptor-positive carcinoma in situ, hormone therapy is recommended. It aims to block the body’s natural hormones to prevent invasive cancer.
Tamoxifen is a hormone therapy drug often used for DCIS. It helps lower the risk of recurrence and new cancers in the breast.
In some cases, a watchful waiting or active surveillance approach is used. This is for patients with low-risk carcinoma in situ or those not suited for aggressive treatments.
This method involves regular mammograms and clinical exams. It ensures the carcinoma in situ doesn’t turn into invasive cancer.
It’s key to know how cancer can grow from in situ to invasive. In situ cancer means cancer cells are there but haven’t spread. If not treated, these cells can turn into invasive cancer.
About 40 percent of ductal carcinoma in situ (DCIS) can turn into invasive cancer without treatment. This is a big risk. Knowing this helps both patients and doctors.
Women with lobular carcinoma in situ face a 25% to 30% chance of getting breast cancer. These numbers show why watching and preventing are so important.
Many things can change how likely cancer is to grow. These include:
Keeping an eye on in situ cancer is key to catch invasive cancer early. This might mean:
Understanding the risks and factors helps doctors give better care. This can lead to better results for patients.
To prevent carcinoma in situ, we need a full plan. This includes regular check-ups and making healthy lifestyle choices. These steps can greatly lower the chance of getting invasive cancer.
Screening often is key to catching carcinoma in situ early. We suggest sticking to the recommended screening plans. This helps spot precancerous growths before they turn into cancer.
Changing our lifestyle can also help a lot. Eating well, staying active, and staying away from harmful substances are important. These actions can help lower the risk of CA in situ.
For those at high risk, doctors might suggest certain medicines. These can help prevent cancer from getting worse.
People with a family history or genetic risk should talk to a genetic counselor. They can offer important advice on how to prevent cancer.
| Strategy | Description | Benefit |
| Regular Screening | Following established screening guidelines | Early detection of CA in situ |
| Lifestyle Modifications | Healthy diet, regular exercise, avoiding carcinogens | Reduced risk of CA in situ |
| Preventive Medications | Medications for high-risk individuals | Reduced risk of cancer progression |
Understanding carcinoma in situ is key to stopping cancer from spreading. We’ve looked at what it is, how it’s found, and how it’s treated. CA in situ is a critical point where catching it early can change the disease’s course.
Most people with ductal carcinoma in situ (DCIS) are alive 20 years later. This shows how vital early detection and treatment are. We’ve talked about the role of regular checks, healthy living, and medicines in lowering CA in situ risk.
In summary, CA in situ is a serious issue that needs a full approach to handling. Knowing the risks, how to find it, and treatment choices helps prevent cancer from getting worse. As we learn more about CA in situ, it’s clear that catching it early is key to better patient results.
CA in situ, or carcinoma in situ, is when cancer cells are present but haven’t spread. It’s an early stage of cancer, often called stage 0.
CA in situ is when cancer cells stay in one place. Invasive cancer spreads to other tissues and parts of the body.
Doctors use tests like mammograms or Pap smears to find CA in situ. Then, a biopsy and exam confirm if there are cancer cells.
Treatments for CA in situ include surgery, radiation, medicine, hormone therapy, or watching it closely. The choice depends on the type, location, and the patient’s health.
Yes, CA in situ can turn into invasive cancer if not treated. The chance of this happening depends on the type and the person’s health.
Factors that increase the risk of CA in situ include genetics, lifestyle, age, gender, and having had cancer before.
To lower the risk, get regular screenings, make healthy lifestyle choices, take preventive medicines, and get genetic counseling if needed.
Ductal carcinoma in situ (DCIS) is a type of CA in situ in the breast’s milk ducts. It’s not invasive but can turn into invasive cancer if not treated.
Yes, CA in situ is an early stage of cancer, often stage 0. It’s not invasive but can become invasive if not treated.
Finding CA in situ early is key. It lets doctors treat it quickly, reducing the chance of it becoming invasive and improving treatment results.
Carcinoma in situ means cancer cells are in the top layer of cells but haven’t spread. It’s a condition that needs watching and might need treatment.
The cancer staging system shows how far cancer has spread. CA in situ is stage 0, meaning it’s not invasive.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!