Orthopedic surgery is complex and needs a deep understanding of key principles. Successful operations rely on four key elements: Anatomy, Alignment, Asepsis, and Anesthesia.
These principles work together to ensure the best results for patients. Knowing Anatomy is key for surgeons to understand the human body’s complexities. Proper Alignment is also vital, as it directly impacts the success of the surgery.
By mastering these principles, surgeons can significantly improve patient care and achieve better results in orthopedic surgical practice.
Key Takeaways
- Understanding the 4 A’s is key for successful orthopedic surgery.
- Anatomy, Alignment, Asepsis, and Anesthesia are fundamental principles.
- These principles guide surgeons in performing complex operations.
- Mastering the 4 A’s improves patient care and outcomes.
- The 4 A’s are essential for achieving optimal results in orthopedic surgical practice.
The Fundamental Principles of Orthopedic Surgery
The Fundamental Principles of Orthopedic Surgery
Orthopedic surgery is built on key principles that have grown a lot over time. These principles are the foundation of surgery, making sure procedures are done with great care and precision.
Historical Development of Orthopedic Principles
Orthopedic surgery has a long history. Its principles have changed from ancient times to today’s evidence-based methods. The growth of orthopedic principles has been shaped by new technology, better understanding of the body, and new surgical methods.
At first, orthopedic surgery aimed to fix deformities and treat injuries. Now, it covers a wide range of surgeries, from joint replacements to complex spinal operations.
Importance of Standardized Approaches in Surgical Practice
Standardized methods in orthopedic surgery are key for consistent and high-quality care. Following established orthopedic guidelines and surgical techniques helps reduce risks and better outcomes. Standardization also helps share knowledge and best practices, moving the field forward.
The role of these principles is huge, affecting the success of surgeries and patient recovery. As orthopedic surgery keeps growing, sticking to these basic principles is vital for good practice.
The 4 A’s of Orthopedic Surgery: An Overview
Knowing the 4 A’s is key for orthopedic surgeons to provide top-notch care. The 4 A’s – Anatomy, Alignment, Asepsis, and Anesthesia – are a complete guide for orthopedic surgery.
Origin and Evolution of the 4 A’s Framework
The 4 A’s started with basic surgery principles. Over time, it grew to meet orthopedic surgery’s needs. It now includes new tech, better patient care, and advanced surgical methods.
The 4 A’s have evolved with orthopedic surgery. This includes better understanding of anatomy, improved alignment, better aseptic practices, and advanced anesthesia.
Why These Principles Guide Modern Orthopedic Practice
The 4 A’s are vital in modern orthopedic care. Each “A” is key for successful surgeries.
| The 4 A’s | Description | Importance in Orthopedic Surgery |
| Anatomy | Understanding of human body structure | Crucial for precise surgical planning and execution |
| Alignment | Proper positioning of bones and joints | Essential for restoring function and reducing pain |
| Asepsis | Maintenance of sterile conditions | Vital for preventing surgical site infections |
| Anesthesia | Management of pain during surgery | Necessary for patient comfort and procedural success |
Using the 4 A’s in orthopedic care has greatly improved results. It’s a key part of modern orthopedic surgery.
Anatomy: The First A of Orthopedic Surgery
Anatomy is key in orthopedic surgery. It acts as a guide for surgeons in complex procedures. Knowing human anatomy well is vital for orthopedic surgeons to treat musculoskeletal issues effectively.
Importance of Anatomical Knowledge in Orthopedics
Anatomical knowledge is essential in orthopedics. It helps surgeons understand the complex relationships in the musculoskeletal system. This knowledge is vital for planning and performing surgeries.
“A detailed knowledge of anatomy is essential for surgeons to navigate the complexities of orthopedic surgery and achieve optimal outcomes.”
— Orthopedic Surgery Principles
Anatomical knowledge is important in several ways in orthopedics:
- Accurate diagnosis of musculoskeletal conditions
- Effective surgical planning and execution
- Minimization of complications during and after surgery
Critical Anatomical Considerations for Surgical Planning
When planning orthopedic surgeries, surgeons must consider several key anatomical factors. These are important for success:
| Anatomical Consideration | Importance in Surgical Planning |
| Understanding of bone structure and density | Crucial for selecting appropriate implants and fixation methods |
| Knowledge of soft tissue anatomy | Essential for preserving tissue integrity and function during surgery |
| Awareness of neurovascular structures | Vital for avoiding nerve and vessel damage during surgical procedures |
By carefully considering these anatomical factors, surgeons can greatly improve surgery outcomes.
Mastering Musculoskeletal Anatomy for Surgical Success
Understanding musculoskeletal anatomy is key to successful orthopedic surgeries. Knowing the complex structures in the musculoskeletal system helps surgeons. They can then perform various orthopedic procedures with great detail.
Regional Anatomy Relevant to Common Orthopedic Procedures
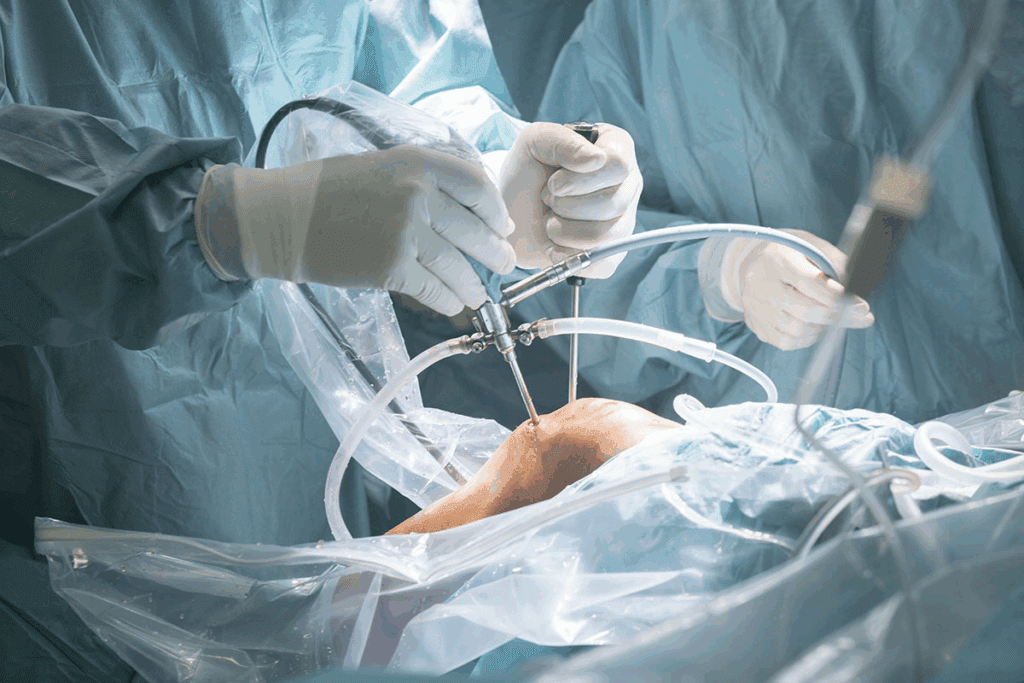
Regional anatomy is vital in orthopedic surgery. Each procedure needs specific knowledge of certain areas. For example, knee or shoulder surgeries require a deep understanding of bones, ligaments, tendons, and muscles.
Accurate anatomical knowledge helps surgeons spot risks and improve results. This knowledge is essential for success in these surgeries.
Anatomical Variations and Their Surgical Implications
Anatomical variations can greatly affect surgery planning and execution. Surgeons must know these variations to adjust their methods. For instance, nerve paths or extra muscles can change how a surgery is done.
Preoperative imaging and detailed patient anatomy reviews are key. They help identify variations and plan the best surgery approach.
By mastering musculoskeletal anatomy and understanding regional variations, surgeons can improve their skills. This knowledge is vital for better patient outcomes. It shows the importance of ongoing education and training in orthopedic surgery.
Alignment: The Second A of Orthopedic Surgery
Alignment is key in orthopedic surgery. It affects both short-term and long-term results. Getting bones and joints right after surgery is essential for their proper function.
Principles of Proper Bone and Joint Alignment
Aligning bones and joints right is vital. It helps restore normal function and lowers the risk of problems. The main principles include:
- Restoring the normal anatomical axis of the bone or joint
- Ensuring proper rotational alignment to prevent abnormal wear or stress
- Achieving optimal congruence between articulating surfaces
To achieve this, surgeons use preoperative planning, intraoperative techniques, and postoperative checks. They employ different methods to check and confirm alignment, such as:
Assessment Methods for Determining Optimal Alignment
Checking alignment before and after surgery is critical. Several methods help determine the best alignment, including:
| Method | Description | Application |
| Radiographic Analysis | Use of X-rays to assess bone and joint alignment | Preoperative planning and postoperative evaluation |
| Intraoperative Navigation | Real-time tracking of bone and implant positions during surgery | Enhancing accuracy of alignment during surgery |
| Clinical Assessment | Physical examination to evaluate alignment and function | Postoperative evaluation of patient outcomes |
By using these methods and understanding alignment principles, surgeons can improve results. The aim is to ensure alignment supports optimal function, reduces wear, and promotes long-term health.
Alignment Techniques in Different Orthopedic Procedures
Alignment is key in orthopedic surgery. It varies with each procedure. The way bones, joints, or the spine are aligned greatly affects the surgery’s success. This, in turn, impacts the patient’s recovery and how well they function after surgery.
Fracture Reduction and Fixation Alignment
In fracture surgery, getting bones back in place is vital. Techniques like open reduction and internal fixation (ORIF) need careful planning and execution. Imaging tools like fluoroscopy help surgeons check alignment in real-time during surgery.
Joint Replacement Alignment Considerations
For joint replacements, like hips or knees, alignment is key for the implant’s success. Proper alignment spreads stress evenly, reducing wear on the implant. Surgeons use computer-assisted navigation to get the best alignment.
Spinal Alignment Principles
Spinal surgeries, like fusions or disc replacements, need precise alignment. Techniques like pedicle screw placement and spinal rods are used. Detailed imaging before surgery is essential for successful spinal alignment.
| Procedure | Alignment Technique | Importance |
| Fracture Fixation | ORIF, External Fixation | Restores bone anatomy, promotes healing |
| Joint Replacement | Computer-assisted navigation, Manual alignment | Ensures even stress distribution, longevity of implant |
| Spinal Surgery | Pedicle screw placement, Spinal rods | Maintains/restores natural spinal curvature |
Different orthopedic procedures need their own alignment techniques. Success depends on planning before surgery, precision during it, and care after. This ensures the best results for patients.
Asepsis: The Third A of Orthopedic Surgery
Maintaining asepsis is key to stopping surgical site infections in orthopedic surgeries. Asepsis means keeping the surgery area clean of harmful germs. This helps lower the chance of infections after surgery.
Asepsis is very important in orthopedic surgery. These surgeries often involve putting in implants or fixing bones and tissues. Following strict aseptic techniques is vital to avoid infections.
Infection Prevention Protocols in Orthopedic Surgery
Orthopedic surgery has many ways to prevent infections. It starts with screening patients before surgery to find those at risk. It also includes using sterile tools and cleaning solutions during the surgery.
| Protocol Component | Description | Importance |
| Pre-operative Screening | Identifying patients at risk of infection | High |
| Sterile Equipment | Using equipment sterilized to prevent microbial contamination | Critical |
| Antiseptic Solutions | Applying solutions to reduce microbial load on the skin | High |
Consequences of Compromised Asepsis in Orthopedic Procedures
Not following asepsis can cause surgical site infections (SSIs). SSIs can lead to serious problems, like longer hospital stays and more surgeries. They can also cause long-term disabilities.
The risks of SSIs show how critical it is to keep aseptic practices strict in orthopedic surgery. By knowing and using good infection prevention methods, doctors can greatly lower the risk of these problems.
Modern Aseptic Techniques and Technologies
Modern aseptic techniques and technologies have changed orthopedic surgery a lot. They have greatly reduced the chance of infections after surgery. These new methods have made surgeries safer and better for patients.
Advances in Sterilization Methods
New sterilization methods are more advanced. They use hydrogen peroxide gas plasma and vaporized hydrogen peroxide. These methods are better at killing germs on surgical tools.
Sterilization Techniques Comparison
| Sterilization Method | Efficacy | Advantages |
| Autoclaving | High | Effective against bacteria and spores |
| Hydrogen Peroxide Gas Plasma | Very High | Low temperature, safe for heat-sensitive equipment |
| Vaporized Hydrogen Peroxide | Very High | Effective for room and equipment sterilization |
Operating Room Design for Optimal Asepsis
Operating rooms are now designed better for cleanliness. They use laminar airflow systems and HEPA filters. These help keep the air clean and reduce germs.
Antimicrobial Prophylaxis in Orthopedic Surgery
Preventing infections is key in orthopedic surgery. Choosing the right antibiotics depends on the surgery type and patient risks.
Good infection prevention needs teamwork. Surgeons, anesthesiologists, and infection control experts all play a role.
Anesthesia: The Fourth A of Orthopedic Surgery
Anesthesia is key in modern orthopedic surgery. It helps make complex procedures less painful for patients. Choosing the right anesthesia is very important for the success of these surgeries.
Types of Anesthesia Used in Orthopedic Procedures
Orthopedic surgery uses different types of anesthesia. These include general, regional, and local anesthesia. The choice depends on the surgery’s complexity, the patient’s health, and the surgery’s needs.
- General Anesthesia: Used for complex surgeries, making the patient unconscious and pain-free.
- Regional Anesthesia: Numbs a larger area, like the lower body for surgeries there.
- Local Anesthesia: Used for small procedures, numbing just the area being operated on.
Patient-Specific Considerations for Anesthesia Selection
Choosing the right anesthesia requires looking at each patient’s unique factors. This includes their age, medical history, and any health issues they have. For example, older patients might need different anesthesia doses because of their age and health.
| Patient Factor | Consideration for Anesthesia |
| Age | Dosage adjustments for elderly or pediatric patients |
| Medical History | Avoidance of certain anesthetics based on previous reactions or conditions |
| Comorbidities | Careful selection to avoid complications related to existing health conditions |
Choosing the right anesthesia helps control pain and improves patient comfort. It also leads to better surgical results. By matching anesthesia to each patient’s needs, surgeons can make the surgery and recovery better.
Advanced Anesthesia Approaches for Complex Orthopedic Cases
Advanced anesthesia is key for complex orthopedic surgeries. These surgeries need precision and care. Anesthesia plays a big role in making sure they are successful.
Regional Anesthesia Techniques
Regional anesthesia is becoming more popular in orthopedic surgery. It offers good pain relief with fewer side effects. Regional anesthesia numbs a specific area, reducing the need for general anesthesia.
Techniques like peripheral nerve blocks are used. They help manage pain more effectively.
Pain Management Strategies During and After Surgery
Managing pain is vital in orthopedic care. During and after surgery, a mix of strategies is used. This includes local anesthetics, NSAIDs, and opioids.
This approach improves patient comfort. It also lowers the risk of opioid side effects.
Anesthesia Challenges in Orthopedic Trauma
Orthopedic trauma cases are challenging for anesthesia. Patients with many injuries need careful management.
“The anesthetic management of orthopedic trauma patients demands a thorough understanding of their injuries, health issues, and the risk of blood loss.”
Advanced techniques, like ultrasound, help place blocks and lines safely. This improves patient results.
Integration of the 4 A’s in Clinical Practice
Using the 4 A’s is key for great results in orthopedic surgery. It makes sure every part of patient care is top-notch, from start to finish.
The 4 A’s – Anatomy, Alignment, Asepsis, and Anesthesia – are a complete guide for orthopedic doctors. They help doctors avoid problems and make patients better.
Case Examples Demonstrating the 4 A’s in Action
Let’s say a patient is getting a new hip. Anatomical knowledge helps doctors plan the surgery. Alignment is important to place the new hip right. Keeping everything clean, or asepsis, lowers infection risk. The right anesthesia makes the patient comfortable and helps the surgery go smoothly.
Interdisciplinary Collaboration to Uphold the 4 A’s
Working together is essential for the 4 A’s in practice. Doctors, anesthesiologists, nurses, and others must team up. This teamwork makes patients safer and surgery better.
Creating a team atmosphere and good communication is vital. It helps keep the 4 A’s in focus and ensures top-notch orthopedic care.
Patient Outcomes and the 4 A’s of Orthopedic Surgery
The 4 A’s in orthopedic surgery are key to success. Anatomy, Alignment, Asepsis, and Anesthesia are the basics. They directly affect how well patients do after surgery.
These principles work together to help surgeons give the best care. Knowing how each “A” helps is important for better patient results.
How Each “A” Contributes to Successful Results
- Anatomy: Knowing the body’s anatomy well is vital for planning and doing surgery. It helps surgeons spot and avoid risks.
- Alignment: Getting the alignment right is key for fixing joints and avoiding problems. It’s essential for good results in orthopedic surgery.
- Asepsis: Keeping the surgery area clean is critical to stop infections. Good infection prevention is key for patient safety.
- Anesthesia: The right anesthesia care is important for patient comfort and safety during surgery. It greatly affects patient outcomes.
Measuring Success Through the Lens of the 4 A’s
Success in orthopedic surgery is measured by how well patients do, based on the 4 A’s. Important signs like complication rates, patient happiness, and how well patients function are used. These signs show if the 4 A’s are working well in practice.
By looking at these signs, surgeons can find ways to get better. They can make their practice better to help patients more.
Training and Education in the 4 A’s for Orthopedic Surgeons
Orthopedic surgeons need a lot of education to do well in the 4 A’s. They must learn a lot to give the best care to their patients.
Residency Training Focus Areas
During residency, surgeons learn a lot about the 4 A’s: Anatomy, Alignment, Asepsis, and Anesthesia. Residency programs give them hands-on practice and important knowledge in these areas.
- Anatomy: Detailed study of musculoskeletal structures
- Alignment: Techniques for proper bone and joint alignment
- Asepsis: Infection control protocols and practices
- Anesthesia: Types and administration techniques
Continuing Education to Maintain Excellence in the 4 A’s
It’s important for surgeons to keep learning about the 4 A’s. Conferences, workshops, and online courses help them improve their skills and knowledge.
By staying up-to-date in the 4 A’s, surgeons can make patients’ lives better. They also help orthopedic surgery grow.
Future Directions and Emerging Concepts in the 4 A’s
The future of orthopedic surgery is exciting. New ideas and tech are changing the 4 A’s. These changes come from tech progress and new care standards.
Technological Innovations Shaping Each “A”
New tech is changing the 4 A’s. In Anatomy, better imaging and 3D printing help us understand the body better. For Alignment, tools like computer-assisted navigation make surgeries more precise.
In Asepsis, new ways to sterilize and antimicrobial coatings lower infection risks. And in Anesthesia, new pain management methods are improving patient care.
Evolving Standards and Best Practices
Our knowledge of the 4 A’s is growing. So are the standards and best practices. Key trends include:
- More use of personalized medicine in orthopedic surgery
- More focus on minimally invasive techniques to speed up recovery
- Artificial intelligence being used in planning and doing surgeries
These changes will make orthopedic surgeries safer and more effective.
Conclusion
The 4 A’s of orthopedic surgery are key: Anatomy, Alignment, Asepsis, and Anesthesia. These principles help surgeons give top-notch care to patients. Knowing and using these principles is vital for the best results in orthopedic surgery.
Surgeons who master the 4 A’s make sure patients get full care. They understand the body’s structure, align procedures right, keep things clean, and pick the best anesthesia. This way, patients feel less pain and get better faster.
As orthopedic surgery keeps getting better, the 4 A’s will stay important. Following these rules helps surgeons give excellent care. This care improves patients’ lives and makes them healthier.
FAQ
What are the 4 A’s of Orthopedic Surgery?
The 4 A’s are key in Orthopedic Surgery. They stand for Anatomy, Alignment, Asepsis, and Anesthesia. These principles help surgeons get the best results for patients.
Why is anatomical knowledge important in orthopedic surgery?
Knowing anatomy is vital. It helps surgeons understand how bones and muscles work. This knowledge is key for planning and doing surgeries right.
How does proper alignment impact orthopedic surgery outcomes?
Alignment is very important. It affects how well a surgery works out. It’s key for fixing bones and joints correctly.
What is the significance of asepsis in orthopedic surgery?
Asepsis is critical to avoid infections. Keeping everything clean and sterile is a must. It keeps patients safe during surgery.
What types of anesthesia are used in orthopedic procedures?
There are many anesthetics used. These include regional, general, and local anesthesia. The choice depends on the patient and the surgery.
How do the 4 A’s contribute to successful patient outcomes in orthopedic surgery?
The 4 A’s work together for the best results. They ensure surgeries are done with care and precision. This leads to better outcomes for patients.
What is the role of interdisciplinary collaboration in upholding the 4 A’s?
Teamwork is key. It involves surgeons, anesthesiologists, and nurses working together. This ensures patients get the best care.
How are the 4 A’s integrated into clinical practice?
The 4 A’s are part of everyday practice. They guide planning, surgery, and aftercare. Each “A” is important for patient success.
What is the importance of continuing education in maintaining excellence in the 4 A’s?
Learning never stops. It keeps surgeons up-to-date with new methods and tools. This helps them stay at the top of their game.
How do technological innovations shape the 4 A’s?
New tech changes the game. It improves imaging, tools, and anesthesia. This makes surgeries safer and more effective.