Last Updated on December 1, 2025 by Bilal Hasdemir
Childhood cancer is a rare but devastating disease that affects thousands of children worldwide each year. Recent studies have shown that the incidence of childhood cancer is on the rise, with a significant increase in the number of cases diagnosed annually. We are committed to understanding the complex factors that contribute to childhood cancer development, including genetic and environmental influences.
Understanding the triggers behind genetic mutation triggers is key for developing effective prevention and treatment strategies. We explore the various pediatric tumor causation factors that play a role in the development of tumors in children. Our goal is to shed light on this complex issue.
Key Takeaways
- Childhood cancer is a rare but increasingly common disease.
- Genetic and environmental factors contribute to childhood cancer development.
- Understanding genetic mutation triggers is key for prevention and treatment.
- Pediatric tumor causation factors are complex and multifaceted.
- Effective prevention and treatment strategies are being developed.
Understanding Childhood Tumors
It’s important to understand childhood tumors to improve treatment and outcomes. These tumors are complex, involving genetics, environment, and biology.
Definition and Classification of Pediatric Tumors
Pediatric tumors are abnormal growths in kids under 18. They can be benign or malignant. Knowing the type helps choose the right treatment.
There are many types of pediatric tumors. These include leukemias, lymphomas, brain tumors, and solid tumors like neuroblastoma. Each needs a specific treatment plan.
Prevalence and Incidence Rates
Childhood cancer is a major cause of death in kids. The rates of these tumors vary by age. For example, leukemia is most common in kids aged 2 to 5.
Knowing the rates helps us find risk factors and screen more effectively. This way, we can better use resources and improve treatment.
Differences Between Adult and Pediatric Tumors
Adult and pediatric tumors differ in biology and treatment response. Pediatric tumors often have unique genetic and molecular profiles. This affects their aggressiveness and how well they respond to treatment.
- Genetic Factors: Pediatric tumors are more likely to be linked to genetic mutations and inherited syndromes.
- Tumor Biology: Pediatric tumors can be more diverse and aggressive.
- Treatment Response: Kids usually handle intense treatments better than adults. But, we must watch for long-term effects.
Understanding these differences is key to creating treatments that work best for kids with cancer.
The Biology of Tumor Development in Children
Tumors in kids grow from a mix of cell, developmental, and molecular factors. Knowing these factors helps create better treatments and better outcomes for kids with cancer.
Cellular Transformation Process
The process of cells turning into cancer in kids is complex. It starts with normal cells changing into cancer cells, often because of genetic changes or environmental factors. Genetic mutations are key in this change, causing cells to grow out of control and form tumors.
Studies reveal that how cancer starts in kids is different from adults. Kids’ cancers often have unique genetic and molecular causes. For example, some cancers in kids are caused by specific genetic changes not seen in adult cancers.
Developmental Biology Insights
Developmental biology sheds light on how tumors form in kids. Kids’ cells and tissues grow fast, which raises the risk of genetic changes and cancer. Knowing how growth affects tumor formation helps find new treatments.
Research shows that some developmental paths are broken in kids’ cancers. This leads to tumor growth. For instance, some cancers in kids have too much activity in early developmental paths, pushing tumor growth.
Molecular Signaling Disruption
Disruptions in molecular signaling are also key in kids’ tumors. Signaling pathways control cell growth and behavior. When these pathways are broken, cancer can start. Finding the right signaling pathways in kids’ cancers helps make targeted treatments.
- Some cancers in kids have problems with the PI3K/AKT pathway, making cells live longer and grow more.
- Other cancers might have issues with the MAPK/ERK pathway, causing cells to grow too much.
Understanding the molecular signaling problems in kids’ cancers helps make treatments that target these issues. This could lead to better results for kids with cancer.
Genetic Mutations as Primary Triggers
Genetic mutations are key to understanding pediatric tumors. These changes in DNA can happen on their own or be passed down. They can greatly affect how cells work and grow.
Spontaneous Genetic Mutations
Spontaneous genetic mutations happen without a known cause. They can come from errors in DNA copying or environmental factors. In kids, these mutations can cause tumors by messing with cell functions.
Spontaneous mutations in genes important for cell growth can lead to cancer. We’ll see how these mutations cause tumors.
Oncogenes and Tumor Suppressor Genes

Oncogenes and tumor suppressor genes control cell growth. Oncogenes can cause cancer if they mutate or are too active. On the other hand, tumor suppressor genes stop cancer by fixing DNA, slowing cell division, or killing damaged cells.
Genetic Instability Factors
Genetic instability means cells are more likely to change their DNA. This can happen because of DNA repair problems or issues with chromosome division. Factors that cause genetic instability can make cells more likely to get tumors.
Knowing what causes genetic instability is key to fighting cancer. We’ll look at how these factors work with others to cause childhood tumors.
Inherited Cancer Syndromes
It’s important to know about inherited cancer syndromes to understand childhood cancer risks. These syndromes are genetic and can greatly increase cancer risk.
Li-Fraumeni Syndrome
Li-Fraumeni Syndrome is a rare genetic disorder. It makes people, mostly kids and young adults, more likely to get cancer. It’s linked to a gene called TP53.
Having Li-Fraumeni Syndrome in your family means you might get cancers like breast cancer, brain tumors, and sarcomas. Testing for TP53 mutations can help catch these risks early.
Retinoblastoma and RB1 Gene Mutations
Retinoblastoma is a cancer that mostly hits young kids. It’s caused by RB1 gene mutations. This cancer often shows up in both eyes early on.
Testing for RB1 mutations can spot at-risk kids. Knowing the genetic cause helps manage the disease and lower the chance of more cancers.
Other Hereditary Cancer Risk Factors
There are other syndromes that raise childhood cancer risk too. For example, familial adenomatous polyposis (FAP) and neurofibromatosis type 1 (NF1).
| Syndrome | Gene Mutation | Cancer Risk |
| Li-Fraumeni Syndrome | TP53 | Breast cancer, brain tumors, sarcomas |
| Retinoblastoma | RB1 | Eye cancer |
| Familial Adenomatous Polyposis (FAP) | APC | Colorectal cancer |
| Neurofibromatosis Type 1 (NF1) | NF1 | Nerve tissue tumors |
Knowing about these syndromes and their genes is key for helping kids with cancer. It helps doctors find and prevent problems early.
Chromosomal Abnormalities in Pediatric Tumors
Tumors in children often come with chromosomal changes. These changes help us understand the disease better. Chromosomal abnormalities are common in many pediatric tumors.
Translocations and Fusion Genes
Translocations are big changes in chromosomes. They happen when parts of two chromosomes swap places. This creates fusion genes, which are abnormal proteins that help tumors grow.
For example, Ewing’s sarcoma, a bone cancer in kids, often has the EWS-FLI1 fusion gene.
Chromosomal Deletion and Duplication
Chromosomal deletions and duplications are also common. Deletions mean losing genetic material. Duplications mean gaining extra genetic material.
These changes can mess with genes that control cell growth. Losing tumor suppressor genes can cause tumors to grow without control.
Detection Methods for Chromosomal Abnormalities
Finding chromosomal changes is key for treating pediatric tumors. We use karyotyping, fluorescence in situ hybridization (FISH), and array comparative genomic hybridization (aCGH) to find these changes.
These methods help doctors know what changes are there. This information helps decide treatment and gives clues about the tumor’s future.
Environmental Exposure Risks
We look into how the environment can lead to tumors in kids. Things like radiation and chemicals can increase cancer risk in children. Knowing how these affect us can help us fight cancer better.
Radiation Exposure
Radiation is a big risk for kids getting cancer. Ionizing radiation can change genes and cause cancer. Kids are more at risk because their bodies are growing.
Sources of radiation exposure include:
- Medical imaging procedures, such as CT scans
- Nuclear accidents or fallout
- Certain industrial or occupational exposures
Chemical Carcinogens
Chemicals that can cause cancer are everywhere. Kids can get exposed through air, water, and food. This is because of pollution and contaminated items.
Examples of chemical carcinogens include:
- Benzene, found in gasoline and industrial emissions
- Pesticides and herbicides
- Polycyclic aromatic hydrocarbons (PAHs)
Parental Occupational Exposures
Jobs can also affect kids’ cancer risk. Chemicals from work can get home on clothes or in other ways. This can expose kids.
Occupations associated with increased risk include:
- Industrial workers exposed to chemicals
- Healthcare workers exposed to certain drugs or radiation
- Workers in the agricultural sector exposed to pesticides
To show how environment and cancer are linked, here’s a summary:
| Exposure Type | Examples | Potential Cancer Risk |
| Radiation Exposure | Medical imaging, nuclear accidents | Leukemia, other cancers |
| Chemical Carcinogens | Benzene, pesticides, PAHs | Leukemia, lymphoma, other cancers |
| Parental Occupational Exposures | Industrial chemicals, agricultural pesticides | Various childhood cancers |
In conclusion, environmental risks are key to understanding childhood cancer. By knowing these risks, we can lower the chance of kids getting cancer.
Viral Infections and Immune System Factors
It’s important to know how viral infections and childhood cancer are connected. Some viruses can increase the risk of cancer in kids. We need to study this link more.
Oncogenic Viruses in Childhood Cancer
Oncogenic viruses can cause cancer in kids. For example, the Epstein-Barr virus (EBV) is linked to lymphoma and other cancers. EBV infects B lymphocytes, which can grow out of control and form tumors.
These viruses disrupt normal cell functions. They can change the host’s genes and weaken the immune system. This leads to tumor growth.
Immune System Disorders and Cancer Risk
Immune system problems can raise cancer risk in kids. Kids with weak immune systems are more likely to get infections and cancer.
For instance, kids with primary immunodeficiency diseases struggle to fight cancer cells. Kids on immunosuppressive therapy, like those with organ transplants, also face higher cancer risks.
Immunosuppression and Tumor Development
Immunosuppression makes it hard for the body to stop tumor growth. A weakened immune system can’t fight off cancer cells well. This can lead to tumors.
Understanding how viruses, immune issues, and immunosuppression work together is key. It helps us find better treatments and prevention for kids with cancer.
Pediatric Tumor Causation Factors: A Comprehensive Overview
Childhood tumors come from a mix of genetic changes, environmental factors, and age-specific risks. Knowing these is key to better prevention and treatment.
Multifactorial Nature of Childhood Tumors
Childhood tumors are complex, caused by many genetic and environmental factors. These factors work together in complex ways, making it hard to pinpoint a single cause.
Both genetics and environment play a part in these tumors. For example, some genetic syndromes raise the risk of certain tumors.
Interaction Between Genetic and Environmental Factors
Childhood tumors often result from the mix of genetic and environmental factors. Genetic changes can affect how cells react to the environment. At the same time, environmental factors can change gene expression.
For example, ionizing radiation can lead to genetic mutations, increasing tumor risk. Environmental toxins can also interact with genes, raising cancer risk.
Age-Specific Risk Factors
Age is a big factor in childhood tumors. Different tumors are more common at different ages, showing age-specific risks.
Infantile tumors have unique genetic traits compared to those in older kids. Understanding these age-specific risks allows us to design targeted prevention strategies and enhance screening efforts.
Common Types of Childhood Tumors and Their Causes
It’s important to know about the different kinds of tumors in kids. Childhood cancers come in many forms, each with its own risk factors and causes.
Leukemias and Lymphomas
Leukemias are the top cancer in kids, making up 30% of all childhood cancers. Acute lymphoblastic leukemia (ALL) is the most common, where lymphoblasts grow too much in the bone marrow. We don’t know all the causes, but genetics and the environment might play a part.
Lymphomas are another common cancer in kids, affecting the lymphatic system. Hodgkin lymphoma and non-Hodgkin lymphoma are the main types, with different risks. Epstein-Barr virus can raise the risk of some lymphomas.
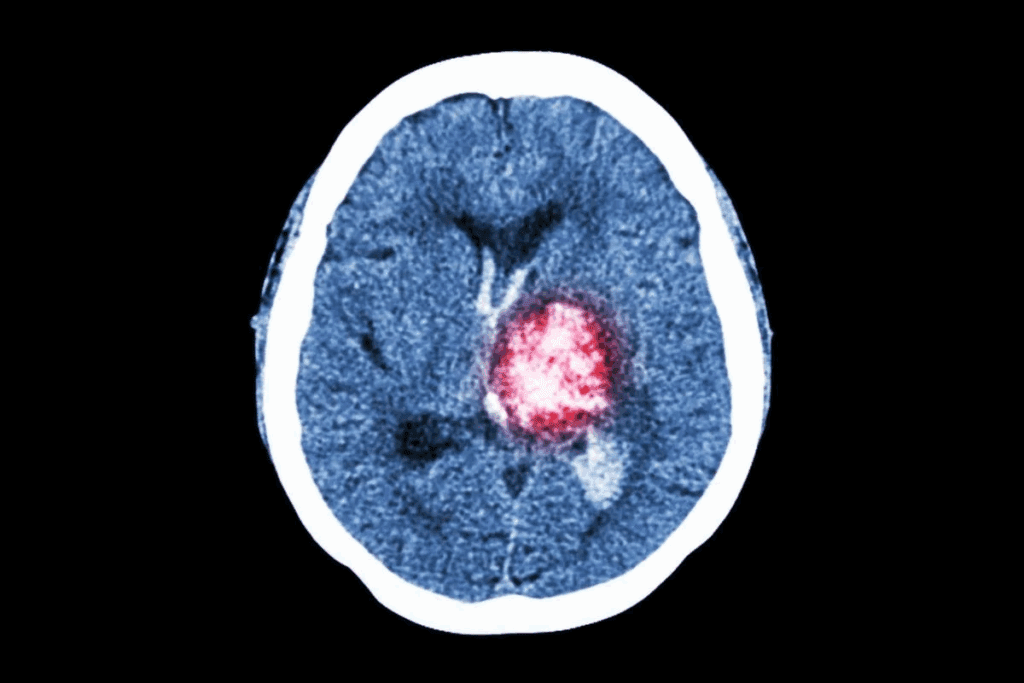
Brain and Central Nervous System Tumors
Brain and CNS tumors are the second most common in kids. They can happen in different parts of the brain and spinal cord. Medulloblastoma and gliomas are common types. Genetic conditions like neurofibromatosis can increase the risk.
“The development of brain tumors in children is often associated with genetic predisposition and certain environmental exposures.” – Expert in Pediatric Oncology
Solid Tumors: Neuroblastoma, Wilms Tumor, and Rhabdomyosarcoma
Solid tumors in kids include neuroblastoma, Wilms tumor, and rhabdomyosarcoma. Each has its own features and age groups. Neuroblastoma comes from neural crest cells and can be in different places. Wilms tumor affects the kidneys, and rhabdomyosarcoma is a soft tissue sarcoma that can be anywhere in the body.
The causes of these tumors are both genetic and environmental. For example, mutations in the WT1 gene increase Wilms tumor risk. Knowing these causes helps us find better ways to prevent and treat these cancers.
Diagnostic Approaches for Identifying Tumor Causes
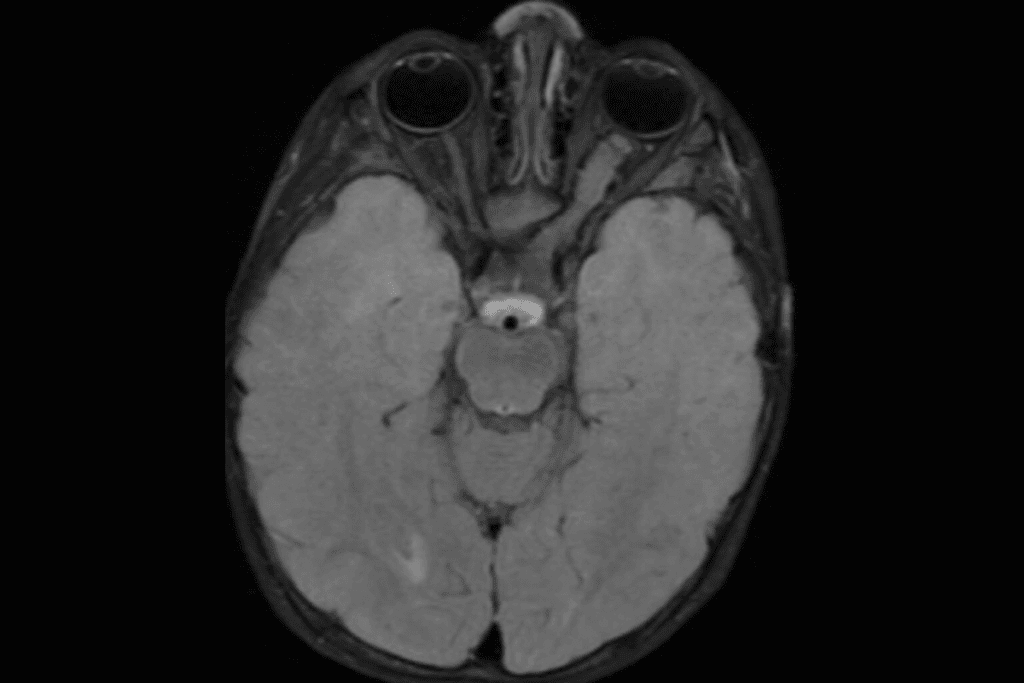
Diagnosing childhood tumors is key to finding their causes. Today’s diagnostic methods are much better. They help doctors give accurate diagnoses and treatments.
Medical Diagnostic Techniques
Medical tests are essential for diagnosing childhood tumors. MRI and CT scans show where and how big the tumor is. They also check if it has spread.
Biopsy procedures are also important. They let doctors look at tumor cells. This helps them know the tumor’s type and how aggressive it is.
Ultrasound and X-ray exams give first clues about tumors. These tests, along with doctor’s checks, help diagnose tumors in kids.
Genetic Testing and Counseling
Genetic testing is vital for understanding childhood tumors. It looks at a child’s genes to find mutations that might cause the tumor. This info helps doctors plan treatments.
Genetic counseling is also important. It tells families about their child’s genetic condition. It also talks about family planning and risk for other family members.
Molecular Profiling of Tumors
Molecular profiling looks at tumor cells’ genetics and molecules. It finds biomarkers that help decide treatments. This approach gives insights into how the tumor might behave.
Techniques like next-generation sequencing analyze tumor genetics deeply. They find targets for treatments. This helps in making treatment plans that fit each child’s needs.
| Diagnostic Approach | Description | Benefits |
| Medical Imaging | Use of MRI, CT scans, and other imaging techniques to visualize tumors. | Accurate tumor localization and sizing. |
| Biopsy and Histopathology | Examination of tumor tissue to determine cell type and aggressiveness. | Definitive diagnosis and tumor classification. |
| Genetic Testing | Analysis of genetic material to identify mutations associated with tumors. | Identification of genetic predispositions and targeted treatment options. |
| Molecular Profiling | Detailed analysis of tumor genetics to identify biomarkers and therapeutic targets. | Personalized treatment planning and possible targeted therapies. |
Screening and Early Detection Strategies
Screening is key in finding childhood cancers early. This boosts the chance of successful treatment. Early detection can lead to better outcomes for kids.
Medical Screening Methodology
Screening for childhood cancer includes various tests. These are based on the child’s age, risk factors, and medical history. Comprehensive physical examinations are vital. They can spot abnormalities that might mean cancer.
Imaging tests like X-rays, ultrasounds, and MRIs help see inside the body. These tests are used to check for cancer before symptoms show.
We use these methods to catch problems early. For example, ultrasound is often used for kids at risk of certain tumors, like Wilms tumor.
| Screening Method | Description | Application |
| Physical Examination | Comprehensive check-up to identify abnormalities | Routine check-ups, risk assessment |
| Imaging Tests (X-rays, Ultrasound, MRI) | Visualization of internal organs and structures | Diagnostic purposes, monitoring |
| Blood Tests | Analysis of blood components to detect markers or abnormalities | Diagnostic support, monitoring treatment response |
Risk-Based Screening Approaches
Risk-based screening focuses on kids at higher cancer risk. This includes genetic predispositions, family history, or environmental factors. Genetic testing is key in identifying these risks.
For kids with a genetic risk, we use more careful screening. This includes regular imaging and biomarker tests. It helps find cancer early.
Emerging Screening Technologies
Pediatric oncology is seeing new screening tech, like liquid biopsies and next-generation sequencing (NGS). These could lead to earlier, more accurate cancer detection.
Liquid biopsies check blood for cancer DNA without surgery. NGS quickly sequences genes to find cancer-causing mutations.
As these techs improve, they’ll likely become part of our standard screening. This will help us detect and treat childhood cancers better.
Prevention Strategies Based on Causal Factors
We can fight childhood tumors by understanding their causes. This knowledge helps us create better prevention plans. It’s key to lowering the risk of cancer in kids.
Reducing Environmental Exposures
One big way to prevent cancer is to cut down on harmful environmental exposures. This means less ionizing radiation, certain chemicals, and pollutants.
- Avoiding unnecessary medical radiation
- Reducing exposure to pesticides and herbicides
- Limiting contact with heavy metals and other pollutants
Genetic Counseling for High-Risk Families
Genetic counseling is vital for families with a history of cancer. It helps figure out the risk of passing on cancer-causing genes.
| Genetic Syndrome | Cancer Risk | Counseling Approach |
| Li-Fraumeni Syndrome | High risk of various cancers | Comprehensive genetic testing and surveillance |
| Retinoblastoma | Eye cancer in children | Genetic testing for RB1 gene mutations |
Lifestyle and Nutrition Considerations
Lifestyle and diet can also affect cancer risk in kids. While some factors are out of their control, good nutrition can help.
Nutritional Factors: Eating more fruits, veggies, and whole grains is good. Avoid too much processed food and sugar.
Maternal Health: What the mom eats and stays healthy during pregnancy matters a lot for the kid’s cancer risk.
Current Research and Future Directions
Research is making big strides in understanding childhood tumors. We’re learning more about the causes and how they start. This is thanks to new medical tech and scientific discoveries.
Advances in Understanding Tumor Initiation
Studies have greatly improved our knowledge of tumor start in kids. It’s clear that genetic changes are key in many cancers. For example, some cancers start from random genetic changes, while others are linked to inherited conditions.
Key factors in tumor initiation include:
- Genetic instability
- Oncogene activation
- Tumor suppressor gene inactivation
Targeted Therapies Based on Causal Factors
Targeted therapies are a big step forward in treating childhood cancer. By knowing the genetic and molecular reasons behind tumors, scientists can create treatments that directly target these causes.
Examples of targeted therapies include:
- Tyrosine kinase inhibitors for leukemias with specific genetic mutations
- PARP inhibitors for tumors with defects in DNA repair mechanisms
- Immunotherapies that harness the body’s immune system to fight cancer
Promising Areas of Research
There are many promising research areas for tackling childhood tumors. These include studying the tumor environment, the role of epigenetics, and precision medicine.
Emerging trends in pediatric cancer research:
- Integration of genomic data with clinical information
- Development of novel therapeutic agents
- Investigation of the impact of environmental exposures on cancer risk
Conclusion: The Complex Landscape of Childhood Tumor Causation
Understanding childhood tumor causes is key to better prevention and treatment. We’ve looked at many factors, like genetic changes and environmental exposures. These include genetic mutations and inherited syndromes.
The way these factors work together is complex. Their effects can change based on the child’s age. Knowing this helps us find and help high-risk kids early.
New technologies like genetic testing are helping us understand tumors better. We’re learning more about how tumors grow. This knowledge leads to new treatments and better care for kids.
We must keep studying to improve treatments for childhood tumors. This research will help us find more effective ways to fight these diseases.
FAQ
References:
- Chen, X., et al. (2024). Developmental origins shape the pediatric cancer genome. Nature Communications, 15, 2124.https://pmc.ncbi.nlm.nih.gov/articles/PMC11571274/