Last Updated on December 3, 2025 by Bilal Hasdemir

When a loved one gets a brain tumor diagnosis, it makes you think about family risks. Studies show that genetic risk might play a part in some brain tumors. We’ll look into how brain tumors family history affects your risk.Learn how brain tumors family history increases genetic risk and prevention tips.
Knowing if brain tumors can be hereditary is key to understanding your risk. We’ll dive into familial brain tumor syndrome and its impact on families with a history of brain tumors.
Key Takeaways
- Understanding the genetic risk associated with brain tumors.
- The role of family history in assessing brain tumor risk.
- Exploring familial brain tumor syndrome and its implications.
- Steps to take if there’s a history of brain tumors in your family.
- The importance of genetic counseling for at-risk families.
The Basics of Brain Tumors
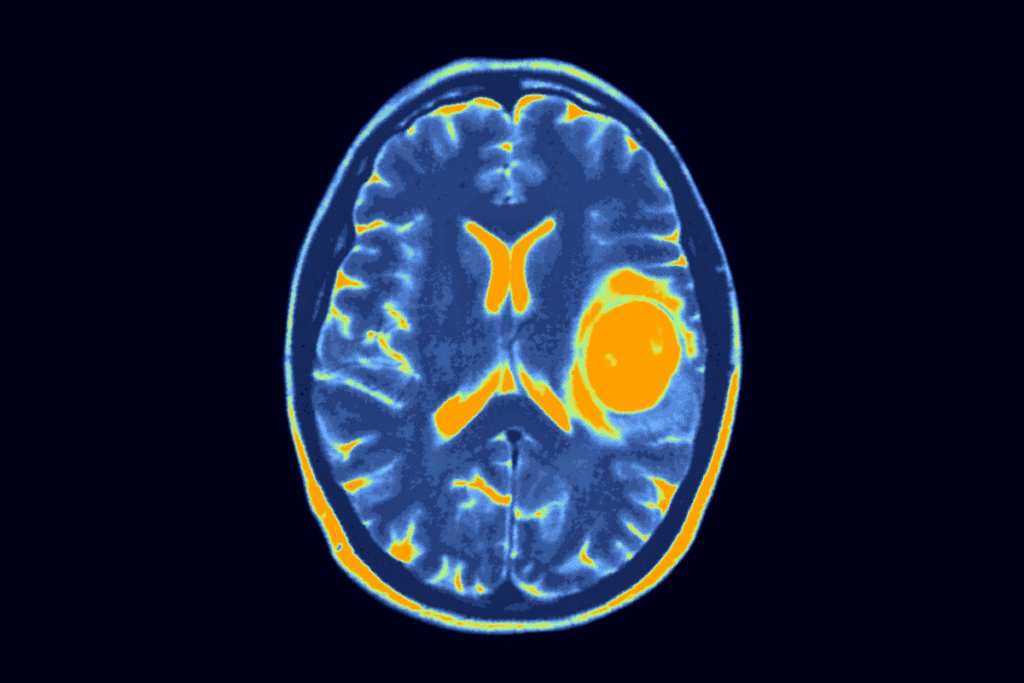
Brain tumors come in many forms, each with its own traits. Knowing these differences is vital for effective treatment. They can be benign or malignant, affecting the brain and health differently.
Types of Brain Tumors
Brain tumors are divided into primary and secondary types. Primary tumors start in the brain. Secondary tumors come from cancer spreading to the brain from elsewhere.
- Primary Brain Tumors: These can be benign or malignant and include types such as gliomas, meningiomas, and acoustic neuromas.
- Secondary Brain Tumors: These are metastatic tumors that have spread from cancers in other parts of the body, such as the lung, breast, or skin.
Common Symptoms and Warning Signs
The symptoms of brain tumors depend on their location, size, and type. Common symptoms include:
- Headaches that are persistent or severe
- Seizures, even if you’ve never had them before
- Nausea or vomiting, often in the morning
- Weakness or numbness in the arms or legs
- Difficulty with speech or understanding language
- Vision problems, like blurred vision, double vision, or loss of peripheral vision
If you experience these symptoms, it’s important to see a doctor. They should not be ignored.
General Risk Factors
While we don’t know all the causes of brain tumors, some risk factors have been found. These include:
- Age: The risk of getting a brain tumor goes up with age.
- Genetic Predisposition: Some genetic conditions, like Li-Fraumeni syndrome or neurofibromatosis, raise the risk.
- Exposure to Radiation: Being exposed to ionizing radiation, like from radiation therapy, can increase the risk.
Knowing these risk factors can help you understand your own risk. It might also help you take steps to prevent them.
Understanding Brain Tumors Family History
Looking into your family’s history of brain tumors can tell you a lot. It can show if you might be at higher risk for brain cancer. We’ll dive into the details of brain tumors that run in families. This includes how common they are and the risks for different family members.
What Constitutes a Family History of Brain Tumors
A family history of brain tumors means more than one family member has had one. This can include gliomas, meningiomas, and acoustic neuromas. Just because your family has had brain tumors doesn’t mean you will get one. But, it might mean you’re at higher risk.
Family history is important because it can show genetic links. For example, Li-Fraumeni syndrome, neurofibromatosis, and tuberous sclerosis complex can raise brain tumor risks. Knowing these genetic factors helps figure out your own risk.
Statistical Prevalence of Familial Brain Tumors
Studies show many brain tumors might have a family link. If a first-degree relative has a brain tumor, your risk goes up. About 5-10% of brain tumors might be due to genetics.
- Familial glioma risks are high, as gliomas are common and often deadly.
- Being related to someone with glioma, and being young when they got it, raises your risk even more.
First-Degree vs. Extended Family Risk
The risk from family history changes based on how closely related you are. First-degree relatives, like parents and siblings, face higher risks. This is because they share more genes.
- First-degree relatives include parents, children, and siblings.
- Extended family, like grandparents and aunts, also add to the family history. But the risk is lower than for first-degree relatives.
Knowing the difference between first-degree and extended family risks helps understand your risk better. If you have a strong family history, talk to a doctor. They can give you advice and suggest screenings.
Genetic Predisposition to Brain Tumors
It’s important to know how genes affect brain tumors. This knowledge helps us understand our risk. Finding the genes linked to brain tumors can lead to early detection and prevention.
Influence of Genes on Brain Tumor Development
Genes control how cells grow and divide. When genes mutate, cells can grow out of control. This can cause tumors to form.
Key Genetic Mechanisms:
- Mutations in tumor suppressor genes
- Alterations in DNA repair genes
- Changes in oncogenes
Sporadic vs. Inherited Genetic Mutations
Brain tumor mutations can be either random or inherited. Random mutations happen by chance and aren’t passed down. Inherited mutations come from family genes.
| Mutation Type | Description | Risk Factor |
| Sporadic | Random mutations not inherited | Variable, often related to environmental factors |
| Inherited | Mutations passed down through families | Higher risk if family history is present |
Common Genetic Markers Associated with Brain Tumors
Some genes are linked to a higher risk of brain tumors. These include TP53, NF1, and VHL genes.
Knowing these markers helps us find people at higher risk. We can then take steps to screen and prevent brain tumors.
Hereditary Brain Cancer Risk Factors
It’s important to know the risk factors for hereditary brain cancer, mainly for families with a history of brain tumors. While genetics are key, other factors also play a role.
Environmental Factors That Interact with Genetic Predisposition
Studies show that environmental factors can affect the risk of brain tumors, even with a genetic predisposition. For example, ionizing radiation is a big risk factor, more so for those with a genetic risk.
Key environmental factors to consider include:
- Exposure to ionizing radiation
- Certain chemicals and pollutants
- Infections and other environmental exposures
Age and Gender Considerations in Familial Cases
Age and gender can also impact the risk of hereditary brain tumors. Some families may see tumors at a younger age. Also, some tumors are more common in one gender.
For instance, meningiomas are more common in women, while glioblastomas are more common in men. Knowing these patterns helps in assessing family risk.
Cumulative Risk Assessment
A cumulative risk assessment looks at many factors. This includes genetic predisposition, environmental exposures, and health conditions. It aims to estimate an individual’s risk of brain cancer.
Cumulative risk assessment involves:
- Evaluating family history and genetic markers
- Assessing environmental exposures
- Considering other health conditions and risk factors
By understanding these factors and their interactions, families can better assess their risk. This helps them make informed health decisions.
Familial Brain Tumor Syndromes
It’s key to know about familial brain tumor syndromes if you have a family history of brain tumors. These are genetic disorders that make you more likely to get brain tumors.
Li-Fraumeni Syndrome
Li-Fraumeni Syndrome is a rare genetic disorder. It greatly raises your risk of getting several cancers, including brain tumors. It’s caused by a mutation in the TP53 gene. People with this syndrome should get regular check-ups to catch tumors early.
Neurofibromatosis Types 1 and 2
Neurofibromatosis Type 1 (NF1) and Type 2 (NF2) are genetic conditions. They can cause tumors on nerve tissue. NF1 leads to skin color changes and nerve tumors. NF2 causes tumors on nerves that control hearing and balance.
- NF1 raises the risk of gliomas, like optic gliomas.
- NF2 increases the risk of schwannomas, meningiomas, and ependymomas.
Tuberous Sclerosis Complex
Tuberous Sclerosis Complex (TSC) is a genetic disorder. It causes non-cancerous tumors to grow in the body, including the brain. TSC is caused by mutations in the TSC1 or TSC2 gene. It can lead to epilepsy, developmental delays, and behavioral issues.
Von Hippel-Lindau Disease
Von Hippel-Lindau Disease (VHL) is an inherited disorder. It makes people more likely to get certain tumors, like brain hemangioblastomas. VHL is caused by a mutation in the VHL gene. Managing VHL means regular tumor screenings and other disease checks.
Familial brain tumor syndromes show how genetics play a big role in brain tumors. Knowing about these syndromes helps in early detection and management of brain tumors in families.
Pediatric Brain Tumors and Genetic Inheritance
Pediatric brain tumors have a complex genetic makeup. They involve inherited and random mutations. Knowing these genetic factors is key for families with brain tumor history. It helps them make informed choices about screening, prevention, and treatment.
Unique Genetic Factors in Childhood Brain Tumors
Childhood brain tumors come from specific genetic changes. These changes might be passed down or happen by chance. For example, Li-Fraumeni syndrome and neurofibromatosis raise the risk of brain tumors in kids.
These conditions can cause tumors to appear earlier and increase the chance of more tumors. Knowing the genetic causes is vital for managing risk and setting up surveillance plans.
Familial Patterns in Pediatric Cases
Familial patterns are important in understanding pediatric brain tumor risk. Research shows kids with a family history of brain tumors are at higher risk. This risk is even higher in families with certain genetic syndromes.
Spotting these patterns helps assess risk and guide genetic testing and counseling. It’s important for doctors to take a detailed family history to find genetic risks.
Developmental Considerations
Brain tumors in kids are shaped by genetics and environment. The critical periods are during fetal development and early childhood. This is when genetic mutations can cause tumors.
Understanding these developmental stages helps us grasp how pediatric brain tumors form. It also leads to new treatments. Recognizing the role of genetics and development helps in early detection and treatment.
Genetic Testing for Brain Tumor Susceptibility
Genetic testing for brain tumors is growing fast. It helps us understand our risk better. As we learn more about genes linked to brain tumors, testing becomes key for spotting high-risk people.
Available Testing Methods
There are many genetic tests for brain tumor risk. These include:
- Single Gene Testing: This tests for specific genes like TP53 in Li-Fraumeni syndrome.
- Multi-Gene Panel Testing: This tests many genes at once for a wider view of risk.
- Whole Exome Sequencing (WES): WES looks at all protein-coding parts of the genome for detailed genetic info.
Each test has its benefits. The right one depends on family and medical history, and other factors.
When Genetic Testing Is Recommended
Testing is suggested for those with a strong family history of brain tumors or cancers. It’s also for young people with brain tumors or certain genetic syndromes.
Interpreting Test Results
Understanding genetic test results needs expertise. A positive result means higher risk, but it’s not a sure thing. A negative result doesn’t mean no risk, as some factors might not be caught.
Insurance and Cost Considerations
Genetic test costs vary a lot. It depends on the test and lab. Insurance coverage also differs. It’s important to talk to your insurance and healthcare provider about costs.
As genetic testing improves, we expect better and cheaper tests. This will help us manage brain tumor risk better.
Genetic Counseling for Families with Brain Tumor History
Genetic counseling is key for families with brain tumor history. It helps understand genetic factors and aids in making health decisions.
The Role of Genetic Counselors
Genetic counselors are experts in genetics and counseling. They help families by understanding their medical history and genetic risks. They also explain genetic testing implications.
Genetic counselors are vital in:
- Interpreting genetic test results
- Providing emotional support and guidance
- Facilitating discussions about family planning
- Connecting families with relevant resources
Family Planning Considerations
Genetic counseling offers insights for families with brain tumor history. It discusses genetic risks and family planning options.
| Family Planning Option | Description | Considerations |
| Genetic Testing | Testing for specific genetic mutations associated with brain tumors | Risks, benefits, and limitations of testing |
| Preimplantation Genetic Diagnosis (PGD) | A technique used during IVF to identify genetic disorders in embryos | Success rates, ethical considerations, and cost |
| Family Planning Counseling | Counseling to discuss reproductive options and risks | Emotional support, decision-making strategies |
Psychological Support During the Counseling Process
Discussing genetic risks and family planning can be tough. Genetic counselors offer psychological support. They help families deal with the stress and uncertainty of genetic testing and decision-making.
Key aspects of psychological support include:
- Emotional support and empathy
- Strategies for coping with uncertainty
- Resources for additional support, such as support groups
Comprehensive genetic counseling empowers families to make informed health decisions.
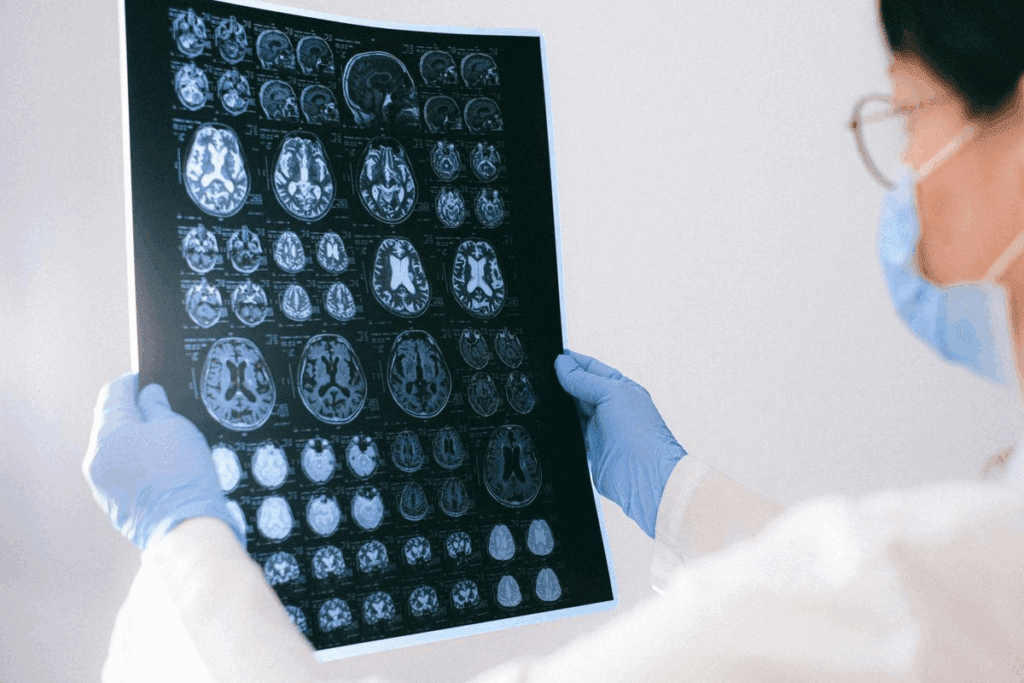
Screening Recommendations for High-Risk Families
Screening is key for families at high risk of brain tumors. It helps find tumors early. Families with a history of brain tumors should know the latest screening options.
Current Guidelines for Monitoring
Monitoring high-risk families involves several steps. It’s important for families to talk to a healthcare provider. They will decide the best screening plan based on the family’s risk.
The American Cancer Society and other groups give guidelines. Healthcare providers use these to suggest screenings for those at high risk.
Imaging Technologies and Protocols
Advanced imaging is vital for catching brain tumors early. MRI (Magnetic Resonance Imaging) is often used. It’s very sensitive and shows the brain’s details well.
For those at high risk, the protocols might include:
- Annual or biennial MRI scans
- Contrast-enhanced MRI for better visualization
- Specific sequences like FLAIR or T1-weighted images
Frequency of Screening Based on Risk Level
How often to screen depends on the risk level. This level is based on family history, genetics, and other factors.
| Risk Level | Recommended Screening Frequency |
| High Risk | Annual MRI |
| Moderate Risk | Biennial MRI or as recommended by a healthcare provider |
| Low Risk | Screening may not be recommended unless other risk factors are present |
Families should work with their healthcare providers. Together, they can figure out the best screening schedule for each family’s risk.
Living with Inherited Brain Tumor Risk
Brain tumors in families can cause a mix of feelings and worries about the future. Knowing you might get a brain tumor can make you more careful but also anxious.
The Psychological Impact on Family Members
Knowing you might get a brain tumor can deeply affect family members. It can make them feel more anxious, scared, and vulnerable.
Family members might feel many things, like denial or always being on guard. Support from doctors, family, and friends is very important during this time.
“The emotional toll of knowing one’s risk for brain tumors cannot be overstated. It’s a burden that requires a lot of support.”
Support Groups and Resources
Support groups are key for dealing with the psychological impact of inherited brain tumor risks. They offer a place to share, get emotional support, and learn how to manage risks.
- Groups like the National Brain Tumor Society and the American Cancer Society help families with brain tumors.
- Online forums and local groups connect families with others facing similar issues.
- Genetic counseling helps understand genetic testing and personal risk.
| Resource | Description | Contact Information |
| National Brain Tumor Society | Provides information, resources, and support for brain tumor patients and families. | www.braintumor.org |
| American Cancer Society | Offers a range of resources, including support groups and information on cancer risk and prevention. | www.cancer.org |
Balancing Awareness with Quality of Life
Balancing awareness of risk with a good quality of life is hard for families with brain tumor history. It’s key to know the risks and take steps to prevent them. But, it’s also important not to let fear control your life.
Families can find this balance by staying informed, getting regular health checks, and joining support groups. This way, they can lower their anxiety and improve their overall happiness.
- Stay updated on the latest research and guidelines on brain tumor risk and management.
- Get regular health check-ups and screenings as advised by doctors.
- Join support groups to connect with others facing similar challenges.
Research Advances in Familial Brain Tumor Genetics
Recent breakthroughs in genetic research have greatly improved our understanding of familial brain tumors. We now know more about specific genetic markers and how to use precision medicine. These advances are changing the field.
Recent Discoveries in Genetic Markers
Scientists have found genetic mutations linked to a higher risk of brain tumors. For example, the TP53 gene mutation, common in Li-Fraumeni syndrome, is associated with brain tumors. Also, mutations in NF1 and NF2 genes, found in Neurofibromatosis types 1 and 2, are risk factors.
These findings help us understand genetic risks better. They also guide genetic testing and counseling.
| Genetic Marker | Associated Syndrome | Risk Implication |
| TP53 | Li-Fraumeni Syndrome | Increased risk of brain tumors |
| NF1 | Neurofibromatosis Type 1 | Higher incidence of brain tumors |
| NF2 | Neurofibromatosis Type 2 | Increased risk of vestibular schwannomas |
Ongoing Clinical Trials
Many clinical trials are underway to find new treatments and diagnostic methods for familial brain tumors. These trials are key to improving our understanding and patient care.
For instance, one trial is looking at targeted therapy for brain tumors with specific genetic mutations. Another trial is studying advanced imaging for early detection.
Precision Medicine Approaches
Precision medicine is changing how we treat familial brain tumors. It tailors treatment to each patient’s genetic profile. This approach has shown to improve outcomes and reduce side effects.
By identifying the genetic changes that cause tumors, doctors can choose targeted therapies. This personalized treatment is a big step towards better and safer care.
Preventive Strategies for Those with Family History
Preventive strategies are key for those with a family history of brain tumors. By using these strategies, people can lower their risk of getting brain tumors.
Lifestyle Modifications
Lifestyle changes are important for those with a family history of brain tumors. These changes include eating right, staying active, and avoiding harmful substances.
Eating a balanced diet with lots of fruits, veggies, and whole grains is good. Foods like berries and leafy greens are full of antioxidants. Regular exercise, like walking or jogging, helps keep you healthy and might lower cancer risk.
- Eat a balanced diet rich in fruits and vegetables
- Engage in regular physical activity
- Avoid tobacco and limit alcohol consumption
Environmental Exposure Reduction
Reducing exposure to harmful substances is also vital. This means avoiding ionizing radiation, certain chemicals, and pesticides.
Be careful with tests that use radiation, like CT scans. Follow safe use guidelines. Also, try to avoid pesticides and industrial chemicals.
- Minimize exposure to ionizing radiation
- Avoid exposure to harmful chemicals and pesticides
- Use protective gear when working with hazardous materials
Emerging Preventive Treatments
There’s ongoing research into new ways to prevent brain tumors. This includes using drugs or supplements to prevent cancer and boosting the immune system to stop tumors from forming.
These treatments are not yet proven but show promise. We’ll look at some studies and possible treatments.
| Preventive Measure | Description | Potential Benefit |
| Lifestyle Modifications | Dietary changes, regular exercise, avoiding harmful substances | Reduces overall cancer risk, improves health |
| Environmental Exposure Reduction | Minimizing radiation, avoiding harmful chemicals | Reduces risk of carcinogen exposure |
| Chemoprevention | Using drugs or supplements to prevent cancer | Potential to prevent tumor development |
When to Consult a Specialist About Family Brain Tumor History
If you have a family history of brain tumors, knowing when to see a specialist is key. Knowing your family’s health history can spot genetic risks. This helps you make smart health choices.
Warning Signs That Warrant Medical Attention
Some signs mean you should talk to a specialist about your family’s brain tumor history. These include:
- A first-degree relative (parent, child, or sibling) diagnosed with a brain tumor
- Multiple family members across generations diagnosed with brain tumors
- A personal or family history of genetic syndromes linked to brain tumors, like Li-Fraumeni syndrome or neurofibromatosis
Spotting these signs can lead you to get medical tests and possibly genetic testing.
Finding Specialists in Neuro-Oncology Genetics
To find a specialist, start by asking your doctor for a referral to a neuro-oncologist or genetic counselor. You can also:
- Check with your insurance for specialists in your network
- Look up specialists through the National Cancer Institute or the American Society of Clinical Oncology
- Ask for recommendations from brain tumor support groups or online forums
Finding the right specialist can offer you tailored advice and support.
| Specialist Type | Role |
| Neuro-Oncologist | Specializes in the diagnosis and treatment of brain tumors |
| Genetic Counselor | Provides guidance on genetic testing and interpreting test results |
Questions to Ask Your Healthcare Provider
When you see a specialist, ask important questions to grasp your risks and how to manage them. Some key questions include:
- What are the chances that my family history indicates a genetic predisposition to brain tumors?
- Should I undergo genetic testing, and if so, what tests are recommended?
- What screening protocols are appropriate for me based on my family history?
- Are there any preventive measures or lifestyle changes that can reduce my risk?
Being informed and proactive can greatly improve your health outcomes.
“Understanding your genetic risk factors can empower you to take control of your health. Consulting with specialists and being aware of your family’s medical history are key steps in managing and potentially reducing your risk of developing brain tumors.”
Conclusion: Understanding Your Personal Risk and Next Steps
Knowing your risk of brain tumors is key, thanks to family history. We’ve seen how genes can play a big part in brain tumor development. Certain genetic syndromes can raise this risk.
If your family history worries you, see specialists in neuro-oncology genetics. Genetic tests can show your risk level. This helps you make smart choices about screenings and prevention. We urge you to act early, seeking expert advice to manage your risk.
By grasping your risk and taking action, you can catch brain tumors early. This might lower your risk. We’re here to help, with top-notch healthcare and support services for you.
FAQ
What is the likelihood of developing a brain tumor if there is a family history?
The chance of getting a brain tumor from family history changes. It depends on the genetic factors and how closely related you are. We look at your family history and genetics to figure out your risk.
Are certain types of brain tumors more likely to be hereditary?
Yes, some brain tumors are more likely to run in families. For example, Li-Fraumeni Syndrome, Neurofibromatosis, and Von Hippel-Lindau Disease. Knowing the type of tumor is key to understanding your risk.
How do genetic counselors help families with a history of brain tumors?
Genetic counselors are very important. They help figure out your risk of brain tumors. They guide you on genetic tests and offer support. They help you understand your risk and make health decisions.
What genetic testing is available for brain tumor susceptibility?
There are many genetic tests available. They look for specific mutations linked to brain tumor syndromes. These tests can spot high-risk individuals early, helping with monitoring and care.
What are the recommended screening protocols for families with a history of brain tumors?
Screening plans vary based on your risk and genetics. High-risk families might need regular MRI scans. They also get monitoring plans based on their risk.
Can lifestyle modifications reduce the risk of developing a brain tumor if there’s a family history?
While you can’t prevent brain tumors, some lifestyle changes might help. Reducing environmental toxins and staying healthy are good steps. Always talk to a doctor about these ideas.
How does a family history of brain cancer affect children?
Kids from families with brain cancer history might face higher risks. This is due to inherited genes. It’s a complex area, and families should talk to experts. They can learn about risks and screening for their kids.
What are the psychological impacts on families with a history of brain tumors?
A family history of brain tumors can be tough on the mind. It can lead to anxiety and stress. But, there are support groups and resources to help. They aim to balance awareness with a good quality of life.
Are there any ongoing clinical trials related to familial brain tumor genetics?
Yes, there are ongoing studies and trials. They aim to understand brain tumor genetics and find new treatments. These efforts could lead to better care for those at risk.
When should I consult a specialist about my family history of brain tumors?
If your family has a lot of brain tumors, see a neuro-oncology genetics specialist. They can check your risk, suggest tests, and guide you on managing your risk.
Reference
- Comelli, I., et al. (2017). Clinical presentation and epidemiology of brain tumors firstly diagnosed by emergency department. Journal of Neuro-Oncology, 132, 115-123. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5515810/