Last Updated on November 4, 2025 by mcelik

Nearly 2% of people will get a shoulder dislocation at some point. But, not all shoulder injuries are easy to spot. Many patients are misdiagnosed, which can cause delays in treatment and harm.
Diagnosing shoulder injuries is tricky. Many shoulder pain causes can look like a shoulder dislocation. This includes fractures, separations, and soft tissue injuries.
Getting the right diagnosis is key. It ensures the right treatment and avoids more problems.
Key Takeaways
- Shoulder injuries can be complex and difficult to diagnose.
- Misdiagnosis can lead to delayed treatment and long-term damage.
- Accurate diagnosis is critical for proper treatment.
- Various conditions can be mistaken for a dislocated shoulder.
- Fractures, separations, and soft tissue injuries are common shoulder injuries.
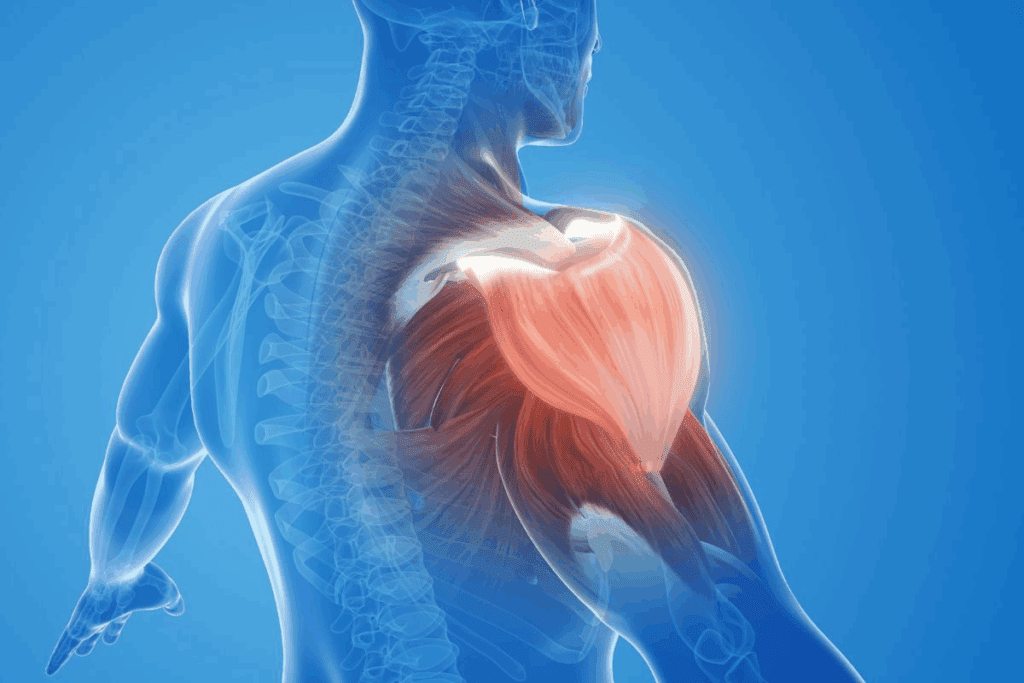
The Anatomy of the Shoulder Joint
Knowing the anatomy of the shoulder joint is key for diagnosing and treating injuries. The shoulder joint, or glenohumeral joint, is complex. It allows for a wide range of motion.
Basic Shoulder Structure and Components
The shoulder joint has several important parts: the humerus, scapula, and clavicle. The rotator cuff, made of muscles and tendons, helps stabilize the joint.
The shoulder is made of bones, ligaments, tendons, and muscles. These work together for movement. The glenohumeral ligaments are key for stability.
| Component | Function |
| Humerus | Upper arm bone that forms the shoulder joint |
| Scapula | Shoulder blade that provides attachment points for muscles |
| Clavicle | Collarbone that connects the arm to the body |
| Rotator Cuff | Group of muscles and tendons that stabilize the shoulder |
How the Shoulder Normally Functions
The shoulder works by balancing mobility and stability. It moves in many directions thanks to its components.
The rotator cuff muscles work together for smooth movement. The deltoid muscle is also important for shoulder movement.
What Makes the Shoulder Vulnerable to Injury
The shoulder is injury-prone due to its flexibility and constant stress. Overuse, trauma, and degenerative changes can lead to injuries.
Repetitive overhead movements, like throwing or lifting, can strain the shoulder. This makes it more likely to get injured.
True Shoulder Dislocations: Defining Characteristics
Knowing the details of a true shoulder dislocation is key for the right diagnosis and treatment. A shoulder dislocation happens when the upper arm bone, called the humerus, moves out of its socket. This can happen from falls, sports injuries, or car accidents.
Types of Shoulder Dislocations
Shoulder dislocations are divided by the direction of the bone’s movement. The most common is an anterior dislocation, where the bone moves forward. Posterior dislocations are less common and involve the bone moving backward. There’s also inferior dislocation, where the bone moves down.
Classic Symptoms of a Dislocated Shoulder
The signs of a dislocated shoulder are clear. People often feel a lot of pain and see their shoulder looks different. Other symptoms include:
- Swelling and bruising around the shoulder
- Feeling like the shoulder is loose or unstable
- Numbness or tingling from nerve damage
- Not being able to move the shoulder well
Immediate and Long-term Complications
Ignoring a dislocated shoulder can lead to serious problems. Right away, you might face nerve damage or blood vessel injuries. Later, you could deal with repeated dislocations, ongoing pain, and a less functional shoulder. You might also get osteoarthritis over time.
| Complication | Description | Potential Impact |
| Nerve Damage | Damage to the nerves around the shoulder | Numbness, tingling, or weakness in the arm or hand |
| Recurrent Dislocations | Repeated shoulder dislocations | Chronic instability and reduced function |
| Osteoarthritis | Wear and tear on the joint cartilage | Chronic pain and reduced mobility |
Conditions Mistaken for Dislocated Shoulder
Diagnosing shoulder injuries can be tricky because different conditions share similar symptoms. The shoulder’s complex anatomy and the variety of injuries make it easy to get it wrong.
Why Misdiagnosis Commonly Occurs
Misdiagnosis often happens because of similar symptoms in different shoulder conditions. Not getting a full medical history and the limits of imaging tests also play a role. For example, a shoulder sprain and a rotator cuff tear can look the same, making diagnosis hard without detailed checks and scans.
The shoulder joint is very complex, making it prone to many injuries. Conditions like shoulder subluxation and labral tear shoulder share symptoms, making diagnosis tricky.
The Importance of Accurate Diagnosis
Getting the diagnosis right is key to proper treatment and avoiding more harm. Wrong diagnoses can lead to the wrong treatment, making recovery longer and causing more damage. A correct diagnosis means the right treatment plan is followed, lowering the chance of problems.
Overview of Similar-Presenting Conditions
Many conditions can be mistaken for a dislocated shoulder because of similar symptoms. These include:
- Shoulder sprains and ligament injuries
- Rotator cuff tears
- Shoulder subluxation
- Labral tears
- Fractures around the shoulder complex
| Condition | Common Symptoms | Diagnostic Challenges |
| Shoulder Sprain | Pain, swelling, limited mobility | Differentiating from other injuries |
| Rotator Cuff Tear | Pain, weakness, limited mobility | Identifying the extent of the tear |
| Shoulder Subluxation | Pain, instability, apprehension | Distinguishing from complete dislocation |
Knowing about these conditions and their symptoms is key to accurate diagnosis and treatment. By understanding the similarities and differences, healthcare professionals can give better care to patients with shoulder injuries.
Shoulder Sprains and Ligament Injuries

Shoulder sprains and ligament injuries have symptoms similar to dislocations but are different. Knowing these differences is key for the right diagnosis and treatment.
Mechanism of Shoulder Sprains
A shoulder sprain happens when the ligaments around the shoulder joint get stretched or torn. This often occurs from falling onto an outstretched arm, a direct hit to the shoulder, or sudden twisting.
The severity of a sprain can range from mild to severe, based on the damage to the ligaments. Knowing the cause and how severe it is helps decide the best treatment.
Symptomatic Differences from Dislocations
While sprains and dislocations both cause pain and limited movement, they differ in symptoms. Dislocations usually result in a visible deformity and the arm is held in an odd position.
On the other hand, shoulder sprains don’t cause visible deformity but can lead to significant pain and swelling. Knowing these differences helps in making an accurate diagnosis.
Grading and Severity Levels
Shoulder sprains are graded based on their severity:
- Grade 1: Mild stretching or micro-tears of the ligament.
- Grade 2: Partial tearing of the ligament, resulting in some loss of function.
- Grade 3: Complete tear of the ligament, leading to significant instability.
Accurate grading is key for choosing the right treatment.
Treatment Approaches for Sprains
Treatment for shoulder sprains varies with the injury’s severity. Mild sprains might be treated with rest, ice, compression, and elevation (RICE), along with physical therapy to keep the range of motion and strength.
More severe sprains might need a sling to immobilize the shoulder or, in some cases, surgery to repair the ligaments. Rehabilitation is vital for recovery, aiming to restore function and prevent future injuries.
Rotator Cuff Tears and Injuries
Understanding rotator cuff tears is key to treating shoulder pain. The rotator cuff is a group of muscles and tendons around the shoulder. They keep the upper arm bone in the shoulder socket.
Rotator cuff injuries can be sudden or develop over time. They are a big reason for shoulder pain. These injuries can be mild strains or complete tendon tears.
Types of Rotator Cuff Damage
There are different types of rotator cuff damage:
- Tendinitis: inflammation of the tendons
- Tendinosis: degeneration of the tendons without significant inflammation
- Partial-thickness tears: tears that do not completely sever the tendon
- Full-thickness tears: tears that completely sever the tendon
Acute vs. Chronic Tear Symptoms
Symptoms of rotator cuff tears vary. Acute tears happen suddenly and cause sudden pain and weakness. Chronic tears develop slowly and lead to ongoing pain and weakness.
| Symptom | Acute Tear | Chronic Tear |
| Pain Onset | Sudden | Gradual |
| Weakness | Immediate | Progressive |
| Movement Limitation | Significant | Variable |
How Rotator Cuff Injuries Mimic Dislocations
Rotator cuff injuries can look like shoulder dislocations. Both can cause pain and limited movement. But, the cause and treatment are different.
Key differences: Dislocations move the bone out of the joint. Rotator cuff injuries damage the muscles and tendons around the joint.
Diagnostic Approaches
Diagnosing rotator cuff injuries needs a few steps. These include physical exams, patient history, and imaging. Diagnostic methods include:
- X-rays to rule out bone fractures
- MRI to see soft tissue damage
- Ultrasound to check tendon health
- Arthroscopy for direct look and treatment
By knowing about rotator cuff injuries and using the right tests, doctors can treat these common shoulder problems well.
Shoulder Subluxation: The Partial Dislocation
Shoulder subluxation is a complex condition that needs a deep understanding for proper management. It’s when the shoulder joint partially dislocates, but the humerus isn’t fully out of the socket.
Understanding Subluxation Mechanics
Subluxation can happen due to trauma, sports injuries, or repetitive strain. It’s caused by a disruption in the shoulder joint’s alignment, leading to instability. Knowing these mechanics is key to accurately diagnosing the condition.
Differences Between Subluxation and Complete Dislocation
The main difference between subluxation and complete dislocation is the extent of bone displacement. In subluxation, the bone is only partially out. In complete dislocation, it’s fully out. This affects symptoms and treatment options.
Recurrent Subluxation Patterns
Recurrent subluxation can become a long-term problem if not managed well. The frequency of recurrence varies based on the injury’s severity, shoulder health, and treatment success.
Treatment and Management Options
Treatment for shoulder subluxation may include physical therapy, bracing, and sometimes surgery. The aim is to stabilize the shoulder joint and prevent future subluxations. Making lifestyle changes is also part of the management plan.
Effective management of shoulder subluxation requires a detailed approach. It must address both symptoms and underlying causes. Healthcare providers can create specific treatment plans by understanding subluxation mechanics and its differences from complete dislocation.
Fractures Around the Shoulder Complex
It’s important to know about fractures around the shoulder. The shoulder area has bones like the humerus, clavicle, and scapula. These bones can break, and it’s key to tell the difference between a break and a dislocated shoulder.
Proximal Humerus Fractures
A proximal humerus fracture happens near the shoulder joint. It’s more common in older adults. It can happen from falling onto the shoulder or arm. Symptoms include pain, swelling, and trouble moving.
Clavicle (Collarbone) Fractures
Clavicle fractures are common, mainly in kids and teens. They often happen from falling onto the shoulder or arm. Symptoms include pain, swelling, and a visible deformity along the clavicle.
Scapular (Shoulder Blade) Fractures
Scapular fractures are rare and usually from big accidents. They can come with other injuries and need a detailed check-up.
Distinguishing Fractures from Dislocations
Telling fractures from dislocations is key for the right treatment. Both can hurt a lot and make it hard to move. But they need different care. Here’s a table to show the main differences:
| Characteristics | Fractures | Dislocations |
| Pain Location | Localized to the fracture site | Often around the joint |
| Deformity | May have visible deformity or bone fragments | Visible deformity with the bone out of place |
| Mobility | Limited due to pain and instability | Limited due to pain and mechanical obstruction |
| Diagnostic Tool | X-rays, CT scans | X-rays, sometimes CT or MRI |
Getting the right diagnosis is critical for the right treatment. Knowing the difference between fractures and dislocations is important for both patients and doctors.
Labral Tears and SLAP Lesions
Understanding labral tears and SLAP lesions is key for diagnosing and treating shoulder injuries. The labrum is a cartilage around the shoulder joint socket. It helps keep the shoulder stable and moving smoothly.
Function of the Shoulder Labrum
The shoulder labrum is a cartilage ring around the glenoid socket. It deepens the socket, making it fit better for the humeral head. This is important for stability, mainly during movements and overhead activities.
The labrum also helps attach ligaments and tendons. This adds to the joint’s stability.
Types and Causes of Labral Injuries
Labral tears can happen from trauma, strain, or aging. SLAP lesions are a specific type of tear affecting the labrum’s top part. These are common in athletes doing overhead sports like baseball or tennis.
Causes of labral tears include:
- Traumatic injuries, such as falls or direct blows to the shoulder
- Repetitive strain injuries, often seen in athletes with overhead throwing motions
- Degenerative changes, which can occur with aging
Symptoms That Overlap with Dislocations
Labral tears and SLAP lesions share symptoms with shoulder dislocations. These include pain, weakness, and limited motion. Some people might feel their shoulder catching or locking.
These similar symptoms make diagnosis hard. A detailed check-up and imaging studies are needed for a correct diagnosis.
Diagnostic Challenges and Solutions
Diagnosing labral tears and SLAP lesions is tricky. Symptoms are not specific, and the shoulder joint is complex. A thorough approach includes a patient history, physical exam, and imaging like MRI or CT arthrography.
Diagnostic arthroscopy might be needed to confirm the diagnosis. Treatment plans are then made based on the injury’s severity, symptoms, and activity level.
Inflammatory Conditions: Bursitis and Tendonitis
Understanding bursitis and tendonitis in the shoulder is key to treating them right. These conditions can cause a lot of pain and discomfort. They can even feel like more serious injuries like dislocations.
Mechanisms and Symptoms of Shoulder Bursitis
Shoulder bursitis happens when the bursae, small fluid-filled sacs, get inflamed. This can be due to repetitive motion, direct trauma, or infection. Symptoms include pain, swelling, and limited mobility.
The bursae help reduce friction between bones, tendons, and skin around the shoulder. When they’re inflamed, it can be very uncomfortable. This can affect your daily activities and sleep.
Common Tendonitis Patterns in the Shoulder
Tendonitis is when the tendons, which connect muscles to bones, get inflamed. In the shoulder, it often affects the rotator cuff tendons. It can be caused by repetitive strain, aging, or sudden injury. Symptoms include pain during movement, tenderness, and mild swelling.
Tendonitis can make it hard to do everyday activities. Knowing the causes and symptoms is important for managing it well.
Distinguishing Inflammatory vs. Traumatic Pain
It’s important to tell the difference between inflammatory and traumatic pain. Inflammatory pain, like in bursitis and tendonitis, comes on slowly and gets worse with movement. It may also have swelling or redness. Traumatic pain, on the other hand, happens suddenly after an injury and is sharp.
| Characteristics | Inflammatory Pain | Traumatic Pain |
| Onset | Gradual | Sudden |
| Nature of Pain | Dull, aching | Sharp, intense |
| Associated Symptoms | Swelling, redness | Immediate loss of function |
Conservative Treatment Approaches
For conditions like bursitis and tendonitis, rest, ice, compression, and elevation (RICE) are recommended. Anti-inflammatory medications can also help. Physical therapy is beneficial for keeping the shoulder moving and strengthening the muscles.
In some cases, corticosteroid injections may be suggested to reduce inflammation. Making lifestyle changes, like avoiding repetitive motions and improving posture, can also help manage symptoms and prevent them from coming back.
Frozen Shoulder (Adhesive Capsulitis)
Frozen shoulder makes the shoulder joint stiff and painful. It limits how much you can move it. This condition, also known as adhesive capsulitis, goes through several stages.
The Three Stages of Frozen Shoulder
Frozen shoulder goes through three stages: freezing, frozen, and thawing. In the freezing stage, the shoulder gets stiffer and more painful. It’s harder to move during this stage, which can last months.
The frozen stage sees a big drop in the shoulder’s range of motion. The pain might lessen a bit, but stiffness stays, making daily tasks tough. The thawing stage slowly improves mobility and reduces stiffness. This stage can last from months to years.
Primary Risk Factors and Causes
Several factors can raise your risk of getting frozen shoulder. These include:
- Diabetes
- Immobilization due to injury or surgery
- Inflammatory conditions such as arthritis
- Previous shoulder injuries or conditions
Knowing these risk factors helps with early diagnosis and treatment.
Distinctive Movement Limitations vs. Dislocations
Frozen shoulder is different from a dislocated shoulder. A dislocated shoulder means the bone is out of place. But frozen shoulder is caused by inflammation and scarring around the joint. The main symptom is a big drop in movement without the bone being out of place.
Dislocations cause an immediate loss of function because of the bone’s position. But frozen shoulder gets stiffer over time.
Treatment Timeline and Expectations
Treatment for frozen shoulder aims to improve mobility and reduce pain. Recovery time varies, often taking months to years. Treatments include physical therapy, pain meds, and sometimes surgery to loosen tight tissues.
Getting treatment early can greatly improve your outcome. It’s key to see a doctor if symptoms don’t go away.
Nerve Compression Syndromes Affecting the Shoulder
It’s important to know about nerve compression syndromes to treat shoulder pain. When a nerve gets compressed, it can’t work right. This leads to pain, numbness, or weakness. The shoulder, with its many nerves, is prone to these issues.
Thoracic Outlet Syndrome
Thoracic outlet syndrome (TOS) happens when nerves and blood vessels get squished. It causes shoulder and arm pain, numbness, and weakness. TOS can be hard to diagnose because its symptoms are similar to other shoulder problems.
“Diagnosing TOS is tricky,” says a doctor. “It needs a detailed check-up to rule out other shoulder pain causes.” Doctors use physical exams, imaging, and sometimes nerve tests to figure it out.
Cervical Radiculopathy and Referred Pain
Cervical radiculopathy is when a nerve in the neck gets hurt. It can cause pain in the shoulder and arm. This makes it hard to tell it apart from other shoulder issues. The key to diagnosing it is to look at the pain pattern and match it with imaging results.
Brachial Plexus Injuries and Presentations
The brachial plexus is a group of nerves from the spinal cord to the arm. Injuries here can cause weakness or even paralysis. Getting a correct diagnosis of brachial plexus injuries needs a detailed check-up and imaging like MRI.
Neurological Testing for Differential Diagnosis
Neurological tests are key in diagnosing nerve issues. Tests like EMG and NCS check how nerves work and find compression spots. These tests help tell nerve compression syndromes apart from other shoulder problems.
In summary, nerve compression syndromes in the shoulder are complex. They need a deep understanding for right diagnosis and treatment. By using clinical checks, imaging, and nerve tests, doctors can create treatment plans that fit each patient’s needs.
Diagnostic Methods for Shoulder Conditions
To find out why someone has shoulder pain, doctors use different ways to diagnose. Getting the right diagnosis is key to treating and healing the shoulder.
Physical Examination Techniques
A detailed physical check is the first step in finding out what’s wrong with the shoulder. Doctors use many methods to see how well the shoulder moves, how strong it is, and where it hurts. They look for:
- Visible signs of damage or swelling
- How well the shoulder can move and if it’s stiff
- Weakness in the muscles
- Pain when touching the shoulder area
These checks help doctors guess what might be wrong and decide on more tests.
Imaging Options: X-rays, MRI, CT, and Ultrasound
Imaging tests are very important for diagnosing shoulder problems. Each type of test shows different things about the shoulder’s structure and any problems.
X-rays are often the first choice, showing bones clearly and spotting breaks or dislocations. MRI (Magnetic Resonance Imaging) is great for seeing soft tissues like tendons and cartilage. It’s best for finding tears in the rotator cuff and other soft tissue issues. CT (Computed Tomography) scans show both bones and soft tissues, helping find complex fractures and other problems. Ultrasound lets doctors see tendons and soft tissues in real-time, which is good for checking the rotator cuff.
Specialized Tests for Specific Conditions
There are also special tests for certain shoulder problems. These tests try to make symptoms appear or check specific parts of the shoulder. Some examples are:
- The apprehension test for shoulder instability
- The Neer test and Hawkins-Kennedy test for impingement syndrome
- The drop arm test for rotator cuff tears
- The O’Brien test for labral lesions
These tests, along with other methods, help doctors make sure they have the right diagnosis.
When Diagnostic Arthroscopy Is Necessary
Diagnostic arthroscopy is a small surgery that lets doctors see inside the shoulder joint. It’s usually needed when other tests don’t give a clear answer or when surgery is planned. It’s very useful for:
- Looking at labral tears or SLAP lesions
- Checking for cartilage damage or osteoarthritis
- Finding loose bodies in the joint
- Examining the rotator cuff and nearby areas
Arthroscopy not only helps find the problem but also lets doctors fix it right away. This makes it a key tool for treating tough shoulder problems.
When to Seek Medical Attention for Shoulder Pain
If you’re feeling shoulder pain, it’s important to know when to see a doctor. Shoulder pain can come from many things, like small injuries or serious problems that need quick medical help.
Red Flag Symptoms Requiring Immediate Care
Some symptoms with shoulder pain mean you should see a doctor right away. These red flag symptoms include:
- Severe pain that doesn’t get better with rest
- Swelling, bruising, or deformity around the shoulder
- Can’t move the shoulder or arm
- Numbness, tingling, or weakness in the arm or hand
- Shoulder pain after a fall or direct hit
Doctors say it’s very important to see a doctor fast if you have these symptoms. This is to check for serious problems like fractures or dislocations.
“Early diagnosis and treatment can significantly improve outcomes for patients with shoulder injuries.”
Distinguishing Emergency vs. Non-Emergency Situations
It’s important to know if your shoulder pain is an emergency or not. Some pain can be treated without seeing a doctor, but others need quick help. Think about how bad the pain is, if you have red flag symptoms, and how it affects your daily life.
What to Expect During Medical Evaluation
When you see a doctor for shoulder pain, they will check you physically, ask about your health history, and might do tests like X-rays or MRIs. This helps find out why you’re in pain and what to do next.
A detailed medical check is key to finding the right treatment. Knowing why you’re in pain helps doctors suggest the best treatments. This could be physical therapy, medicine, or surgery.
Self-Care Measures While Awaiting Treatment
While waiting to see a doctor, there are things you can do to help with your pain. Try using ice to reduce swelling, take over-the-counter pain meds, and avoid things that make the pain worse. But remember, these are just temporary fixes and not a replacement for professional advice.
It’s very important to follow up with a healthcare provider to get the right diagnosis and treatment. This way, you can avoid making the problem worse and have a better chance of getting better.
Conclusion
Understanding shoulder injuries is key to getting the right treatment. Many conditions can look like a dislocated shoulder, making it hard to diagnose. A detailed check-up, including physical exams and imaging, is needed to find the cause of pain.
Getting the right treatment starts with knowing the exact injury. This could be a sprain, a rotator cuff tear, or something else. Knowing what’s wrong helps doctors create a good plan to fix it. Staying strong and flexible in the shoulder can also help avoid injuries in the future.
Seeing a doctor when pain doesn’t go away is important. This ensures you get the right care for your injury. Taking care of your shoulder health can lead to better results and less chance of lasting damage.
FAQ
What are the common conditions mistaken for a dislocated shoulder?
Shoulder sprains, rotator cuff tears, and shoulder subluxation are often mistaken for a dislocated shoulder. Other conditions include fractures, labral tears, bursitis, tendonitis, frozen shoulder, and nerve compression syndromes.
How can a shoulder sprain be differentiated from a dislocation?
Shoulder sprains cause pain and swelling but the joint stays in place. A dislocated shoulder has the humerus out of the socket. Imaging and physical exams can tell them apart.
What are the symptoms of a rotator cuff tear that might be confused with a dislocated shoulder?
Rotator cuff tears cause pain, weakness, and limited mobility. They are mistaken for dislocated shoulder symptoms. But, they don’t involve the humerus moving out of the socket.
Can a shoulder subluxation be considered a partial dislocation?
Yes, a shoulder subluxation is a partial dislocation. The humerus is only partially out of the socket. It causes instability and pain, and may happen again.
How can fractures around the shoulder be distinguished from dislocations?
Fractures around the shoulder can be told apart from dislocations with X-rays or CT scans. These tests show if there’s a fracture.
What is the role of the labrum in the shoulder joint, and how can labral tears be diagnosed?
The labrum is a cartilage ring that helps keep the shoulder stable. Labral tears are diagnosed with physical exams, MRI, and arthroscopy.
How can inflammatory conditions like bursitis and tendonitis be differentiated from traumatic injuries?
Bursitis and tendonitis cause pain, swelling, and warmth without trauma. Ultrasound or MRI can confirm inflammation.
What are the stages of frozen shoulder, and how can it be treated?
Frozen shoulder goes through three stages: freezing, frozen, and thawing. Treatment includes physical therapy, pain management, and sometimes injections or manipulation under anesthesia.
How can nerve compression syndromes affecting the shoulder be diagnosed?
Nerve compression syndromes are diagnosed with physical exams, neurological tests, and imaging like MRI or electromyography.
When should I seek medical attention for shoulder pain?
Seek medical help for severe pain, swelling, or deformity. Also, if moving your arm or shoulder is hard. Look out for numbness, tingling, or weakness in your arm or hand.
References
Skillgate, E., Leden, I., & Blomgren, J. (2020). Effectiveness of deep tissue massage therapy and combined treatments for musculoskeletal pain. European Journal of Pain Management, 24(3), 355-363. https://www.sciencedirect.com/science/article/pii/S2468781219302036





