Nearly 1 in 5 patients face complications after orthopedic surgeries, studies show. This highlights the need to know the risks involved.
Orthopedic surgical procedures are often needed but come with inherent risks and postoperative concerns. It’s key for both patients and healthcare providers to understand these surgical risks.
Looking into the possible complications and risks helps people make better choices about their health care.
Key Takeaways
- Orthopedic surgeries carry significant risks and possible complications.
- Knowing these risks is vital for making informed decisions.
- Good postoperative care is important to reduce surgical risks.
- Assessing surgical risks helps in planning the right care.
- Patients should talk about their worries with healthcare providers.
Understanding Orthopedic Surgery

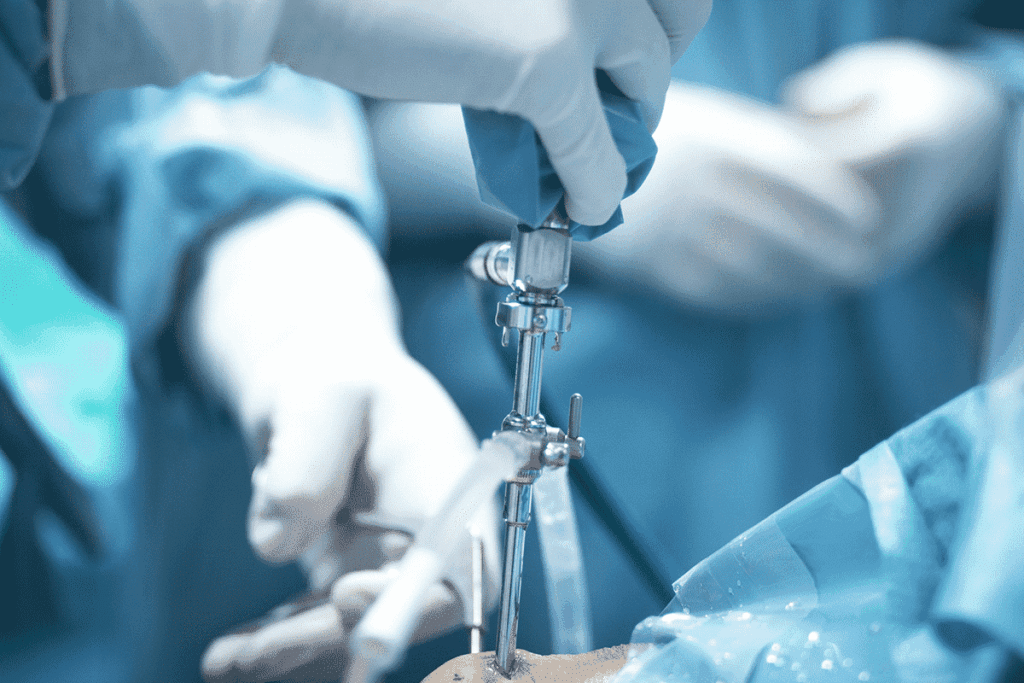
Orthopedic surgery deals with many types of musculoskeletal issues. It includes joint replacements and fracture repairs. This knowledge is key to understanding these surgeries.
Common Types of Orthopedic Procedures
Orthopedic surgeries are divided into several types. They target different areas of the body. Here are some common ones:
- Joint replacement surgeries (e.g., hip, knee, shoulder)
- Fracture repair surgeries
- Soft tissue surgeries (e.g., tendon and ligament repairs)
- Osteotomy (cutting and realigning bones)
Each procedure is chosen based on the patient’s condition. Surgeons use their expertise to decide the best option.
When Orthopedic Surgery Is Necessary
Surgery is needed when other treatments fail. The decision to have surgery comes after careful evaluation. This includes diagnostic tests and a review of the patient’s medical history.
| Condition | Common Surgical Intervention |
| Severe joint degeneration | Joint replacement surgery |
| Fractures | Fracture repair surgery |
| Tendon and ligament tears | Soft tissue repair surgery |
Knowing when and what type of surgery is needed helps patients make better choices. It’s about understanding their treatment options.
Orthopedic Surgery Risks: An Overview
Orthopedic surgeries carry risks that are important to know. These surgeries fix many musculoskeletal problems, like joint replacements and fracture repairs. Even though they can greatly improve life quality, they might have complications.
Statistical Analysis of Complication Rates
Studies give us insight into how often complications happen in orthopedic surgeries. The rates can change a lot based on the surgery type, the patient’s health, and other factors.
| Surgery Type | Complication Rate (%) | Common Complications |
| Hip Replacement | 5-10 | Infection, Dislocation, Deep Vein Thrombosis |
| Knee Replacement | 5-15 | Infection, Implant Loosening, Stiffness |
| Shoulder Replacement | 3-8 | Infection, Implant Failure, Limited Mobility |
The data shows that while complications can happen, they are usually not too common for most surgeries.
Comparing Risks to Benefits
It’s key to think about the risks and benefits of orthopedic surgery. For many, the surgery’s benefits, like less pain and better movement, are worth the risks.
- Significant pain reduction
- Improved joint function and mobility
- Enhanced quality of life
Even with risks, knowing them and taking steps to prevent them can make surgery outcomes better.
Anesthesia-Related Risks in Orthopedic Procedures
Anesthesia in orthopedic surgeries is key but comes with risks. It helps manage pain during surgery. Knowing these risks is important for patients.
General vs. Regional Anesthesia
Orthopedic surgeries use general or regional anesthesia. General anesthesia makes you unconscious for complex surgeries. Regional anesthesia, like epidurals, numbs a part of your body. It’s safer and manages pain well.
- General Anesthesia Risks: Includes respiratory and cardiac complications.
- Regional Anesthesia Benefits: Less risk of nausea and vomiting, and allows for faster recovery.
Potential Complications and Prevention
Anesthesia complications are rare but serious. They can include nerve damage, allergic reactions, and breathing problems. To prevent these, doctors evaluate patients before surgery, monitor them during, and care for them after.
- Careful selection of anesthesia type based on patient health and surgical requirements.
- Continuous monitoring of vital signs during surgery.
- Post-operative care to manage pain and monitor for complications.
Knowing about anesthesia risks in orthopedic surgeries helps patients make better choices. Talking to your doctor about these risks prepares you for a safe surgery.
Infection Risk Following Orthopedic Surgery
The risk of infection after orthopedic surgery is a big worry for doctors and patients. These surgeries can greatly improve life but also bring the chance of infections. These infections can make recovery harder and affect the outcome.
Surgical Site Infections
Surgical site infections (SSIs) are a big worry in orthopedic surgery. These infections can happen at the incision site or deeper in the tissue or organ. SSIs can cause longer hospital stays, more surgeries, and higher healthcare costs.
Things that make SSIs more likely include:
- Prolonged surgical time
- Poor wound care
- Patient health issues like diabetes
- Smoking
Osteomyelitis and Bone Infections
Osteomyelitis is a bone infection that can happen after orthopedic surgery. It’s when the bone tissue gets inflamed, usually from bacteria. Treating osteomyelitis can be hard and may need long antibiotic treatment or more surgery.
Symptoms of osteomyelitis include:
- Persistent pain
- Swelling and redness at the surgical site
- Fever
Infection Prevention Strategies
Stopping infections is a key goal in orthopedic surgery. Several steps are taken to lower the risk of SSIs and other infections:
- Preoperative Antibiotics: Giving antibiotics before surgery to cut down bacteria.
- Sterile Technique: Keeping the surgery area clean to avoid contamination.
- Postoperative Wound Care: Making sure wound care is done right and watching for infection signs.
By knowing the risks and using these prevention steps, infections after orthopedic surgery can be greatly reduced.
Blood Clot and Circulatory Complications
When planning orthopedic surgery, patients and surgeons must consider blood clot and circulatory risks. These issues can stem from prolonged rest, surgery trauma, and individual health factors.
Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis is when a blood clot forms in deep veins, often in the legs. It’s serious because it can cause pulmonary embolism if the clot moves to the lungs. Signs include swelling, pain, and redness in the affected leg.
Risk Factors for DVT
- Prolonged immobilization
- Major surgery, like orthopedic procedures
- History of DVT or pulmonary embolism
- Cancer and other chronic conditions
Pulmonary Embolism Risk
Pulmonary embolism happens when a blood clot travels to the lungs. It’s life-threatening and needs quick medical help. Symptoms include sudden breathlessness, chest pain, and coughing up blood.
Preventing Pulmonary Embolism is key. This can be done by managing DVT risk factors, using blood thinners, and using devices like compression stockings.
Preventive Measures and Treatments
Preventing blood clots and circulatory issues requires a variety of steps. These include blood thinners, mechanical devices, and moving early after surgery.
| Preventive Measure | Description | Benefits |
| Anticoagulant Medications | Medications that prevent blood clot formation | Reduces the risk of DVT and pulmonary embolism |
| Mechanical Prophylaxis | Use of compression stockings and IPC devices | Enhances blood flow, reducing clot risk |
| Early Mobilization | Encouraging patients to move and exercise post-surgery | Improves circulation, reduces clot risk |
In summary, knowing the risks of blood clots and circulatory problems is vital in orthopedic surgery. By using preventive steps and understanding risks, patients and doctors can work together to avoid these issues.
Nerve Damage and Neurological Complications
Orthopedic surgery can sometimes lead to nerve injury. This causes significant neurological complications. Both surgeons and patients must consider this risk.
Common Causes of Nerve Injury
Nerve injury during orthopedic surgery can happen for several reasons. These include direct trauma, compression, or stretching of nerves. The risk is higher in surgeries that involve complex nerve networks.
The chance of nerve damage varies with the surgery type. For example, spine or major joint surgeries like the hip or knee have different risks.
Symptoms and Long-term Effects
Symptoms of nerve damage can range from mild numbness or tingling to severe pain or weakness. Some patients may face long-term neurological deficits.
| Symptom | Description | Potential Long-term Effect |
| Numbness | Loss of sensation in the affected area | Permanent sensory loss |
| Tingling | A pins-and-needles sensation | Chronic discomfort |
| Weakness | Reduced muscle strength | Muscle atrophy |
It’s important for patients to understand these risks and their long-term effects. This helps them make informed decisions about their surgery.
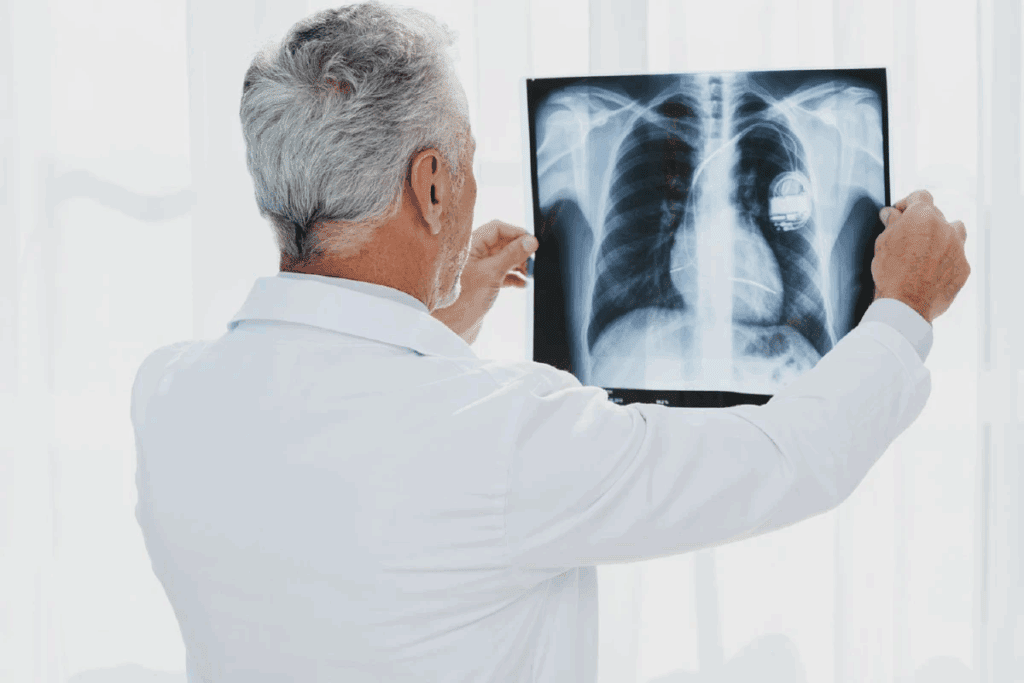
Hardware and Implant Complications
Orthopedic surgery often uses implants and hardware. These tools help fix bones and joints. But, they can also cause problems.
Implant Failure and Loosening
Implant failure or loosening is a big worry. Implant failure can happen for many reasons. This includes mechanical stress, wrong placement, or bone quality issues.
- Mechanical stress and wear and tear over time
- Inadequate implantation technique
- Poor bone quality or osteoporosis
Loosening can be due to infection, bad initial fix, or bone loss around the implant.
Hardware Rejection and Allergic Reactions
Rejection or allergic reactions to hardware are serious risks. These issues are rare but can cause a lot of harm.
“Metal sensitivity and allergic reactions to orthopedic implants, though rare, are key in patient prep for surgery.” – a Journal
Common metals in implants are titanium, stainless steel, and cobalt-chromium. While safe for most, some may react to these metals.
Revision Surgery Necessity and Risks
When implants fail, loosen, or get rejected, revision surgery might be needed. This second surgery is usually harder than the first.
Revision surgery risks include:
- Higher chance of infection
- More blood loss and longer surgery
- Possible nerve damage or fracture
Even with these risks, revision surgery is sometimes necessary. It helps fix problems and improve patient health. Good planning and care after surgery can reduce these risks.
Joint Replacement Specific Risks
Joint replacement surgeries can change lives but come with risks. These surgeries aim to ease pain and improve joint function. But, they can lead to complications that differ by joint.
Hip Replacement Complications
Hip replacement surgeries are common and generally safe. Yet, they can lead to dislocation and infection. These issues can be serious and may need more surgery.
“Following post-operative instructions can help avoid dislocation,” an orthopedic specialist says. “Knowing the risks and taking steps to prevent them can greatly improve results.”
- Dislocation
- Infection
- Nerve damage
Knee Replacement Complications
Knee replacement surgeries are also common and often successful. But, they can face complications like infection, blood clots, and implant loosening. This happens when the artificial parts of the knee become unstable over time.
To lower these risks, patients are advised on post-operative care. This includes physical therapy and watching for signs of complications.
| Complication | Description | Prevention |
| Infection | Bacterial infection at the surgical site | Antibiotics, proper wound care |
| Blood Clots | Clot formation in the legs | Anticoagulants, mobilization |
Shoulder Replacement Complications
Shoulder replacement surgeries are less common but have risks. These include instability, nerve injury, and implant failure. These issues can stem from the shoulder’s complex anatomy and the high demands on it.
It’s vital to have careful surgical planning and post-operative rehabilitation. This helps reduce these risks.
Spinal Surgery Risks and Complications
Patients thinking about spinal surgery need to know about possible complications. This helps them make smart choices about their health. Different surgeries, like disc surgery and spinal fusion, have their own risks.
Disc Surgery Complications
Disc surgery aims to ease nerve pressure from herniated or damaged discs. But, it can lead to problems like infection, nerve damage, and cerebrospinal fluid leaks. Sometimes, the disc can bulge again, needing more surgery.
Nerve damage is a big worry. It can cause numbness, weakness, or ongoing pain. Choosing a skilled surgeon is key to avoid this.
Spinal Fusion Risks
Spinal fusion joins two or more vertebrae together. But, it has risks like nonunion or pseudoarthrosis, where the bones don’t fuse right. There’s also a chance of hardware failure and faster wear of nearby vertebrae.
| Complication | Description | Prevention/ Management |
| Nonunion/Pseudoarthrosis | Failure of the bones to fuse | Use of bone grafts, careful patient selection |
| Hardware Failure | Breakage or loosening of implanted hardware | High-quality hardware, proper implantation technique |
| Adjacent Segment Disease | Degeneration of vertebrae adjacent to the fusion site | Careful surgical planning, post-operative care |
Failed Back Surgery Syndrome
Failed back surgery syndrome (FBSS) is when pain persists or comes back after surgery. It can be due to bad surgery, not fixing the real problem, or new issues.
“Failed back surgery syndrome is a complex condition that requires a thorough treatment plan, often involving a team of healthcare experts.”
A Neurosurgeon
Dealing with FBSS is tough. It might need more surgery, pain management, or other treatments like spinal cord stimulation.
Knowing the risks of spinal surgery is vital for patients and doctors. This knowledge helps patients make better choices, and doctors can reduce risks.
Fracture Repair Complications
Fracture repair surgery is a common procedure in orthopedics. It’s generally safe but can have risks. These complications can affect recovery and the final result.
Delayed or Non-union Healing
Delayed or non-union healing is a big risk. This means the bone heals slowly or not at all. The severity of the fracture, patient health, and surgery method play a role.
Risk Factors for Delayed Healing
- Infection
- Poor blood supply
- Smoking
- Diabetes
Malunion Issues
Malunion happens when a fracture heals wrong, causing bone misalignment. This can make it hard to move and might need more surgery to fix.
Causes of Malunion
- Inadequate reduction during surgery
- Insufficient immobilization
- Premature weight-bearing
Hardware Problems in Fracture Fixation
Hardware like plates and screws can cause issues. These problems include failure, loosening, or reactions to the materials.
| Hardware Complication | Description | Potential Solution |
| Hardware Failure | Breakage of the implanted device | Revision surgery |
| Loosening | Implant becomes loose over time | Revision surgery or additional stabilization |
| Adverse Reaction | Allergic reaction or sensitivity to implant material | Removal of the implant or use of alternative materials |
It’s important for both doctors and patients to know about these risks. Understanding them can help improve the chances of a good outcome.
Age-Related Risk Factors in Orthopedic Surgery
Age affects the risks of orthopedic surgery in many ways. This is true for people of all ages, from kids to seniors. Knowing these age-related factors is key to reducing risks and improving results.
Pediatric Considerations
Children often need orthopedic surgery for birth defects or injuries. The risks depend on the child’s health, the condition being treated, and the surgery method.
Key considerations for pediatric orthopedic surgery include:
- The risk of growth problems after surgery
- The need for careful planning and execution to avoid complications
- The importance of post-operative care and rehabilitation tailored to the child’s needs
A study in a medical journal noted, “The success of pediatric orthopedic surgery depends on a multidisciplinary approach. This includes careful preoperative planning, meticulous surgical technique, and thorough postoperative care.”
“Pediatric orthopedic surgery requires a nuanced understanding of the child’s musculoskeletal development and the long-term implications of surgical interventions.”
Elderly Patient Risks
Elderly patients face unique challenges in orthopedic surgery. They often have conditions like diabetes, heart disease, and osteoporosis. These can make surgery and recovery harder, needing a detailed preoperative check-up.
| Comorbidity | Impact on Orthopedic Surgery | Management Strategy |
| Diabetes | Increased risk of infection and delayed healing | Tight blood glucose control pre- and post-operatively |
| Heart Disease | Increased risk of cardiovascular complications | Cardiac evaluation and monitoring during surgery |
| Osteoporosis | Poor bone quality affecting implant stability | Use of bone-strengthening medications and careful implant selection |
Osteoporosis and Bone Quality Concerns
Osteoporosis is a big worry in orthopedic surgery, mainly for older patients. Poor bone quality can make implants unstable and surgery less successful.
Osteoporosis management strategies include:
- The use of medications to strengthen bones
- Careful selection of orthopedic implants designed for osteoporotic bone
- Modification of surgical techniques to accommodate poor bone quality
By understanding and addressing these age-related risk factors, healthcare providers can better manage the risks associated with orthopedic surgery. This leads to better outcomes for patients of all ages.
Chronic Pain and Long-term Complications
Orthopedic surgery aims to reduce pain and improve function. Yet, some patients face chronic pain and long-term issues. Chronic pain lasts longer than expected healing times. It can greatly affect a patient’s life quality.
Post-Surgical Pain Syndromes
Post-surgical pain syndromes are chronic pain conditions that start after surgery. They can stem from nerve damage, scar tissue, or the body’s reaction to surgery. Effective pain management strategies are vital to lower the risk of chronic pain syndromes.
“Chronic pain is a complex condition that requires a multifaceted treatment approach,” notes a leading pain management specialist. “Understanding the underlying causes and tailoring treatment to the individual’s needs is key to successful management.”
Joint Stiffness and Mobility Issues
Joint stiffness and mobility problems are common after orthopedic surgery. These can come from the surgery, post-operative immobilization, or the condition that led to surgery. Early mobilization and physical therapy are key to preventing or reducing these issues.
- Range of motion exercises can help maintain flexibility.
- Strengthening exercises support the joint and improve function.
- Physical therapy modalities, such as heat or electrical stimulation, can aid in recovery.
Psychological Impact of Chronic Pain
Chronic pain can deeply affect a person’s mind, leading to depression, anxiety, and a lower quality of life. The ongoing nature of chronic pain can be very hard to deal with. It can make it hard to do daily tasks. A complete treatment plan that includes mental health support is vital for patients with chronic pain.
“The psychological burden of chronic pain should not be underestimated. It requires a compassionate and multidisciplinary approach to care.”
Recovery Complications and Rehabilitation Risks
Recovery and rehabilitation after orthopedic surgery can face many challenges. It’s key to manage these issues well to ensure a good outcome.
Physical Therapy Challenges
Physical therapy is vital after surgery. But, some patients struggle to keep up due to pain or lack of motivation. Following physical therapy plans is important to regain strength and function.
Some might feel more pain during therapy, which can slow progress. Healthcare providers must watch how patients react and adjust the therapy as needed.
Delayed Recovery Issues
Delayed recovery can happen for many reasons, like infection or poor bone quality. Finding out why is the first step to fix the problem.
Patients who recover slowly might feel frustrated or depressed. They need strong support from doctors, family, and friends.
Return to Activity Complications
Going back to activities too fast can cause injuries or overuse. Slowly getting back to normal is safer.
Patients should always follow post-operative instructions and talk to their doctor before starting hard activities or sports.
Minimizing Orthopedic Surgery Risks
To lower the risks of orthopedic surgery, a detailed plan is needed. This includes getting ready for surgery, choosing skilled surgeons, and following doctor’s orders. By taking these steps, patients can greatly improve their surgery results.
Pre-surgical Preparation and Optimization
Getting ready for surgery is key to avoiding risks. Doctors check the patient’s health, like managing diabetes and high blood pressure. They also look at nutrition to help with healing.
Patients are told to stop smoking and not take certain medicines. A checklist from the healthcare team helps make sure everything is done right before surgery.
Surgeon Experience and Hospital Quality
The surgeon’s skill and the hospital’s quality matter a lot. Surgeons with lots of experience do better because they know their craft well. They can handle problems better too.
It’s also important to pick a hospital that cares a lot about quality and keeps infections away. Hospitals with great orthopedic care and teams can help from start to finish.
Patient Compliance with Instructions
Following the doctor’s orders is very important. This means taking medicine, going to therapy, and following care instructions. Being active in your recovery helps avoid problems and leads to better results.
By focusing on preparation, choosing the right surgeon and hospital, and following instructions, patients can greatly reduce surgery risks. This leads to a successful recovery.
When to Seek Medical Attention Post-Surgery
Knowing when to seek medical help after surgery is key for a good recovery. After orthopedic surgery, it’s important to watch your health closely. Look out for signs that mean you need to see a doctor.
Warning Signs of Complications
There are several signs that might mean you’re facing complications after surgery. These include:
- Increasing pain not managed by prescribed medication
- Swelling, redness, or warmth around the surgical site
- Fever or chills
- Difficulty moving the affected limb or joint
- Numbness or tingling sensations
Knowing these signs can help you act fast.
Emergency Situations Requiring Immediate Care
Some situations need you to get medical help right away. These include:
- Severe pain or swelling
- Signs of infection such as redness, warmth, or pus
- Shortness of breath or difficulty breathing
- Chest pain or pressure
- Severe headache or confusion
Follow-up Care Importance
Getting regular check-ups after surgery is very important. It lets doctors keep an eye on how you’re healing. They can catch any problems early and change your treatment if needed.
At these check-ups, talk about any worries or symptoms you have. This helps doctors spot issues early and make sure you get the right care.
Conclusion: Weighing the Risks and Benefits of Orthopedic Surgery
Orthopedic surgery can greatly improve life for those with musculoskeletal issues. We’ve looked at common surgeries, risks, and complications in this article.
It’s key to think about the risks and benefits of surgery. While problems can happen, many patients find the benefits worth it. Knowing the risks and benefits helps in making smart health choices.
Knowing the risks, like infections or nerve damage, helps patients reduce them. They can follow pre-surgery steps, pick a skilled surgeon, and follow post-op advice.
Deciding on surgery needs careful thought of risks and benefits. Talking to a healthcare provider is important to find the right treatment. Weighing risks and benefits is a big part of making informed surgery choices.
FAQ
What are the most common risks associated with orthopedic surgeries?
Orthopedic surgeries have risks like infection, blood clots, and nerve damage. Anesthesia complications can also happen. The risks depend on the surgery type, like joint replacement or fracture repair.
How can infection risk be minimized after orthopedic surgery?
To lower infection risk, antibiotics are given before, during, and after surgery. Keeping the surgery area clean and proper wound care are key. Following your surgeon’s post-op care instructions helps prevent infections.
What is the risk of blood clots and circulatory complications after orthopedic surgery?
Blood clots and circulatory issues, like DVT and PE, are big risks after surgery. This is more common after hip or knee replacements. To prevent these, anticoagulants, compression stockings, and early movement are used.
Can orthopedic surgery result in nerve damage or neurological complications?
Yes, nerve damage is a risk with orthopedic surgery. The chance depends on the surgery and nerves involved. Symptoms can be numbness, tingling, pain, or weakness. It’s important to talk about these risks with your surgeon.
What are the risks associated with orthopedic hardware and implants?
Orthopedic implants can fail, loosen, or cause allergic reactions. This might need a second surgery to fix. Knowing these risks is important for your care.
Are there specific risks associated with joint replacement surgeries?
Joint replacements have risks like infection, loosening, and dislocation. It’s important to understand these risks and talk to your surgeon about them.
What are the risks and complications associated with spinal surgeries?
Spinal surgeries can lead to infections, nerve damage, and hardware failure. Failed Back Surgery Syndrome is a long-term risk. It’s important to discuss these risks with your surgeon.
How do age-related factors influence the risks of orthopedic surgery?
Age affects the risks of orthopedic surgery. Kids and older adults face different risks. Knowing these can help manage your surgery’s outcome.
Can orthopedic surgery lead to chronic pain or long-term complications?
Yes, surgery can cause chronic pain or long-term issues like joint stiffness. The mental impact of chronic pain is significant. Be prepared for long-term management.
How can the risks associated with orthopedic surgery be minimized?
To lower risks, prepare well before surgery and choose an experienced surgeon. Following post-op instructions is also key. This helps avoid complications and ensures a smooth recovery.
When should I seek medical attention after orthopedic surgery?
Seek medical help if you have severe pain, swelling, redness, or trouble moving. Emergency signs like infection or a pulmonary embolism need quick care.
What is the importance of follow-up care after orthopedic surgery?
Follow-up care is vital for monitoring healing and addressing issues early. It helps adjust your rehabilitation plan. Regular check-ups with your surgeon are important for your surgery’s success.
References
- Grau-Villalbazo, J., et al. (2018). Short-term complication rate following orthopedic surgery in a tertiary hospital. European Journal of Orthopaedic Surgery & Traumatology, 28(5), 1031-1040. https://pmc.ncbi.nlm.nih.gov/articles/PMC6024591/

































