IVF has changed reproductive medicine, giving hope to many. But, it doesn’t work for everyone. Embryo transfer failures happen in about 50% of IVF cycles. This is a big problem in assisted reproductive technology.
Dealing with a failed embryo transfer can be very hard. At Liv Hospital, we offer full care and support. We aim to help individuals and couples face IVF challenges.
We know that embryo quality and uterine receptivity are key. By understanding these, we can find out why implantation fails. Then, we can find ways to solve the problem.
Key Takeaways
- IVF cycle failures occur in approximately 50% of cases
- Understanding the causes of embryo transfer failures is key to finding solutions
- Liv Hospital provides full care and support for those going through IVF
- Genetic screening and endometrial assessment help find barriers to implantation
- Personalized care and support help individuals and couples deal with the emotional impact of IVF failures
The Embryo Transfer Process and Success Rates

The embryo transfer process is key in IVF treatment. Success rates vary due to several factors. It’s important to know what affects success or failure.
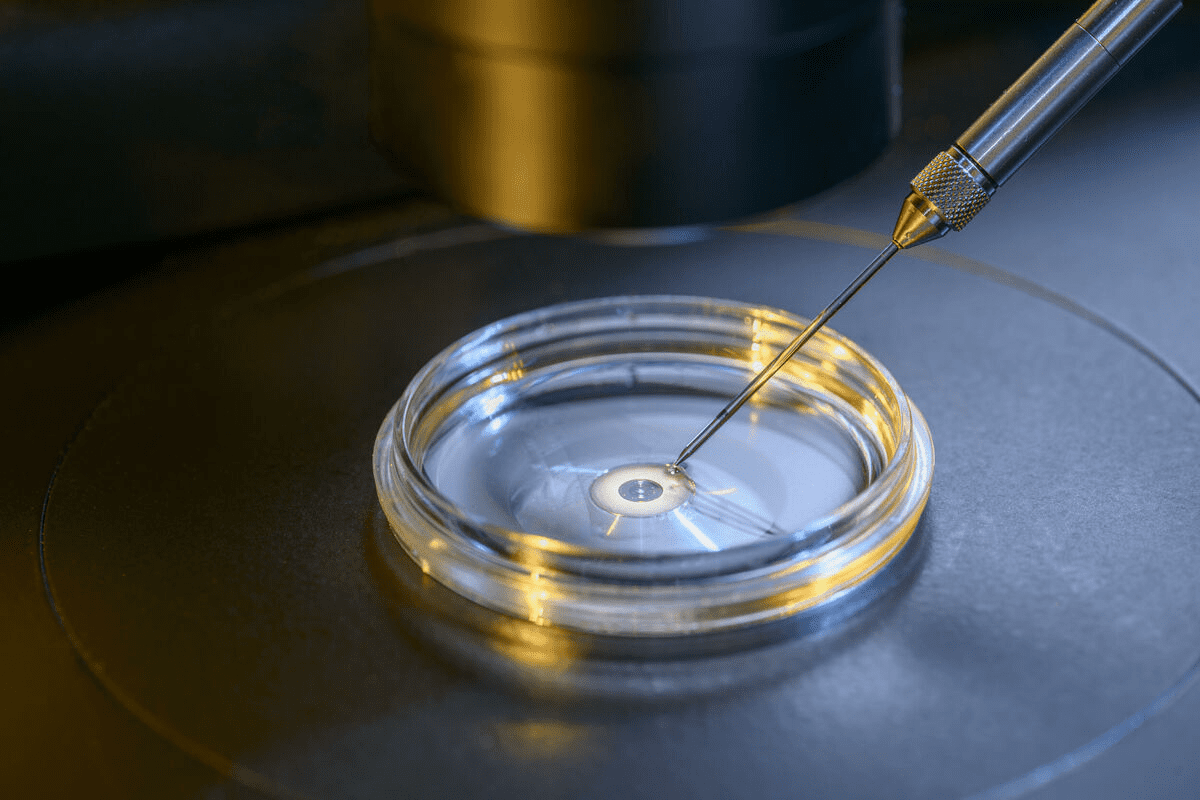
What Happens During an Embryo Transfer
An embryo transfer places a frozen or fresh embryo in the uterus. It’s usually simple and painless. A catheter is used to place the embryo in the right spot in the uterus. This step is critical for getting pregnant.
The procedure is guided by ultrasound for accurate placement. The number of embryos transferred depends on age, embryo quality, and past IVF attempts. It’s a time of high hope for those trying IVF.
Current Success Rates in IVF Treatment
IVF success rates have grown thanks to new technology and methods. On average, women under 35 have a 25% chance of a live birth per transfer. Success rates drop with age, showing age’s big role in IVF success.
- Women under 35: About 25% success rate per transfer
- Women between 35-37: Success rates are 20-24%
- Women between 38-40: Success rates are 15-19%
- Women over 40: Success rates under 15%
These numbers show how success rates change with age and other factors.
Defining a Failed Transfer
A failed IVF transfer means no pregnancy after embryo transfer. Reasons include poor embryo quality, uterine issues, or transfer problems. Knowing why a transfer fails helps plan the next steps.
Causes of a failed transfer include:
- Embryo quality issues
- Uterine abnormalities or receptivity problems
- Age-related decline in egg or sperm quality
Healthcare providers can tailor advice and plans to boost success in future IVF cycles.
Understanding Frozen Embryo Transfer Failure

It’s important to know why frozen embryo transfers fail. These transfers are key in IVF, giving hope to many. But, they come with their own set of challenges.
Statistics on Failed Transfers
Recent studies have shown how common failed frozen embryo transfers are. They looked at nearly 44,000 women. The success rate changes a lot with age.
For women over 45, trying more than three times might not help much. This is because the chances of success keep going down.
Key statistics to consider:
- Nearly 50% of IVF cycles result in failure
- Age is a significant factor in the success of frozen embryo transfers
- Cumulative live birth rates decrease with advancing age, specially after 45
The 50% Failure Rate in IVF Cycles
The 50% failure rate in IVF cycles is a harsh reality. It shows how complex and challenging IVF can be. Many things can cause this failure, like the embryo, the mother, or technical issues.
The emotional impact of a failed IVF cycle is huge. It’s vital for clinics to offer full support to those going through it.
Difference Between Failed Implantation and Miscarriage
It’s key to understand the difference between failed implantation and miscarriage. Failed implantation happens when an embryo can’t attach to the uterine lining. Miscarriage is when a pregnancy ends after it has attached.
Knowing this helps manage what patients expect and understand the IVF journey. Each situation has its own meaning for treatment and future tries.
Age-Related Factors in Transfer Success
Advanced maternal age greatly affects the success of embryo transfers. As women get older, their eggs become less quality and quantity. This makes it harder to get pregnant through IVF.
Impact of Advanced Maternal Age
Egg quality drops with age, mainly after 35. This can lead to IVF failures like failed fertilization or abnormal embryos. Women over 40 face even greater challenges due to the higher likelihood of chromosomal abnormalities and decreased ovarian reserve.
Studies show IVF success rates drop with age. Women under 35 have better success rates than those over 40. The main reason is the decline in egg quality and quantity with age.
2024 Research on Women Over 45
A 2024 study looked at IVF outcomes in women over 45. It found success rates are generally lower but can be improved by:
- Using donor eggs
- Having a healthy uterine environment
- Opting for preimplantation genetic testing (PGT) to select healthy embryos
The study stressed the need for personalized treatment plans for women over 45 undergoing IVF.
Diminished Ovarian Reserve Considerations
Diminished ovarian reserve (DOR) means the ovary loses function, leading to fewer eggs. Age is a big factor in DOR, making IVF treatments harder. Women with DOR may benefit from alternative treatment options, such as egg donation or modified stimulation protocols.
It’s key to understand how age affects ovarian reserve for effective treatment strategies. Healthcare providers use age, hormone levels, and ultrasound findings to assess ovarian reserve and predict IVF outcomes.
By considering these age-related factors, healthcare providers can better counsel patients on their chances of success with IVF. This helps patients make informed decisions about their treatment options.
Embryonic Causes of Failed Transfers
Chromosomal problems in embryos are a big reason for IVF failure. It’s important to check the quality of embryos and use genetic testing. These issues can stop embryos from growing right, leading to failed implantation or miscarriage.
Chromosomal Abnormalities
Chromosomal issues are a major cause of IVF failure. These problems can make it hard for an embryo to implant or grow. The most common issue is aneuploidy, where the embryo has the wrong number of chromosomes.
Key chromosomal abnormalities include:
- Aneuploidy: Having an incorrect number of chromosomes
- Mosaicism: Presence of both normal and abnormal cells
- Structural abnormalities: Deletions, translocations, or duplications of chromosomal material
Embryo Quality Assessment Methods
Checking embryo quality is key to a successful IVF outcome. Embryologists look at several things to judge quality, including:
- Morphological assessment: Looking at how the embryo looks
- Time-lapse imaging: Watching how the embryo grows over time
- Metabolic testing: Checking the embryo’s metabolic activity
Preimplantation Genetic Testing Options
Preimplantation genetic testing (PGT) helps find healthy embryos. There are different types of PGT, such as:
- PGT-A (Preimplantation Genetic Testing for Aneuploidy): Screening for chromosomal abnormalities
- PGT-M (Preimplantation Genetic Testing for Monogenic disorders): Testing for specific genetic disorders
- PGT-SR (Preimplantation Genetic Testing for Structural Rearrangements): Identifying structural chromosomal abnormalities
Using PGT can greatly increase the chances of choosing a healthy embryo for transfer. This can lower the risk of failed transfers and miscarriages.
Maternal Factors in Frozen Embryo Transfer Failure
Frozen embryo transfer failure can happen due to several reasons. These include uterine abnormalities and endometrial inflammation. Knowing about these factors is key to better IVF success rates.
Uterine Structural Abnormalities
Uterine issues can greatly affect frozen embryo transfer success. Problems like fibroids, polyps, and a septate uterus can block embryo implantation. Fixing these problems through surgery can boost IVF results.
Endometrial Inflammation
Endometrial inflammation is another big factor in failed embryo transfers. It can mess up the endometrium’s function, making it hard for embryos to implant. Spotting and treating this inflammation is vital for better IVF success.
| Causes of Endometrial Inflammation | Diagnostic Methods | Treatment Options |
|---|---|---|
| Infections | Ultrasound, Biopsy | Antibiotics, Anti-inflammatory medications |
| Endometriosis | Laparoscopy, MRI | Hormonal therapy, Surgery |
| Irritants (e.g., previous surgeries) | Hysteroscopy, Ultrasound | Removal of irritants, Anti-inflammatory measures |
Age-Related Epigenetic Changes
As women get older, epigenetic changes in the mother can affect embryo transfer success. These changes can alter gene expression, impacting implantation and development. Understanding these changes helps tailor IVF treatments better.
By tackling these maternal factors, healthcare providers can create more effective strategies. This can lead to better outcomes for frozen embryo transfers, improving IVF success rates.
Endometrial Receptivity Issues
Understanding endometrial receptivity is key to addressing issues related to failed embryo transfers. A healthy and receptive endometrium is essential for successful embryo implantation during IVF cycles.
The Window of Implantation
The window of implantation is the specific period when the endometrium is ready for embryo implantation. This window is between 6-10 days after ovulation. During this time, the endometrium changes to prepare for implantation.
Factors Affecting the Window of Implantation:
- Hormonal fluctuations
- Endometrial thickness
- Presence of endometrial polyps or fibroids
Non-Receptive Endometrium Signs
A non-receptive endometrium can greatly reduce implantation chances. Signs include:
- Inadequate endometrial thickness
- Abnormal uterine bleeding
- Presence of chronic endometritis
Identifying these signs early can help tailor treatment strategies to improve endometrial receptivity.
Endometrial Thickness Concerns
Endometrial thickness is a key factor in endometrial receptivity. A thickness of less than 7mm is generally inadequate for implantation. Factors contributing to thin endometrium include:
| Factor | Description | Potential Impact |
|---|---|---|
| Hormonal Imbalance | Insufficient estrogen levels | Thin endometrium |
| Endometrial Damage | Previous surgeries or infections | Scarring and thin lining |
| Poor Blood Flow | Inadequate blood supply to the uterus | Impaired endometrial growth |
Addressing these concerns through appropriate medical interventions can help improve endometrial thickness and receptivity.
Immune System Dysfunction and Implantation
Understanding how the immune system affects implantation is vital for IVF success. The immune system’s role in IVF is complex. It can either help or hinder embryo implantation.
Autoimmune Factors
Autoimmune disorders happen when the immune system attacks the body’s own tissues. In IVF, these disorders can cause the immune system to reject the embryo. Conditions like antiphospholipid syndrome and thyroid autoimmunity increase the risk of IVF failure.
Women with autoimmune disorders might benefit from immunomodulatory treatments. These treatments aim to adjust the immune system’s response. This makes it easier for the embryo to implant.
Natural Killer Cell Activity
Natural Killer (NK) cells are important for fighting infections and foreign substances. But, high NK cell activity can harm embryo implantation.
Research shows that too many NK cells in the uterus can harm the embryo. This increases the chance of implantation failure. Testing for NK cell activity and treating it can help reduce this risk.
Immunological Rejection of Embryos
The immune system must be able to tell self from non-self for IVF to work. Sometimes, the immune system sees the embryo as foreign. This leads to immunological rejection.
This rejection can happen for many reasons, like differences in human leukocyte antigen (HLA) between the mother and embryo. Knowing these immunological factors helps doctors find ways to prevent rejection. This can improve IVF success rates.
Diagnostic Tests After Failed Transfers
Diagnostic tests are key in finding out why embryo transfers fail. They help doctors create better plans for future treatments. After a failed transfer, we suggest several tests to find the main problems.
Endometrial Receptivity Analysis (ERA)
Endometrial Receptivity Analysis (ERA) checks when the uterus is ready for an embryo. It takes a biopsy of the endometrium to find the best time for transfer.
ERA is great for those who keep failing to implant embryos. It can make the timing of the transfer better, raising the chances of success.
Hysteroscopy Benefits
Hysteroscopy lets us see inside the uterus without big surgery. It’s important for spotting problems in the uterus that might stop embryos from implanting.
During hysteroscopy, we can find and fix issues like polyps or adhesions. This can help future implantations succeed.
Advanced Imaging Techniques
Tools like 3D ultrasound and saline infusion sonography give us clear pictures of the uterus. These tests help us see if there are any issues that might be causing failed transfers.
| Imaging Technique | Description | Benefits |
|---|---|---|
| 3D Ultrasound | Provides detailed 3D images of the uterus and endometrium | Helps identify uterine abnormalities and assess endometrial thickness |
| Saline Infusion Sonography | Involves infusing saline into the uterus to enhance ultrasound imaging | Helps identify polyps, fibroids, and other uterine abnormalities |
Repeat Embryo Testing Considerations
Testing embryos again, like with preimplantation genetic testing (PGT), might be suggested after a failed transfer. This can help pick the healthiest embryos for future transfers.
Repeat testing is often suggested for those who have failed to implant many times or have genetic concerns.
Treatment Options to Improve Success Rates
To boost the chances of a successful IVF cycle, many treatment options are available. These range from medical interventions to lifestyle changes. Each person’s journey with IVF is unique. So, it’s important to tailor these options to fit individual needs, increasing the chances of success.
Medical Interventions
Medical interventions are key to better IVF success rates. These can include:
- Personalized Medication Regimens: Tailoring medication to the individual’s response can significantly impact IVF outcomes.
- Hormone Therapy: Regulating hormonal balances is critical for creating an optimal environment for embryo implantation.
- Immunotherapy: In cases where immune system dysfunction is identified, immunotherapy can be a valuable treatment approach.
Surgical Solutions for Uterine Factors
Sometimes, uterine factors can hinder IVF success. Surgical solutions can address these issues:
- Correcting Uterine Anomalies: Surgical correction of uterine abnormalities can improve implantation rates.
- Removing Fibroids or Polyps: Eliminating fibroids or polyps that may interfere with implantation can enhance IVF success.
- Treating Endometriosis: Surgical intervention for endometriosis can improve the chances of successful IVF.
| Surgical Procedure | Impact on IVF Success |
|---|---|
| Correcting Uterine Anomalies | Improves implantation rates by creating a more favorable uterine environment. |
| Removing Fibroids or Polyps | Enhances IVF success by eliminating obstacles to implantation. |
| Treating Endometriosis | Reduces inflammation and improves the chances of successful IVF. |
Lifestyle Modifications
Lifestyle changes can also significantly impact IVF success rates. We recommend:
- Dietary Changes: Adopting a balanced diet rich in nutrients can support reproductive health.
- Exercise and Stress Management: Regular exercise and effective stress management techniques can improve overall well-being and IVF outcomes.
- Avoiding Harmful Substances: Refraining from smoking, excessive alcohol consumption, and other harmful substances is critical for IVF success.
By combining medical interventions, surgical solutions, and lifestyle modifications, we can significantly improve IVF success rates. It’s essential to work closely with healthcare providers to determine the most appropriate and personalized treatment plan.
Conclusion: Making Informed Decisions After Failed Transfers
Understanding why IVF fails is key for those trying to have a baby. We’ve looked at many reasons, like age, embryo health, and mom’s health.
Tests like Endometrial Receptivity Analysis (ERA) and hysteroscopy help find the problems. There are many ways to fix these issues, from medicine to changing your lifestyle.
Knowing what to do next can help improve your chances of success with IVF. If you’ve had failed transfers, talk to fertility experts. They can help figure out the best plan for you.
With the right information and support, you can feel more confident. This can help you reach your dream of having a family through IVF.
FAQ
What is considered a failed embryo transfer?
A failed embryo transfer happens when an embryo doesn’t stick to the uterus. It also occurs when no pregnancy results after transferring an embryo.
Why do IVF transfers fail?
IVF transfers fail for many reasons. These include genetic problems, issues with the uterus, problems with the lining of the uterus, immune system issues, and age.
Is failed implantation considered a miscarriage?
No, failed implantation is not a miscarriage. Miscarriage happens when a pregnancy ends after the embryo implants. Failed implantation is when the embryo doesn’t stick to the uterus.
What are the signs of non-receptive endometrium?
Signs of a non-receptive endometrium include an abnormal thickness of the uterine lining. It also includes poor blood flow and hormonal imbalances that affect the lining.
How is embryo quality assessed?
Embryo quality is checked in several ways. These include looking at its shape, genetic testing, and using time-lapse imaging.
What is the role of immune system dysfunction in IVF failure?
Immune system problems can cause IVF to fail. They can affect how the embryo implants and grows. Autoimmune issues, natural killer cells, and rejecting the embryo are all factors.
What diagnostic tests are available after failed IVF transfers?
After failed IVF transfers, several tests are available. These include checking the uterine lining, hysteroscopy, advanced imaging, and testing the embryo again.
Can lifestyle modifications improve IVF success rates?
Yes, making healthy lifestyle choices can help improve IVF success. This includes keeping a healthy weight, reducing stress, and avoiding smoking and too much alcohol.
What are the treatment options for uterine structural abnormalities?
To treat uterine structural problems, surgery might be needed. This includes removing a septum or fibroids through hysteroscopy.
How does age affect IVF outcomes?
Age greatly affects IVF success. As women get older, egg quality drops, and the risk of genetic problems increases. This leads to lower success rates with IVF.
What is the difference between failed implantation and failed IVF?
Failed implantation is when an embryo can’t stick to the uterus. Failed IVF is a broader term that includes not just implantation issues but also failed fertilization and early pregnancy loss.
Why does IVF fail with good embryos?
Even with good embryos, IVF can fail. This is due to issues like uterine receptivity, immune system problems, or other factors that affect implantation and pregnancy.
References
National Center for Biotechnology Information. Embryo Transfer Failure: Causes and Solutions in IVF. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7939155/