Comparative analysis of the benefits and risks of fresh versus frozen transfer protocols. Choosing between fresh and frozen embryo transfer is a big decision in your IVF journey. Knowing the differences in success rates and safety can help you make a better choice with your fertility specialist.
Recent studies show that results depend on many factors and your personal situation. The United States Department of Health and Human Services found that most people choose frozen embryos, from 79.8% to 86.1%. At Liv Hospital, we use the latest research and personal care to help you pick the best embryo transfer method for success.
Key Takeaways
- IVF success rates can vary significantly based on the choice between fresh and frozen embryo transfer.
- Frozen embryo transfers have shown higher live birth rates for women over 38 years old.
- The decision between fresh and frozen transfer depends on multiple clinical factors and individual patient circumstances.
- Liv Hospital’s patient-centered approach ensures personalized care in choosing the most suitable embryo transfer method.
- Understanding the advantages and factors influencing the choice can lead to a more informed decision.
Understanding Fresh and Frozen Embryo Transfers
When thinking about IVF, it’s key to know the difference between fresh and frozen embryo transfers. These choices are part of the IVF process. Each option has its own way of doing things and affects success rates differently.
What is a Fresh Embryo Transfer?
A fresh embryo transfer happens right after egg retrieval and fertilization. The embryo is put into the uterus 3-5 days later. Fresh transfers are often picked when there are many embryos and the uterus is ready.
What is a Frozen Embryo Transfer (FET)?
A frozen embryo transfer uses embryos thawed from a past cycle. This lets for genetic testing and better timing for the transfer. Research shows FET works better for women over 38.
Key Differences in the Procedures
The main differences between fresh and frozen embryo transfers are in timing and preparation. Here are the main points:
- Timing: Fresh transfers happen right after egg retrieval and fertilization. Frozen transfers are planned for a later cycle.
- Uterine Preparation: Frozen transfers allow for better uterine preparation, which can help with implantation.
- Genetic Testing: Frozen transfers often include genetic testing of embryos before transfer, which can boost success rates.
Knowing these differences is vital for making smart choices about IVF treatment. The choice between fresh and frozen depends on many factors. These include the patient’s age, medical history, and specific situation.
By thinking about these factors and understanding the procedures, future parents can make informed decisions. The most important thing is to talk to healthcare providers. They can help decide the best approach based on individual needs.
The Evolution of IVF Transfer Methods

Advances in cryopreservation have changed IVF transfer methods a lot. They have made things better for patients. Before, fresh embryo transfers were the main choice. But now, thanks to new tech, frozen transfers are becoming more common.
Historical Preference for Fresh Transfers
At first, fresh embryo transfers were the norm in IVF. This meant putting embryos in the uterus right after they were taken out. The idea was to keep them in a good environment for implantation.
But, there were downsides. There was a risk of ovarian hyperstimulation syndrome (OHSS). Also, the hormonal stimulation could make the uterine environment less ideal.
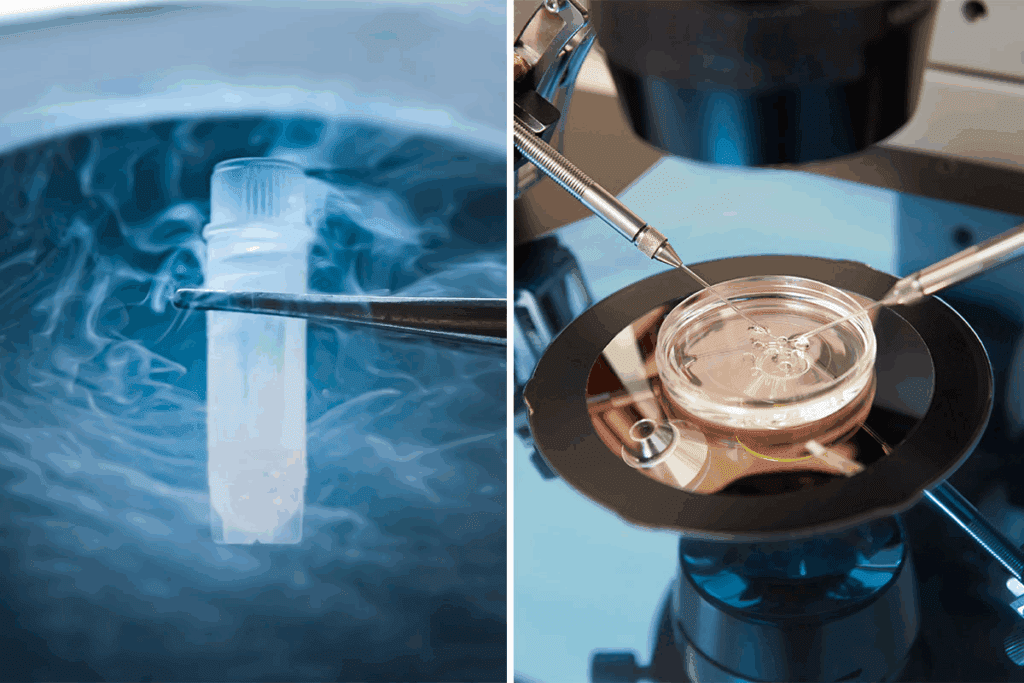
Technological Advances in Cryopreservation
Vitrification, a fast freezing method, has been a big leap in IVF. It has greatly increased the chances of frozen embryos surviving. This makes frozen embryo transfers (FET) a better choice for many.
Key advancements in cryopreservation include:
- Improved freezing techniques
- Better embryo survival rates
- Enhanced flexibility in transfer timing
These changes have made the “freeze-all” approach more popular. This means freezing all good embryos for later use.
Shifting Clinical Practices
More and more, clinics are leaning towards frozen transfers. They see them as better for some patients.
The table below shows the main differences between fresh and frozen transfers:
| Aspect | Fresh Embryo Transfer | Frozen Embryo Transfer (FET) |
|---|---|---|
| Timing | Shortly after egg retrieval | After thawing frozen embryos |
| OHSS Risk | Higher risk due to recent hormonal stimulation | Lower risk as transfer occurs in a natural or programmed cycle |
| Uterine Environment | Potentially affected by hormonal stimulation | More natural environment, potentially improving implantation |
As we keep improving IVF, frozen transfers will likely stay the preferred choice. This is because they offer better success rates and are safer for patients.
Success Rates: Fresh Versus Frozen Transfer Outcomes
IVF success rates differ between fresh and frozen embryo transfers. It’s key for patients and doctors to know this when choosing fertility treatments.
Overall Live Birth Rate Comparisons
Frozen embryo transfers often lead to higher success rates than fresh ones. Recent data shows frozen transfers have better live birth rates, mainly in certain age groups. This change is making doctors rethink how they do IVF.
“The rise in live birth rates with frozen transfers is a big step forward in IVF,” says a top fertility expert. “It’s changing how we handle fertility care.”
Age-Specific Success Statistics
Age is a big factor in IVF success. For women under 35, the difference between fresh and frozen is smaller. But, for women over 38, frozen transfers lead to better live birth rates.
For women aged 38-40, frozen transfers have a 35.7% live birth rate. This is higher than the 28.4% rate for fresh transfers.
The 1.4 to 5.4 Times Greater Odds with Frozen Transfers
Women in advanced age groups have 1.4 to 5.4 times better live birth odds with frozen transfers. This is due to better endometrial receptivity and avoiding OHSS with fresh transfers.
Looking at the data, frozen embryo transfers are a strong option for IVF patients. They offer higher success rates, which is great for older women wanting to get pregnant.
Age as a Critical Factor in Your Decision
Age is key when it comes to IVF success, affecting the choice between fresh and frozen embryo transfers. Looking at different age groups and their success rates, it’s clear age is more than just a number. It’s a major biological factor.
Women Under 35: What the Data Shows
Women under 35 see high success rates with both fresh and frozen embryo transfers. But, frozen transfers might have a slight edge in live birth rates. This age group often has better egg quality, leading to a more favorable prognosis.
Key statistics for women under 35:
- Live birth rates for frozen transfers: 45.6%
- Live birth rates for fresh transfers: 41.1%
Women 35-37: Comparative Outcomes
Women aged 35-37 see a decline in success rates for both fresh and frozen transfers. Yet, frozen transfers remain the better choice. The gap in live birth rates between frozen and fresh transfers widens.
“For women aged 35-37, frozen embryo transfers resulted in a 35.1% live birth rate compared to 30.4% for fresh transfers.”
Women 38-40: The 35.7% vs 28.4% Success Rate Difference
Women aged 38-40 see a significant advantage in frozen transfers. The data shows a notable difference in success rates, with frozen transfers achieving a 35.7% live birth rate versus 28.4% for fresh transfers.
This age group benefits greatly from the improved outcomes of frozen embryo transfers. It’s a preferred option for many.
Women Over 40: Special Considerations
For women over 40, success rates for both fresh and frozen transfers drop significantly. Yet, frozen transfers remain the better choice. In this age group, the need for donor eggs or advanced reproductive technologies becomes more common.
Women over 40 should closely consult with their healthcare providers. This will help determine the best approach for their individual situation.
Embryo Quality and Transfer Success Rates
Embryo quality is very important in IVF success. It’s a key area for both patients and doctors to focus on. Grading embryos helps find the best ones for transfer.
Understanding Embryo Grading Systems
Embryo grading systems check how good an embryo is. They look at cell number, cell division, and if there’s any damage. This helps figure out if an embryo can implant well.
High Quality Embryos: 79% Live Birth Rate
High-quality embryos have the best features. Research shows a 79% live birth rate when these are transferred. This high rate comes from picking embryos with the best implantation chances.
Good Quality Embryos: 64% Success Rate
Good quality embryos also have a good chance of success. They have a 64% live birth rate. This shows even not-so-perfect embryos can lead to successful pregnancies.
Poor Quality Embryos: 28% Success Rate
Poor quality embryos have a lower success rate. But, they can lead to a 28% live birth rate. Some poor quality embryos can also result in successful pregnancies, but at a lower rate.
In summary, embryo quality is very important for IVF success. Knowing about embryo grading and success rates helps make better treatment choices.
Health Outcomes for Mother and Baby
Choosing between fresh and frozen embryo transfers affects both mother and baby’s health. This choice is more than just about success rates. It involves many health considerations.
Ovarian Hyperstimulation Syndrome (OHSS) Risk
Fresh embryo transfers carry a higher risk of Ovarian Hyperstimulation Syndrome (OHSS). OHSS is a serious condition that can happen during fertility treatments. It’s more common with fresh transfers because they stimulate the ovaries to produce more eggs.
Key statistics on OHSS risk:
| Transfer Type | OHSS Risk |
|---|---|
| Fresh Embryo Transfer | Higher Risk |
| Frozen Embryo Transfer | Lower Risk |
Preterm Birth Rates
Research shows fresh embryo transfers lead to more preterm births than frozen ones. The odds ratio for preterm birth with fresh transfers is 1.26. This shows a clear difference in outcomes.
“The shift towards frozen embryo transfers has been associated with improved perinatal outcomes, including reduced preterm birth rates.” –
Journal of Fertility and Sterility
Low Birth Weight Outcomes
Fresh embryo transfers also increase the chance of low birth weight babies. The odds ratio for low birth weight with fresh transfers is 1.37. This highlights the benefits of frozen transfers for birth weight.
Other Maternal Health Considerations
Other health factors are also important when deciding between fresh and frozen transfers. These include the mother’s overall health, pregnancy complications, and long-term effects of fertility treatments.
Every person’s health is different. What’s a big risk for one might not be as big for another. It’s key to talk to healthcare professionals to find the best option for your health and fertility goals.
The Implantation Process and Timing
The implantation process after a frozen embryo transfer is key in IVF treatment. It’s when the embryo attaches to the uterine lining. This step is essential for a successful pregnancy.
When Does Implantation Occur After Frozen Embryo Transfer?
Implantation usually happens 6-10 days after fertilization. But, this time can change with frozen embryo transfers. The exact timing depends on the embryo’s quality and the uterine lining’s readiness.
“The window for implantation is critical, and understanding when it occurs can significantly impact the success of the treatment,” says Medical Expert, a fertility specialist. “With frozen embryo transfers, the timing can be more flexible, but it’s essential to optimize the uterine environment.”
What Is Considered Late Implantation?
Late implantation is when the embryo attaches later than the usual 6-10 days. It’s not rare but can be a worry. It might affect how well the embryo and uterine lining sync up.
Is Late Implantation a Concern?
Late implantation might affect pregnancy success. But, it’s not always a worry. Many things can influence implantation success, and late implantation doesn’t always mean failure.
We’ve seen that late implantation can be successful when the embryo is good and the uterine lining is ready. “Late implantation is not a definitive indicator of a problem,” notes Medical Expert, a reproductive endocrinologist. “Each pregnancy is unique, and the timing of implantation is just one factor among many.”
Late Implantation Success Stories
There are many stories of successful pregnancies with late implantation. These stories show the importance of patience and the complex factors in IVF success.
In conclusion, knowing when implantation happens after a frozen embryo transfer is key. It helps manage expectations and improve treatment results. While late implantation can be a worry, it’s not always bad. With the right care and considering each person’s situation, many women have had successful pregnancies despite late implantation.
Hormonal Environment and Endometrial Receptivity
The success of embryo transfers depends a lot on the hormonal environment and endometrial receptivity. These are key factors for both fresh and frozen embryo transfers.
Natural vs. Stimulated Cycles
In IVF, natural and stimulated cycles are different. Natural cycles follow the body’s normal cycle without drugs. Stimulated cycles use drugs to get more eggs.
Frozen embryo transfers (FET) often happen in natural cycles. This helps control the hormonal environment better. It might improve implantation success.
Endometrial Preparation for Frozen Transfers
Getting the endometrium ready is key for frozen embryo transfers. We aim to create the best environment for implantation. This means syncing the transfer with natural hormonal changes.
- Monitoring the thickness and quality of the endometrium
- Adjusting hormone levels to mimic a natural cycle
- Timing the transfer to coincide with peak receptivity
How Hormonal Differences Affect Implantation
Hormonal differences between natural and stimulated cycles matter a lot for implantation. For example, stimulated cycles can have more estrogen. This might change how receptive the endometrium is.
Our studies show that frozen embryo transfers in natural cycles might be better. They create a more natural hormonal environment. This could help with implantation success.
What Causes Implantation Delay
Implantation delay can happen for many reasons. Hormonal imbalances, endometrial issues, and poor embryo quality are some. Knowing these reasons is important for better treatment results.
- Hormonal imbalances affecting endometrial receptivity
- Poor embryo quality
- Asynchrony between embryo development and endometrial preparation
By tackling these issues, we can boost the chances of successful implantation and pregnancy.
Genetic Testing and Advanced Maternal Age
Genetic testing is key in IVF success, more so for older women. As we get older, our eggs’ quality and genetic health decline. This raises the risk of genetic issues in embryos. Preimplantation genetic testing (PGT) helps pick healthy embryos for transfer.
Preimplantation Genetic Testing Options
PGT is very helpful for older women. It comes in several types:
- PGT-A (Preimplantation Genetic Testing for Aneuploidy): This checks for chromosomal problems, finding embryos with the right number of chromosomes.
- PGT-M (Preimplantation Genetic Testing for Monogenic/Single Gene Defects): It’s for those at risk of a specific genetic disorder.
- PGT-SR (Preimplantation Genetic Testing for Structural Rearrangements): It spots embryos with balanced chromosomal structures.
Benefits of Testing with Frozen Cycles
PGT works on frozen embryos. This is because it needs time for testing. Frozen embryo transfers (FET) are used with PGT. The advantages are:
- It picks the best embryos, boosting pregnancy chances.
- It lowers miscarriage risk from chromosomal issues.
- It matches embryo transfer with the best uterine timing.
Comprehensive Chromosomal Screening for Women 36-42
Women aged 36 to 42 benefit from CCS. CCS checks embryos’ chromosomes for any problems. It has been shown to greatly increase live birth rates in this age group.
Impact on Decision-Making
PGT results greatly influence IVF decisions for couples. They can choose the best embryos to transfer. This might mean fewer transfers, easing emotional and financial burdens.
PGT results also guide decisions on egg donation or adoption. They help families plan their future more clearly.
Financial and Practical Considerations
Understanding the costs and practicalities of fresh and frozen embryo transfers is key for IVF patients. It’s not just about the medical benefits. The economic and logistical sides also play a big role in the decision-making process.
Cost Comparison Between Fresh and Frozen Cycles
The start of IVF includes egg retrieval and fertilization, common to both fresh and frozen transfers. But, frozen transfers add costs for thawing and storage. The total cost for a frozen embryo transfer can be slightly higher due to these extra steps. These expenses are important to consider when planning IVF treatment.
| Procedure | Cost Components | Average Cost Range |
|---|---|---|
| Fresh Embryo Transfer | IVF cycle, egg retrieval, fertilization, transfer | $12,000 – $15,000 |
| Frozen Embryo Transfer | IVF cycle, egg retrieval, fertilization, freezing, thawing, storage, transfer | $15,000 – $18,000 |
Insurance Coverage Variations
Insurance for IVF and embryo transfers varies a lot. Some plans cover the first cycle but not storage or frozen transfers. It’s essential for patients to review their insurance coverage carefully to understand what is included and what additional costs they may incur.
Timing and Scheduling Flexibility
Frozen embryo transfers offer flexibility in timing and scheduling. This can be very helpful for patients. It lets them plan the transfer at the best time for their health and readiness, potentially improving success rates. Frozen transfers can be scheduled at a time that optimizes the patient’s health and receptivity.
Multiple Transfer Opportunities
With frozen embryo transfers, patients can have multiple transfers from one IVF cycle. This is great for those needing more than one try. The ability to use stored embryos for subsequent transfers without the need for additional egg retrievals can be both cost-effective and less physically demanding.
By looking at these financial and practical aspects, patients can make better choices for their IVF treatment. They can choose what fits their personal and medical needs best.
Clinical Scenarios: When to Choose Fresh Versus Frozen Transfer
Choosing between fresh and frozen embryo transfer depends on many factors. These include the patient’s medical history, current health, and specific fertility challenges.
Ideal Candidates for Fresh Transfer
Young women with a high ovarian reserve often do better with fresh transfers. Women under 35 with no known uterine or tubal abnormalities tend to have higher success rates.
Those who respond well to ovarian stimulation and produce many high-quality embryos are also good candidates. Fresh transfer is more natural and suits those who need to start treatment quickly.
Ideal Candidates for Frozen Transfer
Frozen embryo transfer (FET) is best for those at risk of ovarian hyperstimulation syndrome (OHSS). Women with polycystic ovary syndrome (PCOS) are often recommended for FET due to their higher risk of OHSS.
Patients who have undergone preimplantation genetic testing (PGT) and need a controlled hormonal environment are also good candidates for FET. It helps match embryo development with endometrial receptivity.
Special Medical Circumstances
Some medical conditions make one transfer method better than the other. For example, patients with endometriosis or adenomyosis may benefit from FET. This is because FET allows for better hormonal control and reduces inflammation.
Those with a history of recurrent implantation failure may also prefer FET. It offers a more tailored approach to embryo transfer. Women at high risk of OHSS or those experiencing severe side effects from fertility meds are also better off with FET.
In conclusion, the choice between fresh and frozen embryo transfer should be based on individual needs. Understanding the pros and cons of each method helps healthcare providers tailor treatments for better outcomes.
Conclusion
As we wrap up our look at fresh versus frozen embryo transfer, it’s clear that making IVF choices is complex. The decision between fresh and frozen transfers depends on many things. These include age, how good the embryo is, and your health.
The right choice should be made with full knowledge and understanding. This means looking at the latest studies and guidelines. We’ve learned that frozen transfers might work better for some, while fresh might be better for others.
Knowing the differences helps patients make better choices for their IVF journey. It’s key to talk to a healthcare provider. They can help figure out the best option for your unique situation.
FAQ
What is the difference between a fresh embryo transfer and a frozen embryo transfer?
A fresh embryo transfer uses an embryo that hasn’t been frozen. It happens during the same cycle as egg retrieval. A frozen embryo transfer, on the other hand, involves thawing and transferring a previously frozen embryo.
When does implantation occur after frozen embryo transfer?
Implantation usually happens 6-10 days after a frozen embryo transfer. But, it can vary based on individual factors.
What is considered late implantation?
Late implantation is when it happens more than 10 days after embryo transfer. But, what counts as late can vary.
Is late implantation a bad sign?
Late implantation might raise some concerns. But, many women have had successful pregnancies even with late implantation.
What causes late implantation?
Several things can cause late implantation. These include hormonal imbalances, issues with the endometrium, and embryo quality.
How late can implantation happen?
Implantation can happen later than expected in some cases. This shows that timing can vary a lot.
Are frozen embryo transfers associated with better health outcomes?
Yes, frozen embryo transfers are linked to better health outcomes. They have lower risks of OHSS and better birth outcomes.
What are the benefits of preimplantation genetic testing with frozen cycles?
Preimplantation genetic testing with frozen cycles can spot genetic issues in embryos. This boosts the chances of a successful pregnancy.
How does the quality of the embryo impact IVF success rates?
The quality of the embryo is key to IVF success. High-quality embryos have a much higher chance of leading to a successful pregnancy.
What is the impact of age on IVF success rates?
Age greatly affects IVF success rates. Women over 38 have lower success rates with fresh transfers. But, frozen transfers can be more successful.
Are there any financial benefits to choosing frozen embryo transfer?
Frozen embryo transfer can save money and offer flexibility. It allows for multiple transfers without needing more egg retrieval cycles.
How does the hormonal environment affect implantation?
The hormonal environment is vital for implantation. Hormonal imbalances can affect how receptive the endometrium is and implantation success.
What are the advantages of frozen embryo transfer for women over 40?
Frozen embryo transfer is great for women over 40. It allows for genetic testing and better uterine receptivity. This improves the chances of a successful pregnancy.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8489809/)