In vitro fertilization (IVF) has changed how we approach fertility. It involves fertilizing eggs outside the body. But, those with poor ovarian response often struggle with IVF treatments. That’s where the estrogen priming protocol ivf comes in, making IVF more effective.
For those with poor ovarian response, the estrogen priming protocol is a game-changer. It boosts egg quality and quantity, raising the chances of a successful pregnancy. This guide will help you understand how to use this protocol in IVF, covering all you need to know about this new fertility treatment.
Key Takeaways
- Understanding IVF and its challenges.
- The role of estrogen priming protocol in improving IVF success.
- Benefits for patients with poor ovarian response.
- Overview of the IVF process with estrogen priming.
- Expectations and outcomes with this advanced fertility treatment.
Understanding IVF Basics
Learning about IVF is key for those thinking about fertility treatments. IVF, or In Vitro Fertilization, is a method where eggs are taken out and fertilized outside the body. Then, they are put back into the uterus.
What Does IVF Stand For?
IVF means In Vitro Fertilization. It’s when an egg is fertilized with sperm outside the body, usually in a lab. The embryo is then moved to the woman’s uterus, hoping it will grow into a baby.
The Standard IVF Process
The IVF process has several main steps:
- Ovarian stimulation: Medications help the ovaries make more eggs.
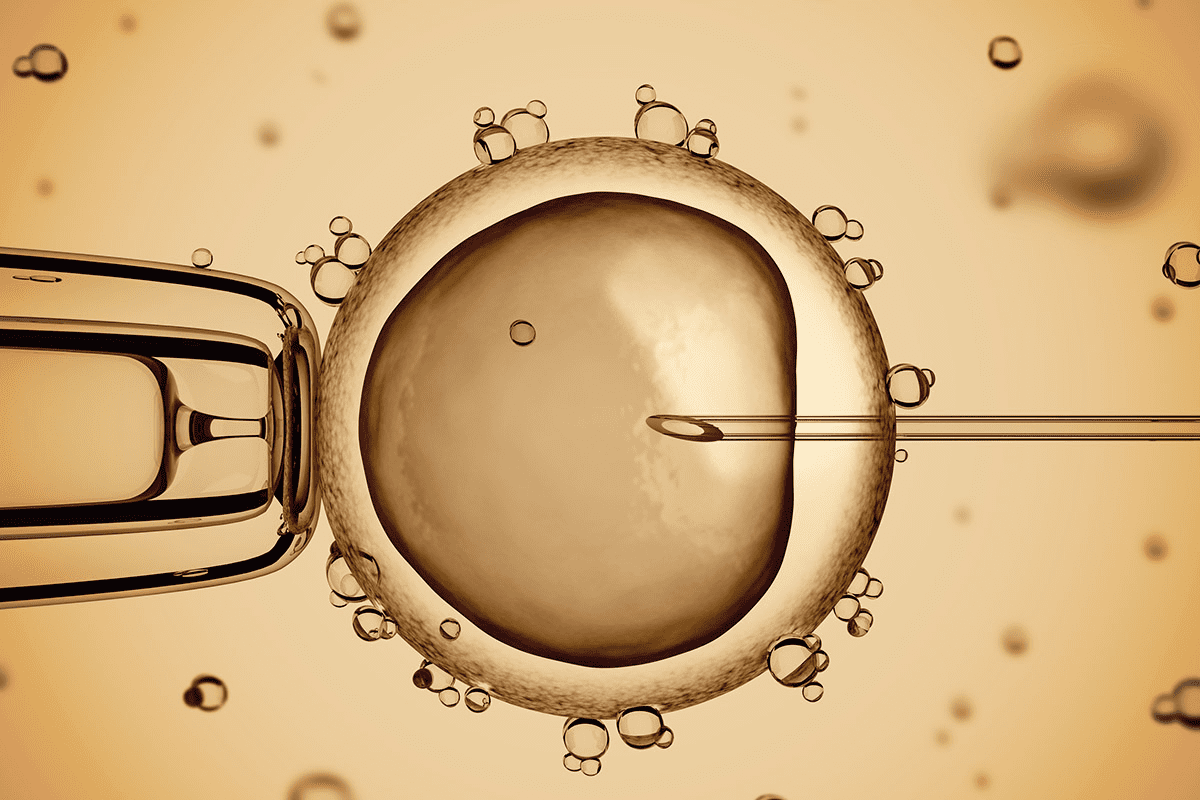
- Egg retrieval: Eggs are taken out through a small surgery.
- Fertilization: Eggs are mixed with sperm in the lab.
- Embryo culture: The fertilized eggs grow in the lab for 3-5 days.
- Embryo transfer: One or more embryos are put into the uterus.
Common Challenges in IVF
Even though IVF works well, there are challenges. These include:
| Challenge | Description |
|---|---|
| Poor Ovarian Response | Some women don’t react well to the stimulation, getting fewer eggs. |
| Low Egg Quality | The quality of eggs can impact fertilization and growth. |
| Cycle Cancellation | Sometimes, the cycle is stopped due to poor response or other issues. |
Knowing these challenges helps prepare for IVF. It lets people make better choices about their fertility treatment.
The Estrogen Priming Protocol in IVF Explained
The estrogen priming protocol is a big step forward in IVF treatments. It helps many patients have successful outcomes. This method uses estrogen before starting an IVF cycle to help the ovaries grow follicles better.
Definition and Purpose
The estrogen priming protocol is a treatment given before IVF. It uses estrogen to get the ovaries ready for stimulation. The main goal is to make follicles more sensitive and help them grow in sync, which is great for those with poor ovarian response.
By giving estrogen first, we can make the IVF cycle better. It helps the ovaries grow follicles better. This leads to more follicles growing in sync and being more responsive to treatment.
Historical Development
The idea of estrogen priming in IVF has grown as we learn more about how ovaries work. It started to help with poor ovarian response. Over time, it has been improved based on research and results.
Studies and trials have been key in making the estrogen priming protocol better. They helped figure out the best way to use it. Now, it’s a big part of IVF, giving hope to those with few options before.
When It’s Recommended
This protocol is often suggested for those with poor ovarian response or a history of not responding well to stimulation. It’s also good for older women or those who didn’t get many eggs in a previous IVF cycle.
By choosing the right patients for estrogen priming, doctors can make IVF plans that fit each person better. This can lead to better results and happier patients.
The Science Behind Estrogen Priming
Understanding estrogen priming is key to better IVF results. This method is designed to make IVF treatments more effective.
How Estrogen Affects Follicular Development
Estrogen is important for growing and maturing follicles in the ovaries. By using estrogen in the priming protocol, we can make follicles grow in sync. This leads to better quality eggs and embryos.
34-36 Hour Window
The timing of the trigger shot is very important. It’s given 34-36 hours before egg retrieval. This timing helps the eggs mature fully, ready for retrieval.
The trigger shot starts the final maturation of eggs. Its timing is critical for a successful IVF cycle.
Types of Trigger Medications
There are different types of trigger shots. These include hCG and GnRHa. The choice depends on the patient’s situation and the IVF protocol.
Post-Trigger Monitoring
After the trigger shot, it’s important to monitor closely. This checks if the response is as expected. Post-trigger monitoring helps make any needed adjustments for a successful egg retrieval.
Statistical Benefits of Estrogen Priming Protocol
Estrogen priming in IVF cycles brings several key benefits. It lowers cycle cancellation rates, boosts oocyte retrieval, and improves embryo quality. These improvements are backed by research.
Reduced Cycle Cancellation Rates
One big plus of estrogen priming is lower cycle cancellation rates. Studies show a drop from 37.7 percent to 15.1 percent. This means more patients can move forward to egg retrieval, boosting their chances of success.
Increased Oocyte Retrieval
Estrogen priming also leads to more oocytes retrieved. It better prepares the ovaries for stimulation, resulting in more eggs. This is key because more eggs mean a better chance of getting viable embryos.
Improved Embryo Quality
Lastly, estrogen priming helps improve embryo quality. It optimizes follicular development, leading to better eggs and embryos. This is vital for successful implantation and pregnancy.
To better understand these benefits, let’s look at a comparative table:
| Outcome Measure | Without Estrogen Priming | With Estrogen Priming |
|---|---|---|
| Cycle Cancellation Rate | 37.7% | 15.1% |
| Average Oocytes Retrieved | 6-8 | 10-12 |
| Embryo Quality Improvement | Baseline | Significant Improvement |
The table clearly shows estrogen priming’s benefits. It reduces cycle cancellations, increases oocyte retrieval, and enhances embryo quality. These improvements make IVF treatments more effective.
Who Should Consider Estrogen Priming?
Estrogen priming is a great choice for people going through IVF, mainly those with certain challenges. It shows clear benefits for specific patient groups.
Poor Ovarian Responders
Poor ovarian responders can greatly benefit from estrogen priming. These are women whose ovaries don’t react well to stimulation. This results in fewer eggs during an IVF cycle. Estrogen priming might help improve this, leading to more eggs for fertilization.
Advanced Maternal Age
Women of advanced maternal age often struggle with IVF. This is due to declining egg quality and quantity. Estrogen priming can enhance the follicular environment. This might improve egg quality and increase fertilization and pregnancy chances.
Previous IVF Failures
Those who have had previous IVF failures might find estrogen priming helpful. It allows for a modified IVF protocol. This might address issues from past failures, boosting the chances of success in future cycles.
Knowing how IVF works and the benefits of estrogen priming can greatly improve fertility treatment success. Tailoring the treatment to each person’s needs can significantly increase the chances of a successful IVF outcome.
Step-by-Step Estrogen Priming Protocol Implementation
To boost IVF success, it’s key to know how to follow the estrogen priming protocol step by step. This method adds estrogen before starting IVF to get follicles ready and make them more responsive to FSH.
Pre-Cycle Preparation
Getting ready before the cycle starts is very important. We look at the patient’s health history, how many eggs they have, and their past IVF results. This helps us make the protocol just right for them.
- Baseline ultrasound to assess ovarian anatomy
- Hormone level testing to evaluate ovarian reserve
- Review of previous IVF cycles to identify areas for improvement
Estrogen Administration Phase
The estrogen phase starts on day 1-3 of the cycle. We give estrogen to get the follicles ready, making them more responsive to FSH.
| Day | Estrogen Dosage | Monitoring |
|---|---|---|
| 1-3 | Estrogen patches or oral estrogen | Baseline hormone levels |
| 4-7 | Continue estrogen dosage | Ultrasound and hormone level testing |
Transition to Stimulation
After the estrogen phase, we move to the stimulation phase. Here, we use FSH to help the follicles grow. When to switch is based on how well the patient responds to the estrogen.
Key factors influencing the transition:
- Hormone level testing
- Ultrasound monitoring
- Patient’s overall response to estrogen priming
By following the estrogen priming protocol carefully, we can make IVF more successful. This helps increase the chances of a successful pregnancy.
Medications Used in Estrogen Priming
It’s important for patients going through IVF to know about estrogen priming. This process uses estrogen to get the uterus ready for embryo transfer.
Types of Estrogen Preparations
There are different types of estrogen used in this process. These include pills, patches, and injections.
- Oral Estrogen Tablets: These are easy to take. Examples are estradiol valerate tablets.
- Estrogen Patches: These patches release estrogen slowly into your blood. Examples are Climara or Vivelle-Dot.
- Injectable Estrogen: This is less common but sometimes used.
Dosage Guidelines
The amount of estrogen given can change based on the treatment plan and how the body reacts. Doctors adjust the dose based on blood tests and ultrasound checks.
| Estrogen Preparation | Typical Starting Dose | Adjustment Criteria |
|---|---|---|
| Oral Estradiol Valerate | 2-4 mg/day | Hormone levels, Ultrasound |
| Estrogen Patches | 0.1-0.2 mg/day | Hormone levels, Ultrasound |
Potential Side Effects
Most people can handle estrogen without problems. But, some might feel sick, have sore breasts, or feel moody.
Talking to your doctor about your health and worries is key. This helps lower the chance of side effects.
The Trigger Shot: Timing and Administration
The trigger shot is given 34-36 hours before egg retrieval. It’s the key to getting eggs ready for the final stage of maturation. This step is vital in the IVF process, making sure eggs are at their best for retrieval.
Purpose and 34-36 Hour Window
The main goal of the trigger shot is to start the final maturation of eggs. This allows for their retrieval at the perfect time. The 34-36 hour gap between the shot and egg retrieval is key. It lets the eggs fully mature and get ready for fertilization.
Timing is critical: If the trigger shot is given too early or late, it can harm the egg retrieval process. So, getting the timing right is very important for a successful IVF.
Types of Trigger Medications
There are many types of trigger medications used in IVF. Each has its own benefits and characteristics. The choice depends on the patient’s needs and the IVF plan.
- hCG (human chorionic gonadotropin): A common trigger medication that mimics the natural LH surge.
- GnRHa (gonadotropin-releasing hormone agonist): Used for patients at risk of ovarian hyperstimulation syndrome (OHSS), as it reduces the risk of this complication.
- Dual trigger: A mix of hCG and GnRHa, used in some cases to improve oocyte maturation and lower OHSS risk.
| Trigger Medication | Characteristics | Benefits |
|---|---|---|
| hCG | Mimics natural LH surge | Well-established protocol |
| GnRHa | Reduces OHSS risk | Ideal for high-risk OHSS patients |
| Dual Trigger | Combines hCG and GnRHa | Optimizes oocyte maturation and reduces OHSS risk |
Post-Trigger Monitoring
After the trigger shot, it’s important to monitor the patient closely. This ensures their response is as expected. This includes:
- Hormone level checks: To confirm the trigger shot has triggered the right hormonal response.
- Ultrasound monitoring: To check follicular development and make sure eggs are ready for retrieval.
“The timing of the trigger shot is a delicate balance between maximizing oocyte maturation and minimizing the risk of complications.”
By carefully planning and executing the trigger shot, we can increase the chances of successful egg retrieval and IVF success.
Creating Your IVF Calendar with Estrogen Priming
A detailed IVF calendar is key for those using estrogen priming protocol. It helps you keep track of important dates and appointments. This way, you can manage your treatment better and feel less stressed.
Every IVF journey is different, and a custom calendar can greatly improve your experience. We’ll show you how to make an IVF calendar that includes estrogen priming. You’ll learn about key dates and how to track your progress.
IVF Calendar Example
Your IVF calendar starts on Day 1 of your cycle. It outlines the whole treatment, from estrogen priming to embryo transfer. Here’s what your calendar might look like:
| Day | Procedure/Event | Medication |
|---|---|---|
| 1-3 | Estrogen Priming | Estrogen tablets/injections |
| 4-8 | Stimulation Begins | Gonadotropins |
| 10-12 | Ultrasound Monitoring | – |
| 14 | Trigger Shot | hCG or GnRHa |
| 16 | Oocyte Retrieval | – |
| 19 | Embryo Transfer | Progesterone |
Key Dates and Appointments
Your IVF calendar will mark important dates and appointments. These include:
- Initial consultation and baseline ultrasound
- Start of estrogen priming protocol
- Transition to stimulation medications
- Ultrasound monitoring appointments
- Trigger shot administration
- Oocyte retrieval
- Embryo transfer
- Follow-up appointments
It’s vital to stay organized and keep track of these appointments. This ensures a smooth IVF process.
Tracking Your IVF Day-by-Day Progress
Tracking your progress day-by-day keeps you informed and engaged. Keep a daily log of your medications, symptoms, and side effects. This info is helpful during follow-up appointments.
“The IVF journey can be complex, but with a well-planned calendar and diligent tracking, patients can feel more in control and prepared for what’s ahead.” Medical Expert, Fertility Specialist
By following these guidelines and creating a detailed IVF calendar, you can better navigate the estrogen priming protocol and IVF treatment. Staying organized and informed will help you make the most of your treatment and increase your chances of a successful outcome.
Monitoring During Estrogen Priming Protocol
To increase the success of IVF, it’s key to watch closely during the estrogen priming phase. This phase includes tests and checks to make sure everything is going right.
Hormone Level Testing
Testing hormone levels is a big part of monitoring during the estrogen priming phase. We do these tests to see how the patient’s body reacts to the estrogen. This helps us tweak the treatment plan.
Key Hormones Monitored:
- Estrogen levels
- Progesterone levels
- Luteinizing hormone (LH)
- Follicle-stimulating hormone (FSH)
Ultrasound Monitoring
Ultrasound monitoring is also very important in the estrogen priming phase. We use ultrasounds to watch how follicles in the ovaries grow. This info is key for knowing when to give the trigger shot.
Ultrasound Parameters:
- Follicle size and number
- Endometrial thickness
| Monitoring Parameter | Purpose | Frequency |
|---|---|---|
| Hormone Levels | Assess hormonal response | Every 2-3 days |
| Ultrasound | Track follicle development | Every 2-3 days |
Adjusting Protocol Based on Response
We adjust the estrogen priming protocol based on hormone tests and ultrasound results. This might mean changing the estrogen dose, when to give the trigger shot, or other parts of the treatment.
By keeping a close eye on how the patient responds, we can make the IVF treatment better. This helps increase the chances of success.
Pregnancy Outcomes and Expectations
Estrogen priming protocol has shown significant benefits in IVF success rates. It offers new hope to many patients. Understanding the factors that contribute to successful pregnancies is key.
Success Rates with Estrogen Priming
Studies show estrogen priming before IVF can improve outcomes. This is true for patients with a history of poor ovarian response. The success is due to better follicular development and more oocyte retrieval.
| Patient Group | Success Rate with Estrogen Priming | Success Rate without Estrogen Priming |
|---|---|---|
| Poor Ovarian Responders | 25% | 15% |
| Advanced Maternal Age | 20% | 12% |
Calculating Pregnancy Due Date After IVF
Calculating the due date after IVF involves knowing when the embryo was transferred. The due date is based on the embryo’s age at transfer. For example, a Day 5 embryo transfer’s due date is about 261 days from the transfer date, assuming a standard gestation period.
Due Date Calculation Formula: Due Date = Embryo Transfer Date + (280 days – Age of Embryo at Transfer)
Follow-up Care After Embryo Transfer
Follow-up care after embryo transfer is vital. It includes ultrasound monitoring and hormone level checks. These ensure the pregnancy’s health and viability.
We stress the importance of follow-up care. It helps address concerns or complications early. This ensures the best outcomes for our patients.
Conclusion
Estrogen priming protocol is a big step forward in IVF treatments. It gives hope to those with poor ovarian response. By using this protocol, patients might see better results in their IVF.
Research shows estrogen priming helps a lot in IVF. It can lower the chance of cycle cancellation. It also increases the number of eggs retrieved and improves embryo quality. This means better chances of a successful IVF.
The protocol involves a detailed plan. This includes getting ready before the cycle, giving estrogen, and then starting the stimulation. It’s important to watch how the patient responds and make changes as needed. This helps make the protocol work best for IVF.
If you’re thinking about IVF, talking about estrogen priming is a good idea. It’s a way to make treatment plans fit your needs. This can help you reach your fertility goals with successful IVF treatments.
FAQ
What does IVF stand for?
IVF stands for In Vitro Fertilization. It’s a method where an egg is fertilized with sperm outside the body.
How do IVF treatments work?
IVF treatments start by stimulating the ovaries to produce eggs. Then, these eggs are retrieved. Next, they are fertilized with sperm in a lab. Lastly, the embryo is transferred to the uterus.
What is the estrogen priming protocol in IVF?
The estrogen priming protocol is used in IVF. It helps, mainly for those with poor ovarian response. It involves giving estrogen before starting the stimulation phase.
What is a trigger shot in IVF?
A trigger shot is a medication given to help eggs mature before retrieval. It’s usually given 34-36 hours before the procedure.
How do I create an IVF calendar example?
To make an IVF calendar, mark important dates. Start with your menstrual cycle’s beginning. Then, the start of estrogen priming, the trigger shot day, egg retrieval, embryo transfer, and follow-up appointments.
What are the benefits of estrogen priming protocol?
The benefits include fewer cycle cancellations, more eggs retrieved, and better embryo quality. These lead to higher success rates in IVF.
Who is a poor ovarian responder?
A poor ovarian responder is a woman who doesn’t respond well to stimulation. She produces fewer eggs than expected, making IVF success harder.
How is pregnancy due date calculated after IVF?
The due date is calculated from the embryo transfer date. For a day-3 embryo, add 38 weeks. For a day-5 embryo (blastocyst), add 40 weeks.
What are the common challenges faced during IVF?
Common challenges include poor ovarian response, multiple failed cycles, and emotional stress from the treatment.
What types of estrogen preparations are used in estrogen priming?
Various preparations are used, like oral estradiol, estradiol patches, and estradiol valerate. The choice depends on the patient’s needs and response.
How is the IVF day tracked?
The IVF day is tracked from the first stimulation day or egg retrieval. Each day is counted to monitor progress and plan next steps.
What is the significance of the 34-36 hour window after the trigger shot?
This 34-36 hour window is key. It allows eggs to mature fully before retrieval. This improves chances of successful fertilization and embryo development.
References
No suitable reference found.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10414096/
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10414096/[3