In vitro fertilization (IVF) creates many IVF embryos, not all of which are used. This leaves patients with tough choices about what to do with them. It’s important to offer caring advice to help them through this hard time.
About 40% of patients don’t know what to do with leftover embryos after IVF. We’ll look at the choices they have, like freezing, donating, or transferring them with care. We’ll also talk about the feelings and legal issues that come with these decisions.
Detailed explanation of the disposal, donation, and storage options for what happens to the unused embryos in in vitro fertilization.
Key Takeaways
- IVF often results in surplus embryos that require careful disposition.
- Patients face difficult decisions regarding the fate of their unused embryos.
- Options for unused embryos include freezing, donation, and compassionate transfer.
- Comprehensive counseling is essential to support patients through this process.
- Emotional and legal considerations play a significant role in embryo disposition decisions.
The IVF Process and Creation of Multiple Embryos
During IVF, many eggs are taken and fertilized, making multiple embryos. This is key to IVF, as it boosts the chance of getting healthy embryos. We’ll look at why extra embryos are made and how they’re handled.
Why IVF Typically Creates Surplus Embryos
IVF makes the ovaries produce lots of eggs, which are then fertilized. This usually means more embryos than can be transferred at once. So, there are extra embryos.
Studies say about 1.5 to 1.9 million embryos are made each year in the U.S. through IVF. The growth of IVF technology has a lot to do with embryo research. Some people might choose to donate their extra embryos for research.
The Embryo Selection Process
Choosing which embryos to transfer is based on their quality and health. Embryologists look at growth rate, shape, and genetic health to pick the best ones.
Initial Patient Decisions During Treatment
Patients starting IVF have to make big decisions early on. They decide how many embryos to transfer and what to do with any extras. These choices depend on age, medical history, and personal views.
| Stage of IVF Process | Description | Outcome |
|---|---|---|
| Ovarian Stimulation | Medications stimulate the ovaries to produce multiple eggs. | Multiple eggs retrieved |
| Egg Retrieval and Fertilization | Eggs are retrieved and fertilized with sperm. | Multiple embryos formed |
| Embryo Culture | Embryos are cultured for 3-5 days. | Embryos assessed for quality |
| Embryo Transfer | One or more embryos are transferred to the uterus. | Pregnancy achieved or not |
| Surplus Embryos | Remaining embryos are frozen for future use. | Embryos available for future transfers |
Statistics on Unused Embryos in the United States
[Add image here]
The number of unused embryos in the US is increasing. This issue affects both IVF patients and clinics. Looking into the statistics, we see a big problem with many facets.
Annual Creation: 1.5-1.9 Million Embryos
Every year, between 1.5 and 1.9 million embryos are made in the US. This number changes because of different IVF cycles and patients. The IVF process makes many eggs to increase the chance of getting pregnant.
Each IVF cycle can make many embryos. Not all are used right away. The extra ones are frozen for later use, adding to the total number of embryos stored.
Current Storage: 600,000 to 1.5 Million Frozen Embryos
There are between 600,000 and 1.5 million frozen embryos in the US. The exact number is hard to know because there’s no single registry. But it’s clear the number is big and keeps growing.
Storing these embryos is a big challenge. Clinics must keep them at the right temperature and handle them carefully. This is to keep them good for future use.
The Growing Challenge of Embryo Accumulation
Unused embryos are a big problem for IVF patients and clinics. Many embryos stay frozen for years or even decades. People face tough choices about what to do with them.
| Category | Estimated Number | Growth Rate |
|---|---|---|
| Annual Embryo Creation | 1.5-1.9 million | 5-7% annually |
| Frozen Embryos in Storage | 600,000 to 1.5 million | 3-5% annually |
| Embryos Discarded Annually | Estimated tens of thousands | Varies by clinic policies |
As more embryos are made, it’s key for clinics, policymakers, and patients to talk about what to do. They must think about the ethics and the practical issues.
Cryopreservation: The Science of Freezing Embryos
The process of freezing embryos, known as cryopreservation, is key in modern IVF. It cools embryos to stop all activity, allowing them to be stored for a long time. This has changed IVF, giving people more time to plan their families.
How Embryo Freezing Works
Freezing embryos is a detailed process that needs precision. The main method today is vitrification, a quick cooling method that keeps the embryo’s structure intact. Vitrification has greatly improved the survival rates of frozen embryos compared to older methods.
The steps for cryopreservation include:
- Preparing embryos for freezing by removing excess water to prevent ice crystal formation.
- Rapid cooling using liquid nitrogen to achieve a glassy state.
- Storage in liquid nitrogen tanks at very low temperatures.
Long-term Viability of Frozen Embryos
Frozen embryos can stay viable for years. Research shows that how long they’re stored doesn’t affect their viability much. The quality of the embryo at freezing time is more important than storage time.
People often ask how long they can store their embryos. While there’s no limit, clinics have rules. New technology is making frozen embryos last longer.
Storage Facilities and Safety Protocols
Storage facilities for embryos have many safety measures. These include:
- Continuous monitoring of storage tanks.
- Backup power supplies to prevent thawing in case of power failure.
- Secure access controls to prevent unauthorized access.
- Regular maintenance and inspection of equipment.
Clinics also have strict rules for tracking and managing embryos. This ensures patient information is correct and up-to-date. This careful approach gives patients peace of mind when freezing embryos for later use.
What Happens to the Unused Embryos in In Vitro Fertilization
IVF treatments often leave patients with extra embryos. This is because IVF aims to create many embryos to boost the chances of success. Patients then face the task of deciding what to do with these extra embryos.
Overview of the Five Main Disposition Options
There are five main ways to handle unused embryos. These include freezing them for later use, donating them to other couples, donating them to research, doing a compassionate transfer, or discarding them. Each choice has its own emotional and practical aspects.
- Continued Freezing: Embryos can be stored for future use, allowing for more pregnancies without another egg retrieval.
- Donation to Other Couples: Couples can donate their embryos to others who are struggling with infertility, giving them a chance at pregnancy.
- Donation to Scientific Research: Embryos can be donated to help advance medical research, potentially leading to better fertility treatments and health improvements.
- Compassionate Transfer: Some clinics offer a compassionate transfer, where the embryo is transferred at a time when pregnancy is unlikely, providing a more natural end.
- Discarding: Couples may choose to discard their embryos, a choice that can be emotionally tough but is a valid option.
Factors Influencing Patient Decisions
The decision on what to do with unused embryos is deeply personal. It is shaped by ethical, religious, and personal beliefs. Clinic counselors and policies help guide patients through these choices.
| Factor | Influence on Decision |
|---|---|
| Ethical Considerations | Patients’ moral beliefs about embryos can greatly affect their choices. |
| Religious Beliefs | Religious teachings can guide patients’ decisions on embryo disposition. |
| Personal Circumstances | Family size, financial situation, and future plans can influence the decision. |
Clinic Policies and Consent Forms
Clinics discuss disposition options with patients before treatment starts. Patients then sign consent forms showing their preferences. These policies and forms differ between clinics, highlighting the need for clear communication and understanding of options.
By understanding the options and factors involved, patients can make informed decisions that match their personal values and circumstances.
Option 1: Continued Freezing for Future Family Building
Freezing embryos gives hope and flexibility to those looking into IVF. It lets patients keep embryos for later use. This might mean fewer egg retrievals, saving on costs and physical stress.
Storage Timeframes and Considerations
Choosing to freeze embryos means thinking about how long they can stay frozen. Clinics have rules on how long embryos can be stored. This time can be a few years or even decades.
It’s key to ask about your clinic’s storage rules and any future changes. Also, know how to renew storage agreements and any costs involved. This keeps your embryos ready for when you’re ready to use them.
Annual Costs and Financial Implications
Freezing embryos costs money each year, depending on where you go. The yearly cost can be between $500 and $1,000. Think about these costs when planning for the future, if you’re storing for a long time.
| Storage Duration | Average Annual Cost | Total Cost |
|---|---|---|
| 1-3 years | $500-$1,000 | $500-$3,000 |
| 4-6 years | $500-$1,000 | $2,000-$6,000 |
| 7-10 years | $500-$1,000 | $3,500-$10,000 |
Success Rates with Previously Frozen Embryos
Freezing embryos can lead to successful pregnancies. The CDC says the success rate is between 43-45% with embryo donation. This shows frozen embryos can work well for IVF.
Success depends on:
- Embryo quality when frozen
- Freezing and thawing methods
- Health of the patient and uterus
Talk to your doctor about your chances of success. This helps you make the best choice for your frozen embryos.
Option 2: Embryo Donation to Other Couples
Donating embryos after IVF is a kind act for those with extra embryos. It helps other couples build their families. This act also brings joy and closure to the donors.
The Donation Process and Requirements
The embryo donation process has several steps. These include screening, matching, and legal agreements. Clinics check donors’ health and mental state to ensure the embryos are good and the donors are okay.
Key steps in the donation process include:
- Initial consultation and screening
- Matching with recipient couples
- Legal contracting and consent forms
- Embryo thawing and transfer
The cost of donating embryos can be between $5,000 and $15,000. This covers matching, screenings, counseling, shipping, and the transfer itself.
Anonymous vs. Known Donation
Donors can choose between anonymous and known donation. Anonymous means no contact, while known allows for some connection.
The choice depends on personal feelings and situations. Some like the privacy, while others want to stay connected.
Legal and Emotional Considerations
Donating embryos has legal and emotional sides. Donors give up all rights, and recipients take full responsibility. Donors might feel happy, sad, or a mix of emotions.
Counseling helps donors deal with these feelings. Clinics also explain the legal parts, making sure everyone knows their roles.
Donating embryos changes lives for the better. It helps families grow and gives donors a sense of purpose and happiness.
Option 3: Donating Embryos to Scientific Research
Donating embryos to research is a big decision. It involves thinking deeply about ethics and emotions. For many, it’s a way to help others and advance medicine.
Types of Research Using Donated Embryos
Donated embryos help in many research areas. This includes studying how embryos grow, stem cell research, and why some pregnancies fail. These studies can improve our understanding of human growth and IVF success.
Medical Expert, “Donating embryos for research can change how we see early human growth. It can also make IVF treatments better.”
“The use of donated embryos in research has already led to significant breakthroughs in our understanding of stem cells and their therapeutic uses.”
Medical Expert, Stem Cell Researcher
The Consent Process and Restrictions
Donating embryos for research requires informed consent. Patients must know what their embryos will be used for and the benefits. Clinics and research places have strict rules to make sure donations are made with full understanding.
Some key parts of the consent process are:
- Clear information about the research purposes
- Understanding of the embryo’s possible uses
- Assurance of anonymity or confidentiality, if desired
- Option to withdraw consent at any time before the research starts
Potential Scientific Advancements
Donating embryos to research can lead to big steps forward in medicine. It has helped in creating new stem cell treatments, understanding genetic disorders, and improving IVF.
| Research Area | Potential Benefits |
|---|---|
| Stem Cell Research | Development of new therapies for various diseases |
| Embryonic Development Studies | Improved understanding of early human development and possible causes of infertility |
| Genetic Disorder Research | Better understanding and possible treatments for genetic conditions |
As we keep moving forward in reproductive medicine, donating embryos to research is key. It helps us make progress. By knowing the benefits and what to consider, people can make choices that fit their values and goals.
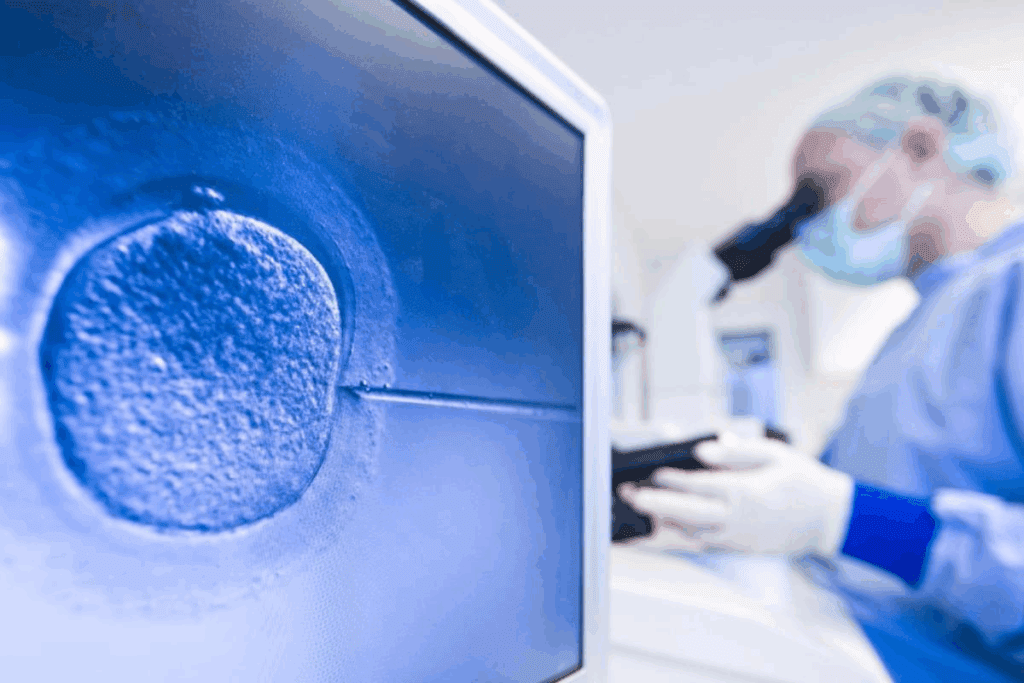
Option 4: Compassionate Transfer Explained
IVF often leaves us with extra embryos. One option is the compassionate transfer. It’s a way to transfer embryos when pregnancy is unlikely. This approach is both dignified and emotionally significant.
The Procedure and Timing
Compassionate transfer happens during the luteal phase or when pregnancy is unlikely. This timing is key. It lets patients avoid a conventional pregnancy but also gives them a chance for emotional closure.
Key aspects of the procedure include:
- Coordination with the patient’s menstrual cycle to determine the optimal timing
- Preparation of the uterus to receive the embryo
- A gentle transfer process similar to a standard embryo transfer
Emotional and Ceremonial Aspects
For many, the compassionate transfer is a meaningful goodbye to their embryos. It’s a therapeutic and cathartic experience. It helps them find closure. Some clinics add ceremonial elements to this process.
“For many, the compassionate transfer is a moment of healing, a way to honor the life while acknowledging reality.”
Medical Expert, Fertility Specialist
Clinics differ in how they support this process. But the goal is always to be compassionate and respectful.
Availability and Provider Policies
Not all clinics offer compassionate transfer. Its availability depends on the clinic’s policies, local laws, and the patient’s situation. Patients should ask about this option when talking to their fertility specialist.
| Clinic | Compassionate Transfer Offered | Additional Services |
|---|---|---|
| Clinic A | Yes | Ceremonial support, counseling |
| Clinic B | No | N/A |
| Clinic C | Yes | Counseling, support groups |
Options like compassionate transfer show the importance of personalized care in fertility treatment.
Option 5: Discarding Unused Embryos
Choosing to discard unused embryos is a tough decision for many. It’s influenced by personal beliefs, ethics, and the emotional bond with the embryos.
Standard Disposal Methods in Clinical Practice
Fertility clinics have set rules for disposing of embryos. Most doctors put embryos in special containers for disposal. These containers are handled according to the clinic’s rules, showing respect and following laws.
- Embryos go into a special waste container.
- Trained staff handle the disposal, following strict rules.
- Some clinics let patients be part of the disposal, if they want.
Variations in Procedures Across Facilities
Even with standard practices, how embryos are disposed of can differ. Some places offer more personal options, like letting patients be there or holding a memorial. It’s key for patients to ask about their clinic’s policies.
- Ask about disposal policies when first visiting the clinic.
- Knowing the clinic’s procedures helps patients make better choices.
- Some clinics might charge extra for special disposal requests.
Ethical and Emotional Considerations
Deciding to discard embryos is more than a medical choice. It’s also emotional and ethical. Getting support from counselors or groups can help with these feelings.
Choosing to discard embryos is a personal decision. It’s easier when patients know all about the process and its meaning.
Conclusion: Navigating Complex Decisions About Unused Embryos
Patients going through IVF often face tough choices about unused embryos. IVF makes many embryos, with about 1.5 to 1.9 million made each year in the U.S. Knowing what happens to these embryos is key to making good choices.
We looked at different options, like freezing embryos for later, donating them to others, or using them for research. Each choice has its own emotional, legal, and financial aspects.
Clinics and support groups help a lot in making these tough decisions. They help patients understand their options and make choices that fit their values and needs. Whether it’s deciding how many embryos to use or what to do with the rest, having support is vital.
In the end, the choice about unused embryos is personal. It depends on the individual’s situation and what they prefer. We suggest patients look into their options carefully and talk to healthcare experts to make the best choice for them.
FAQ
What happens to embryos that are not used in IVF?
Unused embryos can be frozen for later use, donated to other couples, or used in research. They can also be transferred compassionately or discarded.
How are frozen embryos destroyed?
Frozen embryos are thawed and then thrown away. Some clinics offer compassionate transfer as an option.
Does IVF kill embryos?
IVF itself doesn’t kill embryos. But, it can create more embryos than needed, leading to surplus.
How many embryos are destroyed in IVF each year?
It’s hard to say exactly. But, hundreds of thousands of embryos are not used each year in the U.S.
How are IVF embryos discarded?
Embryos are thawed and then disposed of. Clinics follow safe protocols, like incineration, for disposal.
How many embryos are discarded in IVF?
The number varies. But, many embryos are stored or discarded because they’re not used.
Does IVF destroy embryos?
IVF can lead to surplus embryos. These may be frozen, donated, or discarded. But, IVF itself isn’t destructive.
How many embryos are created during IVF?
The number varies. But, it’s common for IVF to create multiple embryos. In the U.S., it’s estimated to be 1.5-1.9 million annually.
How many frozen embryos are there in the US?
There are between 600,000 to 1.5 million frozen embryos in the U.S.
What is compassionate transfer IVF?
Compassionate transfer is a procedure. It allows patients to transfer their frozen embryos at a special time. It often includes ceremonial aspects, unlike thawing and discarding.
Can I donate embryos after IVF?
Yes, you can donate unused embryos. This allows them to help other couples or aid in research.
What happens to left over sperm?
Leftover sperm can be frozen for later use, donated, or discarded. Clinic policies determine the disposal method.
References
Sengupta, D.K., & Herkowitz, H.N. (2003). Lumbar spinal stenosis: Treatment strategies and indications for surgery. Orthopedic Clinics of North America, 34(2), 281-295. https://pubmed.ncbi.nlm.nih.gov/12914268/