Endometriosis is a chronic condition where tissue like the uterine lining grows outside the uterus. It causes debilitating pain and infertility in millions of women worldwide. Laparoscopy is a key tool for diagnosis and treatment, providing a minimally invasive approach. It can greatly improve the quality of life for those affected.Detailed discussion of endometriosis surgery risks and when it is recommended for infertility.
We will look at the role of laparoscopy for endometriosis. This procedure allows for both diagnosis and treatment in one operation. By understanding when endometriosis laparoscopy is needed, women can take a big step towards managing their condition and getting their health back.
Key Takeaways
- Laparoscopy is a key procedure for diagnosing and treating endometriosis.
- It offers a minimally invasive approach with potentially fewer complications.
- The procedure can significantly reduce pain and improve fertility outcomes.
- Understanding the benefits and risks is key for making informed decisions.
- Laparoscopy can be a transformative step in managing endometriosis.
Understanding Endometriosis and Its Impact

Learning about endometriosis starts with knowing its symptoms and how common it is. This condition affects women’s health, emotions, and social lives.
What Is Endometriosis?
Endometriosis is a long-term condition where tissue like the uterus lining grows outside the uterus. This tissue thickens and bleeds with each cycle, causing pain and discomfort.
Understanding endometriosis is key to managing its symptoms and improving life for those affected.
Prevalence and Demographics
About 5-10 percent of women of childbearing age have endometriosis. It can happen to any woman, but is often found in women in their 30s and 40s.
| Age Group | Prevalence of Endometriosis |
|---|---|
| 15-24 years | 1 in 10 women |
| 25-34 years | 1 in 8 women |
| 35-44 years | 1 in 7 women |
Common Symptoms and Their Severity
Endometriosis can lead to pelvic pain, heavy or irregular periods, and infertility. The severity of these symptoms varies among women.
Common symptoms include:
- Pelvic pain or cramping
- Heavy or prolonged menstrual bleeding
- Infertility or difficulty conceiving
- Digestive issues during menstruation
By understanding endometriosis, we can improve diagnosis and treatment. This helps in better care and support for those with the condition.
Non-Surgical Management Options for Endometriosis

Many women try different non-surgical treatments before surgery for endometriosis. Each person’s experience with endometriosis is unique. What works for one may not work for another.
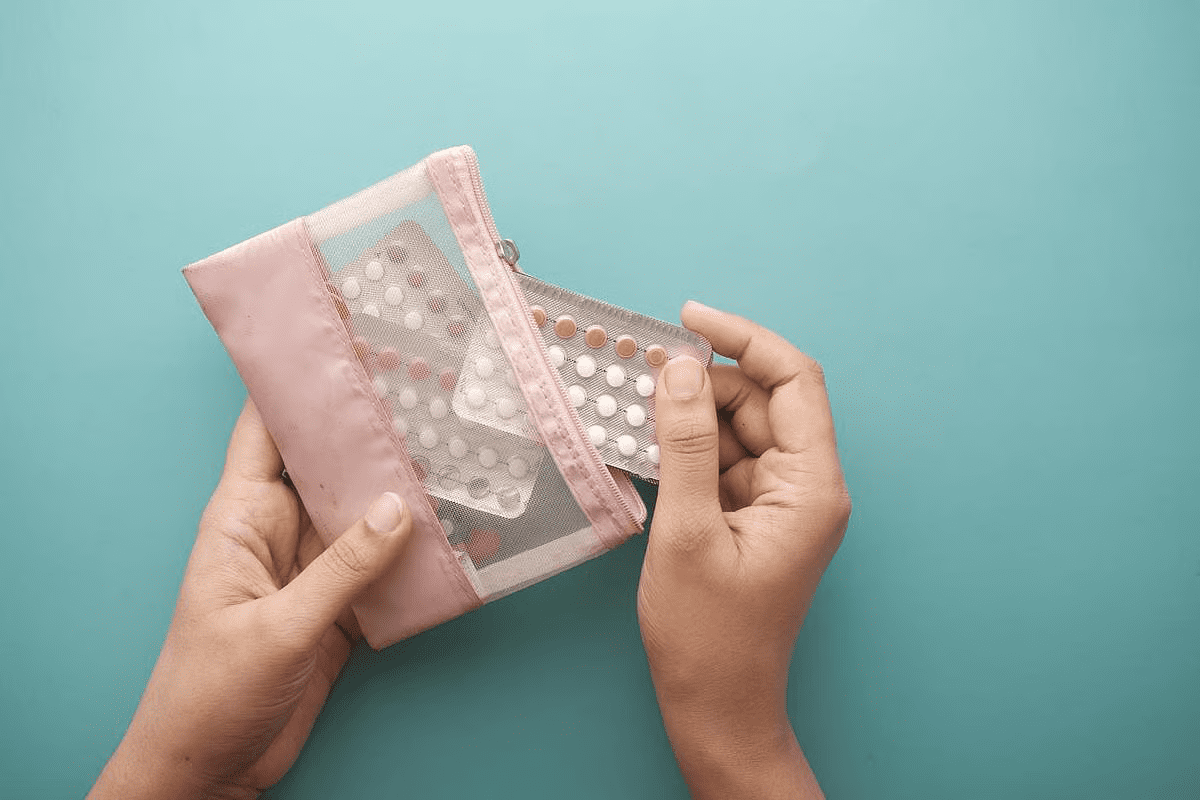
Hormonal Treatments
Hormonal treatments are a common way to manage endometriosis symptoms. They aim to lower estrogen levels. This can help reduce the growth of endometrial tissue.
- Birth Control Pills: Continuous use can help reduce menstrual cramps and heavy bleeding.
- Progestin Therapy: Progestin can help reduce endometrial growth and alleviate symptoms.
- Gonadotropin-Releasing Hormone (GnRH) Agonists: These medications can create a menopause-like state, reducing symptoms.
A study in the Journal of Clinical Endocrinology and Metabolism found hormonal treatments can significantly reduce symptoms in many women.
“Hormonal therapies are effective in reducing pain and improving quality of life for women with endometriosis.”
Pain Management Approaches
Pain management is key in treating endometriosis. There are various ways to manage pain effectively.
| Pain Management Method | Description | Benefits |
|---|---|---|
| Over-the-Counter Pain Relievers | Medications like ibuprofen or acetaminophen | Easy to access, effective for mild to moderate pain |
| Prescription Pain Medications | Stronger medications for severe pain | Effective for severe pain management |
| Alternative Therapies | Acupuncture, physical therapy, etc. | Holistic approach, can be used alongside conventional treatments |
When Conservative Treatments Fail
Some women may find their symptoms persist or worsen over time. In such cases, surgical options like laparoscopy may be considered.
It’s important for patients to work closely with their healthcare providers. This helps determine the best treatment. Laparoscopy can be a viable option for those who don’t find relief with conservative treatments.
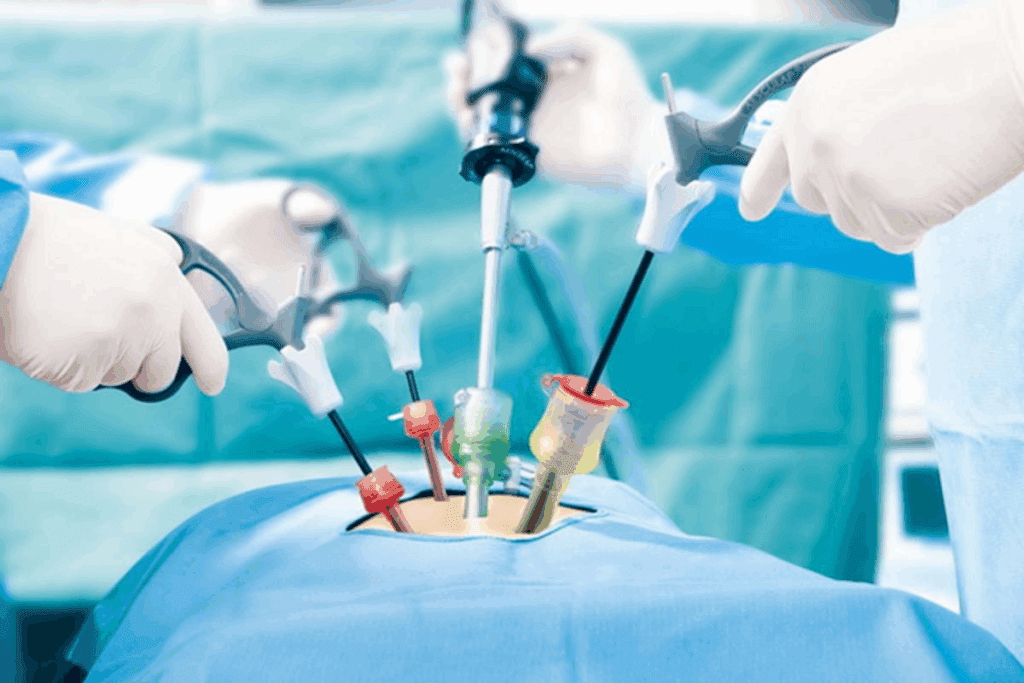
What Is Laparoscopic Surgery for Endometriosis?
Laparoscopic surgery is a key option for women with endometriosis. It’s a minimally invasive method. Small cuts in the belly allow for a thin tube with a camera and light, and tools to remove lesions.
Many find surgery scary, but laparoscopic surgery is preferred. It’s precise and has less recovery time. It can also diagnose and treat endometriosis at the same time.
The Laparoscopy Procedure Explained
The surgery starts with a small cut near the belly button for the laparoscope. This lets the surgeon see inside and find endometrial implants or adhesions. More small cuts are made for tools to remove the tissue.
Diagnostic vs. Operative Laparoscopy
Laparoscopy can be for both diagnosis and treatment. It can show where endometriosis is and how much. Then, it can treat it right away, making it a one-step process.
Excision vs. Ablation Techniques
There are two ways to remove endometrial lesions: excision and ablation. Excision cuts out the lesions. Ablation uses heat or laser to destroy them. The choice depends on the lesions’ size, location, and the surgeon’s skill.
Knowing the difference between these methods helps in making treatment choices. It’s important to talk to your doctor about what’s best for you.
Key Indicators You Should Consider Laparoscopy
Women with endometriosis may need laparoscopic surgery for several reasons. This surgery is considered when symptoms are severe or other treatments don’t work well.
Persistent Pain Despite Medical Treatment
Persistent pain that medical treatments can’t fix is a big sign for laparoscopy. Women with chronic pelvic pain, dysmenorrhea, or dyspareunia might find relief here.
Chronic pain makes daily life hard. If hormonal treatments or pain meds don’t help, laparoscopy can be a good option.
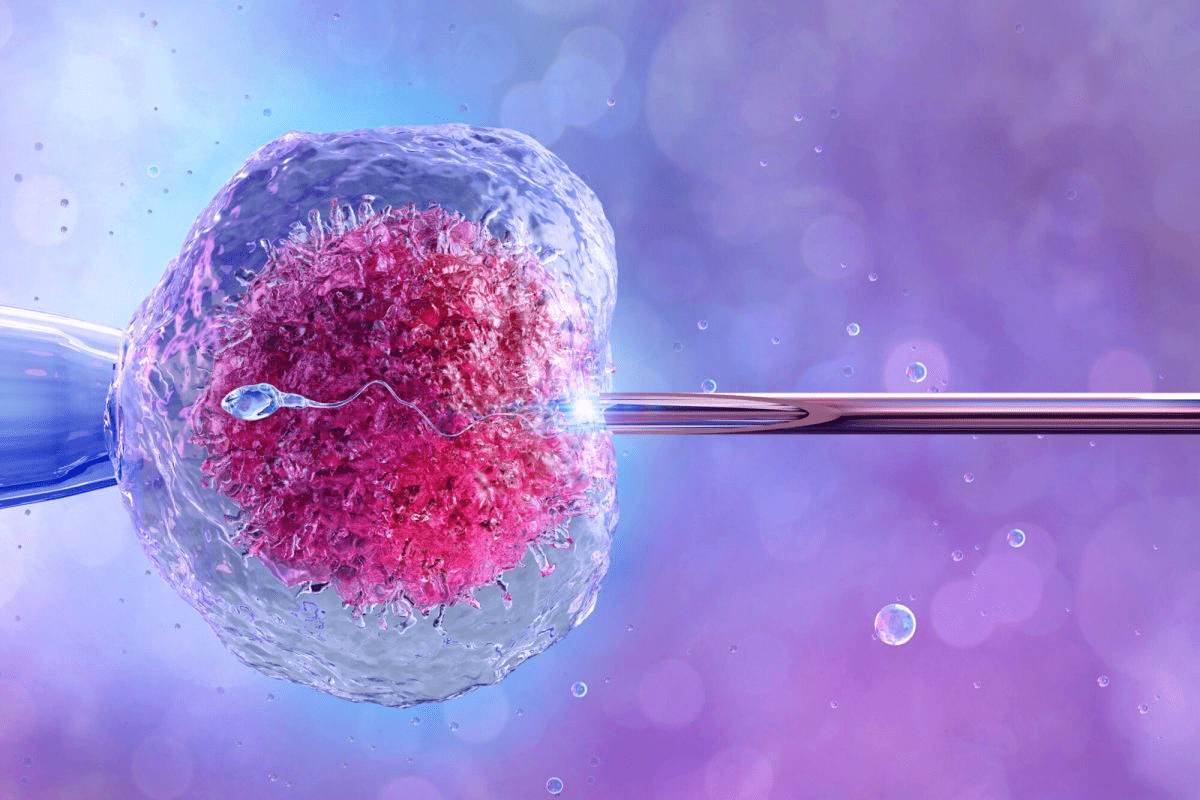
Fertility Concerns
Fertility issues are another reason for laparoscopy. Women having trouble getting pregnant might get help from surgery to remove lesions or fix damaged organs.
Research shows laparoscopy can help with fertility in endometriosis patients. It can fix the problems that make it hard to conceive.
Suspected Deep Infiltrating Endometriosis
Deep infiltrating endometriosis (DIE) is a serious form of endometriosis. It’s when endometrial tissue gets into other tissues and organs. If you think you have DIE, laparoscopy is a good choice.
DIE causes a lot of pain and discomfort. Laparoscopy lets doctors see and treat the problem directly.
Large Endometriomas
Large endometriomas, or chocolate cysts, are painful and can affect fertility. Surgery is often needed to remove them and ease symptoms.
| Indicator | Description | Benefit of Laparoscopy |
|---|---|---|
| Persistent Pain | Chronic pelvic pain not relieved by medical treatment | Diagnostic and therapeutic relief |
| Fertility Concerns | Difficulty conceiving due to endometriosis | Improved fertility outcomes |
| Deep Infiltrating Endometriosis | Severe endometriosis infiltrating surrounding tissues | Thorough examination and removal of affected areas |
| Large Endometriomas | Ovarian cysts causing pain and fertility issues | Removal of cysts to alleviate symptoms |
Benefits of Laparoscopic Surgery for Endometriosis
Laparoscopic surgery is a top choice for treating endometriosis. It’s known for being less invasive and offers many benefits. These include better diagnosis, treatment, and recovery times.
Minimally Invasive Approach
Laparoscopic surgery is less invasive than traditional surgery. It uses small incisions for instruments and a camera. This means less damage, lower infection risk, and less scarring.
Simultaneous Diagnosis and Treatment
This surgery can diagnose and treat endometriosis at the same time. The surgeon can see the lesions, check their size, and remove or destroy them. This saves time and reduces the need for more surgeries.
Improved Fertility Outcomes
Research shows laparoscopic surgery can boost fertility in women with endometriosis. It removes lesions and adhesions, helping the ovaries work better. This increases the chances of getting pregnant.
Pain Relief Success Rates
Many women find relief from pain after laparoscopic surgery. The success rate depends on the disease’s severity and the surgery method. But, a lot of patients see a decrease in pain.
| Benefits | Description | Outcomes |
|---|---|---|
| Minimally Invasive | Small incisions, less tissue damage | Less scarring, reduced infection risk |
| Simultaneous Diagnosis and Treatment | Visualization and removal of lesions | Reduced need for multiple surgeries |
| Improved Fertility | Restoration of normal pelvic anatomy | Enhanced conception chances |
| Pain Relief | Removal or destruction of endometrial lesions | Reduction in pain symptoms |
Endometriosis Surgery Risks and Possible Complications
It’s important to know the risks and possible complications of laparoscopic surgery for endometriosis. This surgery is generally safe but has some risks that patients should be aware of.
Common Side Effects
After laparoscopic surgery for endometriosis, you might feel some discomfort, bloating, and fatigue. These symptoms are usually mild and go away within a few days.
Serious Complications
Though rare, serious complications can happen. These might include damage to organs, infection, or bleeding. It’s important to know about these risks and talk to your healthcare provider.
Risk Factors That Increase Surgical Complications
Some factors can make complications more likely during or after laparoscopic surgery for endometriosis. These include:
- Previous pelvic surgery
- Presence of deep infiltrating endometriosis
- Large endometriomas
- Underlying medical conditions
Talking to your healthcare provider about these risk factors can help you understand how they might affect your surgery.
| Risk Factor | Description | Potential Impact |
|---|---|---|
| Previous Pelvic Surgery | Scarring and adhesions from previous surgeries | Increased risk of complications during surgery |
| Deep Infiltrating Endometriosis | Endometriosis that penetrates deeply into tissues | Higher risk of organ damage during surgery |
| Large Endometriomas | Cysts related to endometriosis that are large in size | Increased risk of rupture or infection |
Knowing about these risks and possible complications helps patients prepare for what might happen with laparoscopic surgery for endometriosis.
Preparing for Your Laparoscopic Procedure
Getting ready for your laparoscopic procedure can make you feel less anxious and improve your results. Knowing what to expect is important. We’ll help you get ready for your surgery.
Pre-Surgical Consultations and Tests
You’ll have many tests and talks with your doctor before surgery. These steps are key to planning your surgery. Your doctor will look at your medical history, talk about your symptoms, and explain the surgery.
Pre-surgical tests may include:
- Imaging studies like ultrasound or MRI to see how bad the endometriosis is
- Blood tests to check for any health issues that might affect surgery
- A physical check-up to see how you’re doing overall
These tests help your team understand your situation and plan the best surgery for you.
What to Expect on Surgery Day
On surgery day, you’ll get special instructions about eating, drinking, and taking medicine. It’s very important to follow these to stay safe during the surgery.
Here’s what you might experience on surgery day:
- Arriving at the hospital or surgical center, where you’ll get ready for surgery
- Getting anesthesia to make sure you’re comfortable during the surgery
- The surgical team will do the laparoscopic procedure, which usually takes 1-2 hours
After surgery, you’ll go to a recovery area. There, you’ll be watched until you’re ready to go home.
Insurance and Cost Considerations
Understanding the costs of laparoscopic surgery for endometriosis and insurance can be tricky. It’s important to talk about this with your doctor and insurance before surgery.
Key things to consider include:
- Checking if your insurance covers laparoscopic surgery for endometriosis
- Knowing any costs you might have to pay yourself
- Talking about payment plans if you’re not fully covered
Knowing about costs and insurance can help you financially prepare for your surgery.
Recovery After Laparoscopic Endometriosis Surgery
The journey to recovery after laparoscopic endometriosis surgery has several stages. Each stage is important for a smooth healing process. Proper care after surgery helps avoid complications and ensures the best results.
Immediate Post-Operative Period
The first hours after surgery are key for a good recovery. Patients are watched in the recovery room for a few hours to manage pain and any issues.
During this time, we focus on:
- Managing pain effectively
- Monitoring for any signs of complications
- Ensuring the patient is stable before discharge
Effective pain management is a top priority. We use a mix of medicines and other methods to reduce pain.
Short-Term Recovery Timeline
The time it takes to recover varies, but most can get back to normal in a few weeks. Here’s a general guide:
| Time Frame | Expected Recovery Progress |
|---|---|
| 1-3 days | Rest and recovery at home; gradual return to light activities |
| 1-2 weeks | Return to most normal activities; some restrictions on heavy lifting or strenuous exercise |
| 4-6 weeks | Full recovery expected; return to all normal activities, including exercise |
Long-Term Follow-Up and Monitoring
Long-term follow-ups are key for managing endometriosis. We suggest regular visits to check for any signs of the condition coming back. We also address any ongoing symptoms or worries.
Understanding the recovery process and following post-operative instructions helps avoid complications. Our team is dedicated to providing full care throughout the recovery journey.
Special Considerations for Different Types of Endometriosis
Endometriosis comes in many forms, each needing its own treatment plan. It’s not one treatment fits all. We must tailor care to each type’s unique needs.
Superficial Peritoneal Endometriosis
Superficial peritoneal endometriosis grows on the peritoneal surface. It often causes inflammation and adhesions. Removing these growths can help manage symptoms and improve life quality.
Key considerations: The size of the growths, adhesions, and the patient’s health are key in choosing treatment.
Ovarian Endometriomas
Ovarian endometriomas, or “chocolate cysts,” are filled with old blood. They can cause a lot of pain and increase the risk of ovarian cancer.
Management strategies: Removing them surgically is often advised, but it must weigh against risks and fertility preservation.
Deep Infiltrating Endometriosis
Deep infiltrating endometriosis (DIE) is a severe form. It deeply invades tissues and organs, causing a lot of pain and affecting bowel and bladder function.
Treatment challenges: DIE needs specialized surgery and a team effort to manage symptoms and restore function.
Bowel and Bladder Involvement
Endometriosis in the bowel or bladder can cause a lot of suffering. Symptoms include painful bowel movements and frequent urination.
| Type of Involvement | Common Symptoms | Treatment Approaches |
|---|---|---|
| Bowel Involvement | Painful bowel movements, constipation | Surgical resection, bowel shaving |
| Bladder Involvement | Urinary frequency, painful urination | Partial cystectomy, ureterolysis |
In conclusion, knowing the different types of endometriosis and their unique features is key to effective care. Tailoring treatment to each patient’s needs can lead to better outcomes and a better quality of life.
Recurrence and Repeat Surgeries
Endometriosis can come back after surgery, and it depends on many things. Knowing what affects it helps set realistic goals and make smart choices about treatment.
Frequency of Laparoscopic Surgeries for Endometriosis
How often you can have laparoscopic surgery for endometriosis varies. It’s not the same for everyone. The first time you have it, how bad it is, the surgery method, and aftercare all matter.
A study in the Journal of Minimally Invasive Gynecology showed that about 10% of people experience a comeback at one year. By two years, it’s 20%, and by three years, it’s 30%. But, these numbers can change based on your situation.
Factors Influencing Recurrence
Many things can make endometriosis come back after surgery. These include:
- The severity of the initial endometriosis condition
- The surgical technique used (e.g., excision vs. ablation)
- The completeness of the surgery
- Post-surgical hormonal therapy
- The patient’s age and overall health
Medical Expert, a leading expert, says, “The best way to lower the chance of it coming back is to remove it all and manage well after surgery.”
“The best way to lower the chance of it coming back is to remove it all and manage well after surgery.” – Medical Expert
| Factor | Influence on Recurrence |
|---|---|
| Initial Severity | Higher severity increases recurrence risk |
| Surgical Technique | Excision generally has lower recurrence rates than ablation |
| Post-Surgical Hormonal Therapy | Can significantly reduce recurrence risk |
Post-Surgical Maintenance Strategies
To lower the chance of it coming back, there are things you can do after surgery. These include:
- Hormonal therapies to stop endometriosis from growing
- Lifestyle changes, like diet and exercise
- Regular check-ups with your healthcare provider
By using these strategies, you can lower your risk of it coming back and live better.
Conclusion: Making an Informed Decision About Endometriosis Surgery
When looking at treatment options for endometriosis, knowing your choices is key. Laparoscopic surgery is a good option, helping with diagnosis and treatment. We’ve looked at the good and bad sides of laparoscopic surgery for endometriosis.
Deciding on endometriosis surgery means understanding the condition and the surgery’s benefits and risks. It also includes knowing how to care for yourself after surgery. This way, patients can make smart choices about their treatment.
Choosing laparoscopic surgery for endometriosis depends on your situation and what your doctor says. We suggest talking to a healthcare provider about your options. This will help figure out the best treatment for you.
FAQ
What is laparoscopy and how is it used in diagnosing and treating endometriosis?
Laparoscopy is a minimally invasive surgery. It helps diagnose and treat endometriosis. A laparoscope is inserted through a small incision in the abdomen. This allows doctors to see the pelvic area and find endometrial lesions.
How often can you have laparoscopic surgery for endometriosis?
The number of times you can have laparoscopic surgery varies. It depends on your symptoms, how severe the disease is, and your health. Each case is different, and the decision to have more surgeries is made based on how well previous ones worked and if symptoms come back.
What are the benefits of laparoscopic surgery for endometriosis?
Laparoscopic surgery has many benefits. It’s a minimally invasive method that can diagnose and treat endometriosis at the same time. It can also improve fertility and reduce pain. This surgery can remove lesions, treat adhesions, and shrink endometriomas.
What are the risks and possible complications of laparoscopic surgery for endometriosis?
Laparoscopic surgery is generally safe but carries risks. These include infection, bleeding, and injury to nearby organs. Though rare, serious complications can include damage to the bowel, bladder, or major blood vessels. It’s important to understand these risks and talk to your healthcare provider.
How do I prepare for a laparoscopic procedure for endometriosis?
Preparing for surgery involves several steps. You’ll have consultations and tests to check your health and the extent of endometriosis. On surgery day, you’ll get instructions on fasting, medication, and what to bring. It’s also important to know about insurance and costs.
What is the recovery process like after laparoscopic endometriosis surgery?
Recovery starts with rest right after surgery. It can take a few days to a few weeks to fully recover. It’s important to follow up with your doctor to watch for any signs of the disease coming back and to manage symptoms or fertility concerns.
Can laparoscopic surgery improve fertility outcomes for women with endometriosis?
Yes, laparoscopic surgery can help with fertility. It removes lesions, endometriomas, and adhesions that can affect reproductive health. The success depends on the disease’s severity and individual factors.
How is deep infiltrating endometriosis treated with laparoscopic surgery?
Treating deep infiltrating endometriosis requires skill. Laparoscopic surgery uses excision techniques to remove deep lesions. It can significantly improve symptoms and quality of life.
What are the strategies for post-surgical maintenance to minimize the risk of endometriosis recurrence?
After surgery, maintenance strategies include hormonal treatments and pain management. Lifestyle changes can also help. Regular check-ups with your doctor are key to monitoring for recurrence and adjusting treatment as needed.
Is it possible to have bowel or bladder involvement with endometriosis, and how is it treated?
Yes, endometriosis can affect the bowel or bladder. Specialized surgery is needed to treat these cases. Laparoscopic surgery is effective, often requiring a team of specialists in gastrointestinal or urological surgery.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8428328/