Choosing between ICSI and conventional IVF can be tough for couples. Both are well-known fertility treatments. But, recent studies show they work differently under various conditions orgasm after iui.
At Liv Hospital, we know how important it is to know the success rates. ICSI means injecting a single sperm into an egg. Conventional IVF mixes eggs and sperm in a dish. The success rate for ICSI is about 30-35% for women under 35.
We’ll look at the differences between ICSI and conventional IVF. We’ll talk about their success rates and what affects them. This will help you make a smart choice for your fertility treatment.
Key Takeaways
- ICSI and conventional IVF have different approaches to achieving pregnancy.
- Success rates vary depending on individual circumstances.
- Understanding the differences between ICSI and conventional IVF is key for making informed decisions.
- Fertility treatment success rates are influenced by many factors.
- Liv Hospital offers full support for international patients looking for fertility treatments.
Understanding Assisted Reproductive Technologies

Assisted Reproductive Technologies (ART) have changed the world of fertility care. They bring hope to those facing infertility. We’ll look at how these technologies have evolved and their role in today’s fertility treatments.
The Evolution of Fertility Treatments
Fertility treatments have grown a lot. The first In Vitro Fertilization (IVF) was successful in the late 1970s. Now, ART includes many techniques, like Intracytoplasmic Sperm Injection (ICSI).
Research and technology have driven these advancements. Today, these treatments are more advanced. They offer better success rates and more choices for those facing fertility issues.
The Role of ART in Modern Fertility Care
ART is key in modern fertility care. It solves many fertility problems. These technologies are vital for those with complex fertility issues.
| Type of ART | Description | Common Indications |
|---|---|---|
| Conventional IVF | Fertilization occurs in the lab | Unexplained infertility, tubal damage |
| ICSI | Sperm injected directly into the egg | Male factor infertility, previous IVF failure |
Knowing about ART and its uses helps people choose their fertility treatments. Our fertility specialists help patients pick the best treatment for them. They consider each person’s unique situation.
What is Conventional IVF?
Conventional IVF is a well-known fertility treatment. It involves several steps to increase the chances of getting pregnant. This traditional method has been a key part of fertility treatments for many years.
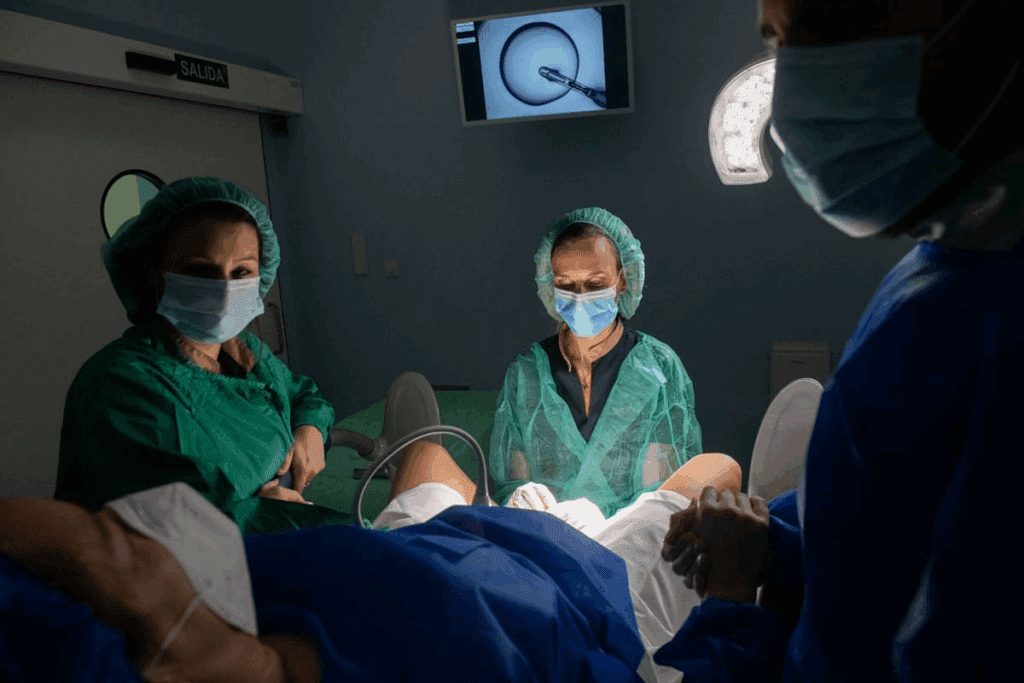
The Process of Traditional IVF
The IVF process starts with ovarian stimulation. This is when medications help the ovaries produce many eggs. Then, the eggs are monitored to see how they grow.
- Ovarian stimulation: Medications are given to stimulate the ovaries.
- Egg retrieval: A minor surgery is done to get the eggs.
- Sperm collection: The male partner gives a semen sample.
- Fertilization: Eggs and sperm are mixed in the lab for fertilization.
- Embryo culture: The fertilized eggs (now embryos) are kept in the lab for 3-5 days.
- Embryo transfer: One or more embryos are put into the woman’s uterus.
Throughout this process, patients get help and support from fertility specialists. This ensures the best results.
When Conventional IVF is Recommended
Conventional IVF is suggested for many fertility problems. These include:
- Female factor infertility, like tubal damage or endometriosis.
- Unexplained infertility, when other treatments fail.
- Male factor infertility, but sometimes ICSI is used with conventional IVF.
The choice to do conventional IVF is based on a detailed check-up. This includes looking at age, medical history, and past fertility treatments.
In summary, conventional IVF is a very effective and common fertility treatment. Knowing about the process and when it’s used helps people make better choices about their fertility care.
What is Intracytoplasmic Sperm Injection (ICSI)?
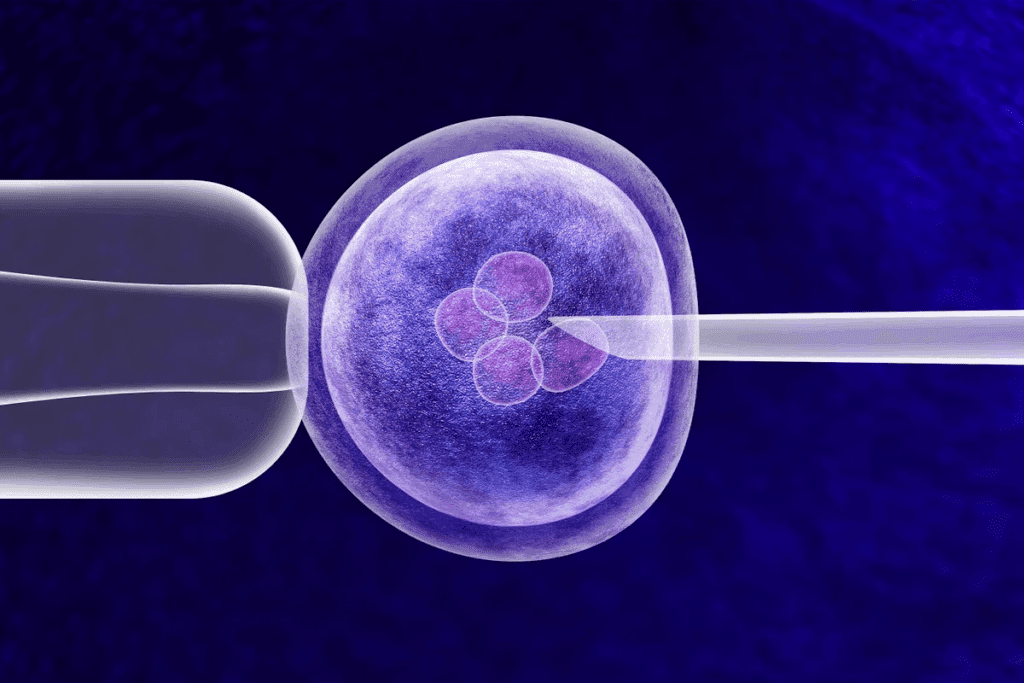
ICSI, or Intracytoplasmic Sperm Injection, is a special IVF method. It involves injecting a single sperm into an egg. This method has changed how we treat male infertility and is key in assisted reproductive technologies.
The ICSI Procedure Explained
The ICSI process has several steps. First, eggs are taken from the female partner like in regular IVF. At the same time, a semen sample is prepared from the male partner. An embryologist picks a healthy sperm and injects it into the egg using a special microscope.
Key steps in the ICSI procedure include:
- Egg retrieval
- Semen sample preparation
- Selection and immobilization of a single sperm
- Microinjection of the sperm into the egg
- Fertilization assessment
- Embryo culture
- Embryo transfer
Indications for ICSI Treatment
ICSI helps couples with male infertility issues. This includes low sperm count, poor motility, or abnormal shape. It’s also used when previous IVF attempts failed or didn’t work well.
Common indications for ICSI include:
| Indication | Description |
|---|---|
| Male Factor Infertility | Low sperm count, poor motility, or abnormal morphology |
| Previous Fertilization Failure | Failed or poor fertilization in previous IVF cycles |
| Severe Male Infertility | Conditions such as azoospermia requiring surgical sperm retrieval |
| Unexplained Infertility | Cases where the cause of infertility is not clearly identified |
Understanding ICSI and its uses helps couples make better choices for fertility treatments. Our fertility experts offer personalized care and advice during the ICSI journey.
ICSI vs Conventional IVF: Key Differences
When looking into fertility treatments, knowing the differences between ICSI and conventional IVF is key. Both have changed the world of fertility, giving hope to those facing infertility.
Fertilization Method Comparison
The main difference is in how they fertilize eggs. Conventional IVF mixes eggs with sperm in a dish, letting nature take its course. ICSI, on the other hand, injects a single sperm into an egg directly.
ICSI is great for men with low sperm count or poor motility. It helps get past natural barriers to fertilization, boosting chances of success.
Laboratory Techniques and Technology
ICSI and conventional IVF use different lab techniques and tech. ICSI needs special tools and skills for precise egg and sperm handling. This advanced micromanipulation technique requires a lot of expertise from embryologists.
Conventional IVF also uses advanced lab tools but doesn’t need the same level of precision as ICSI. Yet, both benefit from new lab tech, like time-lapse imaging, which improves success rates.
Cost Considerations
Cost is a big factor when comparing ICSI and conventional IVF. ICSI is pricier because of its specialized techniques and equipment. The extra cost comes from the procedure’s complexity and the need for skilled embryologists.
While cost matters, it’s important to think about the benefits and success rates of each method. We’ll look at success rates in the next sections to help you understand their effectiveness better.
Fertilization Rates: ICSI vs Conventional IVF
ICSI and conventional IVF have different fertilization rates. These rates are key in fertility care. They help patients and doctors choose the best treatment.
Understanding Fertilization Success Metrics
Fertilization rate is a key measure in ART. It shows how many eggs are fertilized in IVF or ICSI cycles. For IVF, success means one sperm gets into the egg. ICSI injects a sperm directly into the egg, skipping natural barriers.
Fertilization success in IVF is typically measured by:
- The number of eggs retrieved
- The number of eggs fertilized
- The quality of sperm and eggs
Comparative Fertilization Statistics
Studies show ICSI has higher fertilization rates than IVF. ICSI fertilizes 50-80% of eggs, while IVF fertilizes about 50%. This is because ICSI directly injects sperm, helping with male infertility issues.
Even with higher rates, choosing between ICSI and IVF depends on many factors. These include infertility causes, sperm quality, and past treatment results. Knowing these stats helps make treatment plans fit each patient’s needs.
Pregnancy Success Rates by Age Group
Knowing how age impacts pregnancy success is key for those thinking about IVF or ICSI. Age plays a big role in how well these treatments work.
Women Under 35
Women under 35 see high success rates with IVF and ICSI. They tend to have better quality eggs. This leads to higher fertilization and pregnancy chances.
- IVF Success Rates: Women under 35 usually see IVF success rates between 40% to 50% per cycle.
- ICSI Success Rates: ICSI success rates for this age group are also high, often between 45% to 55% per cycle.
Women 35-40
Women in their 35-40s see success rates drop for both IVF and ICSI. Egg quality and quantity decrease. This makes getting pregnant harder.
- IVF Success Rates: Women aged 35-40 usually see IVF success rates between 25% to 35% per cycle.
- ICSI Success Rates: ICSI success rates for women in this age group are often between 30% to 40% per cycle.
Women Over 40
Women over 40 face even lower success rates for IVF and ICSI. Egg quality and quantity drop a lot. This makes getting pregnant very challenging.
- IVF Success Rates: Women over 40 usually see IVF success rates below 20% per cycle.
- ICSI Success Rates: ICSI success rates for women over 40 are generally similar to IVF, often below 20% per cycle.
In conclusion, age is a big factor in IVF and ICSI success. Women under 35 have the best chances. As age goes up, success rates go down. This shows why age matters when planning fertility treatments.
Live Birth Rates: The Ultimate Measure of Success
In the world of fertility treatments, live birth rates are the top measure of success. They show how well treatments like ICSI and IVF work. We’ll look at the live birth rates for both, giving you insights into their success.
ICSI Live Birth Statistics
ICSI has changed how we treat male infertility, with high success rates in live births. Studies show ICSI can match IVF success rates, even with male infertility issues.
Key Statistics:
- Live birth rate per ICSI cycle: 25-30% for women under 35
- Success rates remain robust even with male factor infertility
Conventional IVF Live Birth Statistics
Conventional IVF has a strong track record for live births, mainly when female infertility is the main issue. The success of IVF depends on egg quality and ovarian reserve.
Key Statistics:
- Live birth rate per conventional IVF cycle: 30-40% for women under 35
- Higher success rates observed in cases of female factor infertility
Factors Affecting Live Birth Outcomes
Many factors can change live birth rates for ICSI and IVF. These include:
- Maternal age
- Embryo quality
- Uterine health
- Underlying fertility issues
Knowing these factors helps set realistic hopes and make better choices about fertility treatments.
| Treatment Type | Age Group | Live Birth Rate |
|---|---|---|
| ICSI | Under 35 | 27% |
| ICSI | 35-40 | 20% |
| Conventional IVF | Under 35 | 35% |
| Conventional IVF | 35-40 | 25% |
When ICSI Offers Better Success Rates
ICSI is great for couples with specific fertility problems that regular IVF can’t solve. It has changed how we treat certain types of infertility. This has greatly improved success rates in tough cases.
Male Factor Infertility Cases
For couples dealing with male factor infertility, ICSI is a big help. Male factor infertility means problems with the male partner’s sperm. This could be low count, poor motility, or abnormal shape. ICSI injects a single sperm directly into an egg, getting past natural barriers.
Research shows ICSI boosts fertilization rates when male factor infertility is a problem. It does this by picking a healthy sperm for injection, even if there’s a low count or poor motility.
Previous Fertilization Failure
Couples who failed to fertilize with regular IVF might find success with ICSI. If eggs didn’t fertilize before, ICSI could be a good next step.
Choosing ICSI after IVF failure depends on many factors. These include sperm and egg quality, the age of the couple, and why fertilization failed before.
Other Clinical Indications
ICSI is also beneficial for other reasons. This includes when sperm is taken out surgically or when using frozen sperm with lower motility.
It’s also recommended when there are concerns about sperm quality or when eggs or embryos need to be saved for later.
| Clinical Indication | Conventional IVF Success Rate | ICSI Success Rate |
|---|---|---|
| Male Factor Infertility | Low to Moderate | High |
| Previous Fertilization Failure | Low | Moderate to High |
| Surgically Retrieved Sperm | Low | High |
Knowing when ICSI is more effective helps couples choose the best fertility treatment.
When Conventional IVF May Be Preferable
ICSI has changed how we treat male infertility. But, conventional IVF is better in some cases. We’ll look at when conventional IVF is the best choice, helping you understand your options.
Unexplained Infertility
For unexplained infertility, conventional IVF is often the first choice. It lets doctors check how well eggs and sperm can fertilize without ICSI. This method can be very effective for couples with unexplained infertility, avoiding more complex treatments.
Female Factor Infertility
Conventional IVF is simpler when female factor infertility is the main issue. Problems like ovulation issues, tubal damage, or endometriosis can be tackled with IVF. This natural process can boost the chances of fertilization, focusing on the female side of fertility.
Potential Risks of Unnecessary ICSI
Using ICSI when it’s not needed can raise costs and risks. ICSI injects a sperm into an egg, which is effective for some issues but not all. It can also increase the risk of egg damage and treatment costs. So, conventional IVF is a better choice for some fertility problems.
Knowing when to choose conventional IVF helps couples make better decisions about their fertility treatments.
Conclusion: Making an Informed Decision About ICSI vs IVF
Choosing between ICSI and conventional IVF is a personal choice. It depends on your situation, like the cause of infertility and what you prefer. We’ve looked at the main differences between these two methods, including how they work, when to use them, and their success rates.
When deciding between icsi vs ivf, think about your own situation and medical history. For example, if male infertility is the issue, ICSI might be the best choice. But if it’s unexplained or female factor infertility, conventional IVF could be better.
In the end, making an informed decision means knowing both options well. It’s wise to talk to a fertility expert. They can help figure out the best treatment for you based on your needs and situation.
FAQ
What is the difference between ICSI and conventional IVF?
ICSI (Intracytoplasmic Sperm Injection) involves injecting a single sperm into an egg. Conventional IVF mixes eggs with sperm in a lab dish, letting fertilization happen naturally.
What are the success rates for ICSI compared to conventional IVF?
Success rates for ICSI and conventional IVF depend on age and infertility causes. ICSI often has higher fertilization rates. But, overall success rates, like pregnancy and live birth, are similar for both.
When is ICSI recommended over conventional IVF?
ICSI is often chosen for male infertility, like low sperm count. It’s also used when conventional IVF has failed before.
What are the advantages of conventional IVF?
Conventional IVF is good for unexplained or female infertility. It’s also cheaper than ICSI and helps see how sperm and eggs interact.
How do age and fertility treatment success rates relate?
Age greatly affects fertility treatment success. Success rates drop with age, more so after 35 for both ICSI and conventional IVF.
What is the fertilization rate for ICSI compared to conventional IVF?
ICSI usually has a higher fertilization rate than conventional IVF. This is true, even more so for male infertility issues.
Are there any risks associated with ICSI?
Yes, ICSI carries risks like multiple pregnancies and genetic issues in offspring. These are common with any fertility treatment.
How do live birth rates compare between ICSI and conventional IVF?
Live birth rates for ICSI and conventional IVF are often the same. But, they can change based on infertility reasons and age.
Can ICSI be used for unexplained infertility?
ICSI can be used for unexplained infertility. But, conventional IVF might be a better first choice. It helps check sperm-egg interaction.
What factors influence the success of ICSI and conventional IVF?
Success for both ICSI and conventional IVF depends on age, infertility cause, egg and sperm quality, and clinic expertise.
References
National Center for Biotechnology Information. ICSI vs. Conventional IVF: Success Rates and Considerations. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9650435/