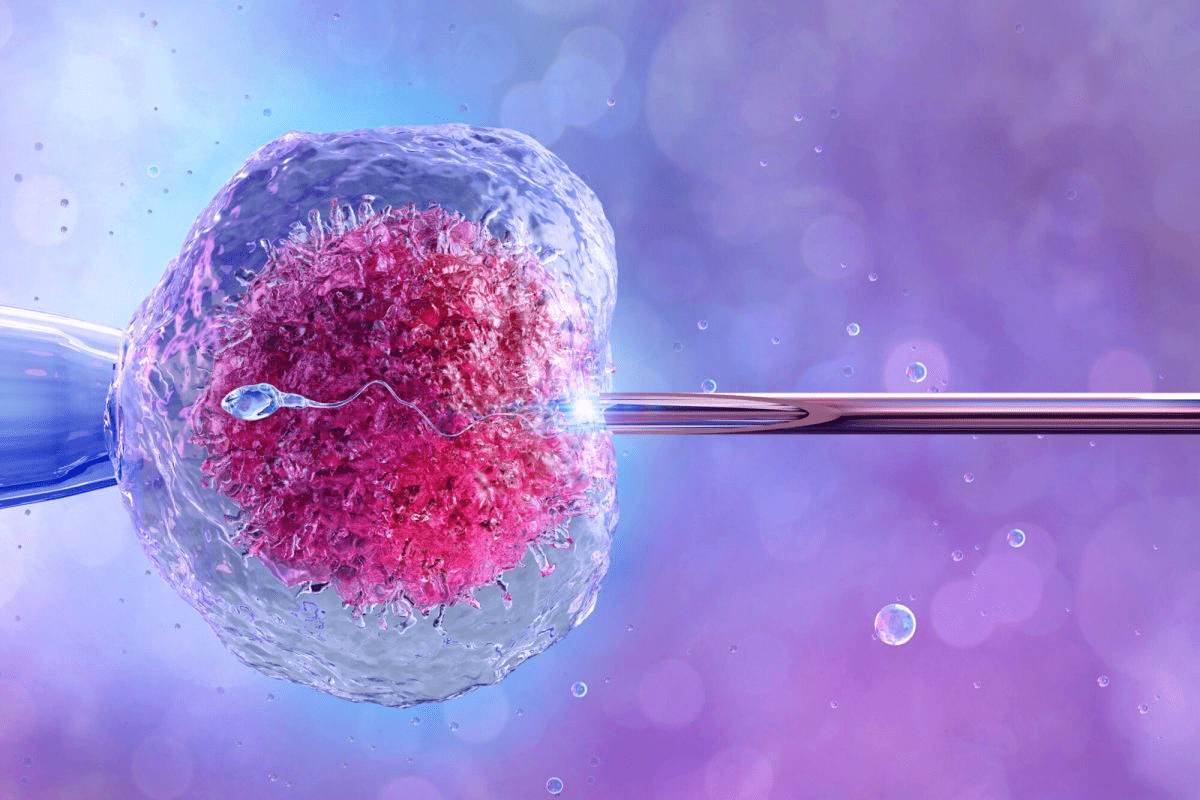
Many couples wonder how many IVF transfers it takes to succeed. While some get pregnant right away, most need more than one try. It’s a big part of the journey to starting a family.
Worldwide, over 12 million babies have been born thanks to IVF and other ARTs. At Liv Hospital, we know that things like maternal age, embryo quality, and medical history matter a lot. These factors help decide if IVF will work for you.
We aim to give a full picture of what affects IVF success. We want to help you know what to expect on your IVF path.
Key Takeaways
- Cumulative IVF success rates improve with multiple cycles.
- Maternal age is a significant factor in IVF success.
- Embryo quality affects the likelihood of successful IVF transfers.
- Individual medical factors influence IVF outcomes.
- Liv Hospital offers personalized care protocols for IVF patients.
The Basics of IVF Transfer Success Rates
Embryo transfer success rates are key in IVF, showing how likely a pregnancy is. Knowing these rates helps set realistic goals and make better choices during IVF.
Single Embryo Transfer Success Rates
Single embryo transfer (SET) is gaining favor for its lower risk of multiple pregnancies. Success rates for SET range from 20-30% in wealthy countries. These rates can change based on the woman’s age, embryo quality, and the clinic’s skill.
“The key to successful IVF lies in selecting the right embryo for transfer.” This highlights the critical role of choosing the best embryo for SET success.
Understanding Live Birth Rates vs. Pregnancy Rates
It’s important to know the difference between live birth rates and pregnancy rates in IVF. Pregnancy rates show how many women get pregnant after IVF. Live birth rates, on the other hand, show how many women actually have a baby. Cumulative live birth rates, which consider all IVF cycles, give a fuller view of success.
For example, a clinic might say a 40% pregnancy rate per cycle. But the cumulative live birth rate over three cycles could be much higher. This offers a more hopeful view for those going through IVF.
“Cumulative live birth rates tell a more complete story about IVF success, giving hope to many who undergo treatment.”
How Many IVF Transfers Before Success: Statistical Overview

Knowing the stats on IVF transfers is key to setting realistic hopes during treatment. Success rates in IVF can change a lot. This depends on age, embryo quality, and how many transfers are done.
Looking at IVF transfer stats gives us important info. For women starting treatment at 30-31, 48% get pregnant after one cycle. This number goes up to 61% after two cycles and 67% after three cycles. This shows that even after the first try, there’s a good chance of getting pregnant with more cycles.
Average Number of Transfers Needed
How many IVF transfers it takes to succeed can vary a lot. Age, how well the ovaries work, and embryo quality all matter. For many women, under 35, it’s usually less than three transfers.
It’s important to remember these numbers are averages. Your own experience might be different. Some might get pregnant right away, while others might need to try a few times.
Cumulative Success Rates After Multiple Cycles
Looking at success rates over many cycles gives a fuller picture. Studies show that success rates keep going up with more cycles. But, the increase might slow down after the third cycle.
For example, data from fertility clinics shows that after three cycles, the chance of a live birth can be between 50% to over 70% for women under 35. This info is key for both patients and doctors when talking about treatment plans and what to expect.
By knowing these stats, people going through IVF can get ready for what’s ahead. They can set realistic hopes and make smart choices about their treatment.
Age as the Primary Factor in IVF Success
IVF success is closely linked to the age of the patient. Younger women generally have higher success rates. As women age, their eggs quality and quantity decline, making IVF more challenging.
We know age is key in IVF success. It’s important to look at how different ages do with IVF.
Success Rates for Women Under 35
Women under 35 have the highest IVF success rates. They tend to have more good-quality eggs, boosting their chances of a successful pregnancy.
Success rates for this age group are generally above 40% per transfer. This makes IVF easier for many women.
Success Rates for Women 35-37
For women between 35 and 37, IVF success rates start to drop slightly. But, they’re not too far off from the top rates.
Recent data shows women in this age group have about 40.5% success rates per IVF transfer.
Success Rates for Women 38-40
Women in their late 30s face more challenges with IVF. Egg quality and quantity decrease, making success harder to achieve.
The success rate for this age group is around 26.4%. This shows IVF becomes more complex in this age range.
Success Rates for Women Over 40
For women over 40, IVF success rates drop significantly. The quality and quantity of eggs are much lower, making pregnancy harder to achieve.
Data shows women over 40 have a success rate of about 8.2% per IVF transfer.
To better understand the impact of age on IVF success, let’s examine the following table:
| Age Group | Success Rate |
|---|---|
| Under 35 | >40% |
| 35-37 | 40.5% |
| 38-40 | 26.4% |
| Over 40 | 8.2% |
Understanding these statistics helps individuals make informed decisions about their IVF journey. It’s important to consider their age and the associated success rates.
Other Factors Affecting IVF Transfer Success
IVF success depends on more than just age. The quality of the embryo and how well the uterus receives it also play big roles. While age matters, other factors can greatly improve IVF results.
Embryo Quality and Grading
Embryo quality is key to IVF success. Experts use a grading system to check how well embryos might do. High-quality embryos have a better chance of implanting.
Studies show that “good” embryos have a 55% implantation rate. Even “poor” embryos have a 1 in 3 chance of leading to a live birth.
Grading looks at the embryo’s development stage, cell count, and cell appearance. This skillful assessment helps predict IVF success.
Uterine Receptivity and Implantation Factors
Uterine receptivity is also vital for IVF success. The uterus must be ready for the embryo, with the right lining thickness and hormonal balance. Any uterine issues can impact implantation.
Other implantation factors include immune system disorders or other conditions. These can affect the embryo’s implantation success. Understanding and managing these factors can boost IVF success rates.
By focusing on embryo quality and uterine readiness, we can increase IVF success. Our fertility team works with patients to optimize these factors for the best results.
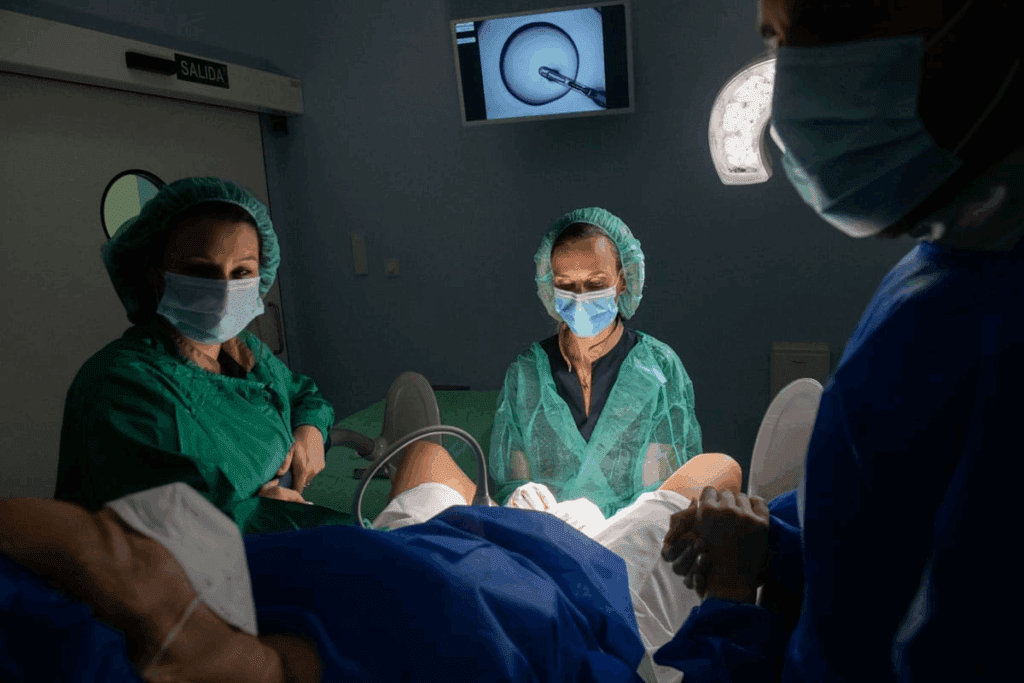
Fresh vs. Frozen Embryo Transfers: Success Rate Comparison
Choosing between fresh and frozen embryo transfers is a big decision in IVF. It affects both success rates and treatment plans. Knowing the differences between these options is key to making the right choice.
IVF has evolved, with frozen embryo transfers (FET) becoming more popular. But why is this, and how do success rates compare?
Benefits of Frozen Embryo Transfers
Frozen embryo transfers are favored for several reasons. They allow for genetic testing before transfer, which boosts success rates. FET also mimics a natural cycle better, as it doesn’t need ovarian stimulation. This can make the uterus more ready for implantation.
Key benefits of FET include:
- Improved success rates due to better embryo selection
- Reduced risk of ovarian hyperstimulation syndrome (OHSS)
- A more natural uterine environment for implantation
Research shows FET can match or even beat fresh transfers in success rates. This is partly because it avoids the negative effects of ovarian stimulation on the endometrium.
| Transfer Type | Success Rate | Key Advantages |
|---|---|---|
| Fresh Embryo Transfer | Variable, often lower than FET | Immediate transfer, no need for freezing |
| Frozen Embryo Transfer (FET) | Generally higher, thanks to genetic testing | Better embryo selection, more natural cycle |
When Fresh Transfers May Be Preferred
Even though FET is popular, fresh transfers are sometimes preferred. This is true when there’s a hurry for genetic testing or when ovarian stimulation is expected to be weak.
Choosing between fresh and frozen transfers should be based on individual needs and medical history.
In summary, both fresh and frozen transfers have their roles in IVF. The trend towards FET is due to its higher success rates and fewer risks. As we move forward in reproductive medicine, understanding these differences is vital for better treatment outcomes.
Single vs. Multiple Embryo Transfers
Choosing between single and multiple embryo transfers is a big decision in IVF. It affects success rates and pregnancy outcomes. Understanding this choice is key to making informed decisions.
Patients and doctors must consider the benefits and risks of each option. Transferring more embryos might increase pregnancy chances. But, it also raises the risk of health problems for the mother and babies.
Success Rates with Multiple Embryo Transfers
Transferring more embryos can boost IVF success, mainly for those with lower chances or past failures. Research shows higher pregnancy rates with multiple transfers, more so for women over 35 or with poor embryo quality.
| Age Group | Single Embryo Transfer Success Rate | Multiple Embryo Transfer Success Rate |
|---|---|---|
| Under 35 | 40-50% | 60-70% |
| 35-37 | 30-40% | 50-60% |
| 38-40 | 20-30% | 40-50% |
The table shows higher success rates with multiple transfers across ages. But, it’s important to think about the risks.
Risks and Considerations of Multiple Embryo Transfers
While multiple transfers can up success rates, they also up the risk of multiple pregnancies. These pregnancies can lead to complications like preterm labor and low birth weight. The American Society for Reproductive Medicine (ASRM) warns of these risks.
“The goal of IVF is not just to achieve a pregnancy, but to ensure the birth of a healthy child. The risks associated with multiple gestations must be carefully weighed against the possible benefits of transferring multiple embryos.”
— ASRM Guidelines
We suggest a personalized approach to decide on embryo transfers. Age, embryo quality, and medical history are key factors.
In conclusion, while multiple embryo transfers can boost IVF success, they also carry big risks. A balanced approach, considering individual factors and guidelines, is vital for the best outcomes.
What to Expect After Failed IVF Transfers
Knowing what to expect after a failed IVF transfer is key. It helps with the emotional and medical sides of fertility treatment. A failed transfer can be tough, but knowing the next steps can guide you.
Next Steps After One Failed Transfer
After one failed IVF transfer, take time to review your treatment. Talk to your healthcare provider about:
- The quality of the embryos transferred
- The uterine receptivity and any factors that might have affected implantation
- Any adjustments to the treatment protocol for future transfers
Don’t forget the emotional side. Seek support from loved ones, groups, or mental health professionals.
Considerations After Two Failed Transfers
After two failed IVF transfers, it’s time for a deeper look at your treatment. Think about:
- The age and its impact on egg or sperm quality
- The number and quality of embryos for future transfers
- Any medical conditions that might affect IVF success
At this point, we might talk about other options like donor eggs or embryos.
Decision-Making After Three or More Failed Transfers
After three or more failed IVF transfers, decisions get harder. Review your treatment history, including:
- Cumulative success rates and the chance of success with more attempts
- The physical and emotional impact of more treatment
- Financial costs and the value of further IVF cycles
Getting a second opinion from a fertility specialist is also wise. We encourage you to think carefully and choose what’s best for you.
In summary, dealing with failed IVF transfers needs a full approach. It’s about medical, emotional, and financial aspects. By understanding what’s next, you can make smart choices for your fertility journey.
Financial and Emotional Considerations for Multiple IVF Cycles
Going through IVF is a big step for individuals or couples. It comes with financial stress and emotional challenges. The journey is filled with hope but also with tough financial and emotional hurdles.
Cost Analysis of Multiple IVF Transfers
The cost of IVF varies a lot. It depends on the clinic, treatment, and if you need extra services like ICSI or genetic testing. A single IVF cycle in the U.S. can cost between $12,000 and $15,000. Medications add another $3,000 to $5,000.
| Service | Average Cost |
|---|---|
| IVF Cycle | $12,000 – $15,000 |
| Medications | $3,000 – $5,000 |
| ICSI | $1,000 – $2,000 |
| Genetic Testing | $2,000 – $4,000 |
For many, the cost of multiple IVF cycles is too much. It’s key to know the costs and look into financial help. This includes insurance and financing plans from fertility clinics.
Emotional Impact and Coping Strategies
IVF can take a big toll on your emotions, even more so with multiple cycles. It’s a mix of hope and disappointment. Finding ways to cope is very important.
“The emotional rollercoaster of IVF can be challenging, but with the right support and coping mechanisms, individuals and couples can navigate this journey more effectively.”
Medical Expert, Fertility Specialist
Ways to cope include talking to loved ones, joining support groups, or doing yoga or meditation. Mental health experts can also offer a lot of help.
It’s vital to understand the financial and emotional sides of IVF. Knowing the costs and challenges helps prepare for the journey. This way, individuals and couples can make better decisions.
Treatment Modifications for Subsequent IVF Transfers
When the first IVF transfer doesn’t work, doctors might suggest changes to help the next cycle succeed. These changes are made just for you, based on what didn’t work before. They aim to fix the issues that led to the failure.
Protocol Adjustments After Failed Transfers
Making changes to the IVF process is key. Medication regimens might be tweaked to get more eggs or better embryos. For example, switching to a minimal stimulation protocol could help if previous cycles didn’t work well.
- Changing the type or dosage of fertility drugs
- Adjusting the timing of egg retrieval
- Modifying the embryo culture conditions
These changes are based on what was learned from before. This includes how well the patient responded to stimulation, embryo quality, and uterine issues.
Add-on Treatments and Their Evidence Base
Some clinics also offer add-on treatments to boost IVF success. These can include assisted hatching, preimplantation genetic testing (PGT), or endometrial scratching.
- Assisted hatching to improve implantation rates
- Preimplantation genetic testing for selecting healthy embryos
- Endometrial scratching to enhance uterine receptivity
Even though these treatments seem promising, it’s important to look at the evidence. Patients should talk to their doctor about the benefits and risks. This helps make the best choice.
By carefully making these changes, patients and doctors can increase the chances of success in future IVF transfers.
When to Consider Donor Eggs or Other Alternatives
For many, exploring donor eggs or other alternatives is a key step towards becoming parents. This choice often hinges on age, egg quality, and past IVF results.
Age-Related Considerations for Donor Options
Age is a big factor in fertility success. As women get older, their eggs quality and number drop, making it harder to get pregnant. Women over 40 often see their IVF success rates with their own eggs plummet. Younger donor eggs can greatly increase their chances.
The American Society for Reproductive Medicine (ASRM) advises women over 35 to consider donor eggs. This is true if they’ve had repeated IVF failures or low egg count.
- Women under 35: They’re not usually considered for donor eggs unless they have other fertility issues.
- Women between 35-40: At this age, thinking about donor eggs starts, mainly if egg quality is a worry.
- Women over 40: For them, donor eggs are often the best choice due to higher success rates.
Success Rates with Donor Eggs vs. Own Eggs
Donor eggs generally lead to higher success rates, even more so for older women. The Society for Assisted Reproductive Technology (SART) shows that live birth rates with donor eggs are higher across all ages.
| Age Group | Live Birth Rate with Own Eggs | Live Birth Rate with Donor Eggs |
|---|---|---|
| Under 35 | 40-50% | 50-60% |
| 35-37 | 30-40% | 50-60% |
| 38-40 | 15-30% | 45-55% |
| Over 40 | 5-15% | 40-50% |
The table clearly shows that donor eggs can significantly boost pregnancy chances, more so for older women. It’s vital to talk to a fertility specialist to find the best option.
Choosing donor eggs or other alternatives should be based on a thorough look at individual circumstances. This includes medical history, age, and personal preferences. Understanding the options and their success rates helps make informed decisions about fertility.
Conclusion: Making Informed Decisions About Your IVF Journey
IVF treatment can be tough to navigate. But knowing what affects success rates can help you make better choices. We’ve looked at how age, embryo quality, and treatment plans play a role.
Understanding these factors helps you see your chances of success more clearly. It’s key to look at success rates, how age affects outcomes, and the differences between fresh and frozen embryo transfers.
As you move forward with IVF, talk to your healthcare provider about your situation and options. This way, you can tailor a treatment plan that fits you best. Knowing all about IVF and its factors is key to making smart decisions.
FAQ
How many IVF transfers before success?
The number of IVF transfers needed for success varies. It depends on age, embryo quality, and how well the uterus accepts the embryo. On average, it takes more than one cycle to get pregnant.
What is the average number of IVF cycles to get pregnant?
It usually takes 2-3 IVF cycles to get pregnant. But, this number can change a lot based on individual factors.
What are the success rates for single embryo transfers?
Success rates for single embryo transfers depend on the embryo’s quality and the individual’s age. They are generally lower than for multiple embryo transfers. But, they also lower the risk of having twins or more.
How do frozen embryo transfers compare to fresh transfers in terms of success rates?
Frozen embryo transfers often have similar or higher success rates than fresh ones. This is because they allow for better timing and uterine readiness.
What are the risks associated with multiple embryo transfers?
Multiple embryo transfers increase the risk of complications. These include health issues for the mother and babies. They also raise the risk of ovarian hyperstimulation syndrome (OHSS).
How does age affect IVF success rates?
Age greatly affects IVF success. Success rates drop with age, more so after 35. Women under 35 usually have better success rates.
What are the benefits of using donor eggs?
Using donor eggs can greatly improve success rates, even for older women. They offer a better chance of a successful pregnancy.
How many embryos are typically transferred during IVF?
The number of embryos transferred varies. It depends on age, embryo quality, and medical history. Usually, one or two embryos are transferred to avoid multiple pregnancies.
What are the next steps after a failed IVF transfer?
After a failed IVF transfer, you might consider changing your treatment plan. You could use add-on treatments or explore donor eggs. Always talk to a healthcare provider to find the best next steps.
How do I cope with the emotional impact of multiple failed IVF cycles?
Dealing with the emotional impact of failed IVF cycles needs support. Get help from loved ones, healthcare providers, and mental health professionals. Self-care, stress management, and looking into other options can help you cope.
Reference
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://academic.oup.com/hropen/article/2020/3/hoaa032/5867220