Knowing about follicle count in IVF is key. Follicles are tiny sacs in ovaries with immature eggs. The number and quality of these follicles greatly affect IVF success rate. ivf vs natural conception
The path to IVF success is complex. While many clinics have goals, individual factors like egg quality and patient age matter a lot. These factors impact how well an egg retrieval goes.
Grasping the link between follicle count and egg retrieval numbers helps. It lets patients have realistic hopes. They can work better with their doctors for a successful IVF cycle.
Key Takeaways
- The number and quality of follicles significantly influence IVF outcomes.
- Individual factors such as egg quality and patient age affect IVF success.
- Understanding follicle count helps in setting realistic expectations.
- Fertility clinics often aim for a certain follicle count benchmark.
- Egg retrieval numbers are closely related to follicle count.
The Role of Follicles in IVF Treatment
Ovarian follicles are key in IVF, affecting both the process and its success. Knowing about follicles is vital for setting realistic goals and improving treatment plans.
What Are Ovarian Follicles?
Ovarian follicles are small, fluid-filled sacs in the ovaries with immature eggs. In a natural cycle, one follicle matures and releases an egg. IVF aims to grow many follicles to get more eggs and better embryos.
Follicle development is a complex process involving hormones and growth factors. “The development of follicles is a critical aspect of IVF, as it directly impacts the number and quality of eggs available for fertilization,” say fertility experts.
How Follicles Develop During Stimulation
In IVF, controlled ovarian stimulation (COS) is used to grow many follicles. This is done with fertility drugs that make the ovaries produce more follicles than usual.
Doctors watch follicle growth closely with ultrasound and hormone tests. This helps them adjust the treatment to grow follicles well without risks like OHSS.
“The key to successful IVF lies in the careful management of follicle development, balancing the need for multiple eggs with the risk of overstimulation.”
Measuring Follicle Size and Maturity
Follicle size and maturity are key for egg retrieval timing. Follicles are ready when they’re about 18-20 mm and hormone levels are right.
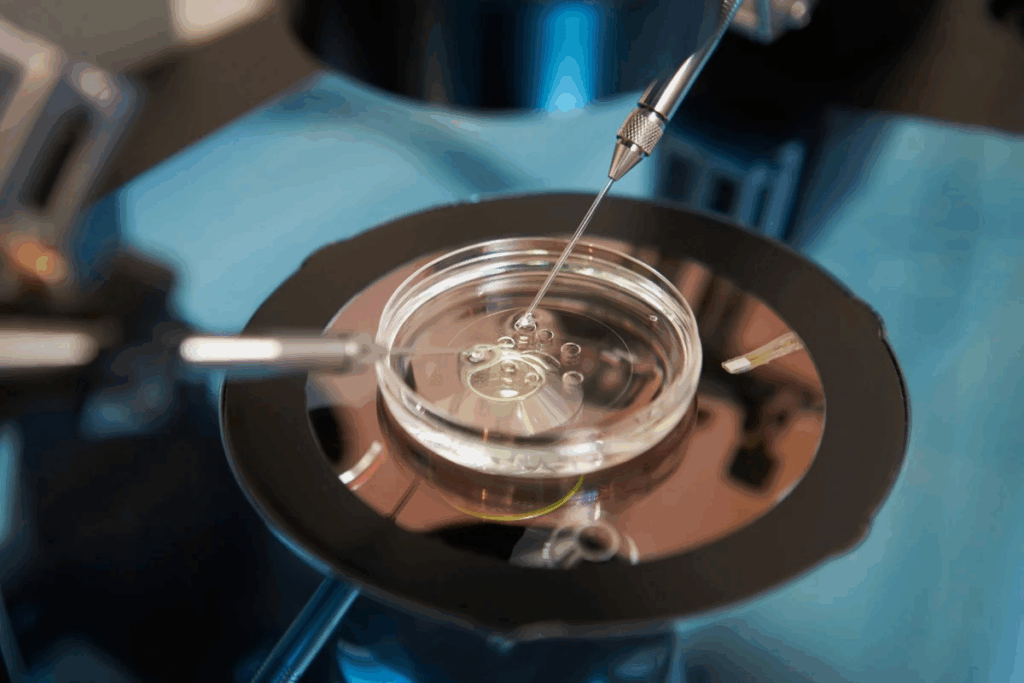
Ultrasound checks follicle size and maturity. These scans help doctors pick the best time for egg retrieval. This increases the chances of successful fertilization and embryo growth.
By managing follicle growth well, fertility specialists can greatly improve IVF success rates. This shows how important follicles are for a successful IVF outcome.
Follicle Count as a Predictor of IVF Success
Follicle count is a key indicator for fertility specialists. It shows how likely IVF will be successful. It also tells about a woman’s ovarian reserve and how she might react to stimulation.
Antral Follicle Count vs. Stimulated Follicles
There are two important follicle counts in IVF: antral follicle count (AFC) and stimulated follicles. The antral follicle count is done early in the cycle. It shows the resting follicles. Stimulated follicles grow with fertility meds during IVF.
AFC gives an early look at ovarian reserve. But, the number of stimulated follicles shows how many eggs might be retrieved. Knowing both helps doctors plan treatments.
Correlation Between Follicle Numbers and Live Birth Rates
Studies link follicle numbers to IVF success. A moderate number (6 to 15) usually means higher success rates. This range offers a good number of eggs while keeping risks low.
Follicle Count Range | Live Birth Rate |
1-5 | Lower success rates due to fewer eggs |
6-15 | Optimal range for most patients, balancing egg number and risk |
16+ | Increased risk of OHSS, potentially reducing success rates |
Why There’s No “Magic Number” for Everyone
While research gives guidelines, individual results can differ a lot. Age, egg quality, and health conditions affect success rates.
It’s key for patients to know their unique situation affects their treatment. Doctors tailor plans for each patient, considering these factors.
4 Follicles IVF Success Rate: What Research Shows
Having 4 follicles during IVF treatment can lead to a reasonable chance of success, according to recent studies. This number, while not considered high, can result in a positive outcome for many patients.
Clinical Outcomes with 4 Mature Follicles
Research shows that the number of mature follicles is key in IVF success. A study published in a leading fertility journal found that patients with 4 mature follicles had a notable pregnancy rate. This rate was lower than those with more follicles.
The quality of the eggs retrieved is also important. Not all follicles yield mature eggs. The health of these eggs is critical for the success of the IVF cycle.
Success Stories and Statistical Realities
While statistical averages give a general outlook, individual success stories show the variability in IVF outcomes.
“We have seen patients with as few as 4 follicles achieve successful pregnancies,” notes a fertility specialist. “It’s a reminder that while numbers are important, they’re not the only factor at play.”
Statistically, more follicles increase the chances of IVF success. But the law of diminishing returns applies. The risk of complications like Ovarian Hyperstimulation Syndrome (OHSS) also rises with higher follicle counts.
When 4 Follicles Can Be Enough
In certain scenarios, 4 follicles can be enough for IVF success. This is true for younger patients or those with a high-quality egg reserve. The key is not just the number of follicles but also their maturity and the quality of the eggs they contain.
For patients with a low ovarian reserve, a tailored approach to IVF can maximize success even with fewer follicles. This may involve adjusting medication protocols or considering alternative treatment options.
5 Follicles IVF: Slightly Better Odds?
The link between follicle count and IVF success is complex. Having 5 follicles might lead to different results than 4. It’s vital to understand how follicle count affects success rates in IVF treatment.
Comparing 4 vs. 5 Follicle Outcomes
Research shows that follicle count during IVF can greatly impact success. When comparing 4 to 5 follicles, several factors are at play:
- Having an extra follicle can mean more eggs, possibly leading to more embryos.
- More embryos can increase the chance of picking healthy ones for transfer.
- But, the quality of these extra eggs and embryos is key to success.
Studies suggest that 5 follicles might offer a slight edge over 4. Yet, the difference is not always big. Many factors, like how well a person responds to IVF, affect success rates.
Research on Marginal Improvements with Each Additional Follicle
IVF research shows that more follicles can slightly improve success rates. But, this gain gets smaller as more follicles are added:
- More than a certain point, extra follicles don’t greatly boost live birth chances.
- More follicles can raise the risk of OHSS.
- Quality of eggs and embryos is always the most important factor.
Adding more follicles makes treatment more complex. Fertility specialists must carefully manage this.
Patient Considerations with 5 Follicles
For patients with 5 follicles, several factors affect IVF success:
- The patient’s age and egg quality are very important.
- How well the body responds to stimulation and the quality of embryos matter a lot.
- Uterine health and overall reproductive health also play a big role.
While 5 follicles might offer a slight advantage over 4, individual factors greatly influence success. Fertility specialists tailor treatment plans to each patient’s unique situation.
The Ideal Follicle Range for IVF Success
Understanding the right number of follicles is key to IVF success. Too few follicles can mean fewer eggs, while too many can lead to complications. So, what’s the perfect number?
Why 6-15 Follicles Is Often Considered Optimal
A follicle count of 6-15 is seen as the best for IVF. This number balances the number of eggs and the risk of ovarian hyperstimulation syndrome (OHSS). It offers enough eggs for fertilization without raising OHSS risk too high.
Balancing Success Rates and OHSS Risk
IVF success depends on finding the right balance. More follicles mean more eggs but also higher OHSS risk. Fewer follicles might mean fewer eggs. The 6-15 range is ideal because it balances both well.
Research Supporting the “Goldilocks Zone” of Follicle Count
Research backs the idea of a “Goldilocks zone” for follicle count in IVF. This range, 6-15 follicles, is not too high or too low. It’s just right for success and safety. A study in a leading fertility journal showed better live birth rates in this range.
Follicle Count Range | Live Birth Rate | OHSS Risk |
0-5 | Low | Low |
6-15 | High | Moderate |
16+ | High | High |
This table shows how follicle count affects live birth rates and OHSS risk. It explains why 6-15 follicles are the best for IVF success.
Egg Retrieval Numbers: Expectations vs. Reality
People looking into IVF often have high hopes for egg retrieval numbers. They might think about how many follicles they have. But, the real numbers can surprise them.
Not All Follicles Yield Mature Eggs
It’s important to know that not every follicle will give a mature egg. The maturity of eggs is a key factor in IVF success. Many follicles might have eggs that aren’t ready or won’t work.
Several things can affect this:
- The quality of the eggs
- The IVF stimulation method
- How well the patient responds to the medication
Average Number of Eggs Retrieved in IVF
The number of eggs retrieved in IVF can vary a lot. Women under 35 usually get more eggs than older women. Clinics report an average of 8 to 15 eggs, based on age and other factors.
Age Group | Average Number of Eggs Retrieved |
<35 years | 10-15 |
35-37 years | 8-12 |
38-40 years | 5-8 |
The Attrition Rate: From Follicles to Viable Embryos
The path from follicles to embryos has a natural drop-off rate. Not all eggs will fertilize, and not all fertilized eggs will become embryos. This is a normal part of IVF.
Things that can affect this drop-off include:
- Egg quality
- Sperm quality
- How the embryos are cultured
Knowing these factors can help manage hopes and make better choices about IVF.
Understanding egg retrieval numbers and what affects them can help patients through their IVF journey. Even if reality doesn’t meet expectations, being informed can make the experience better.
Quality vs. Quantity: Why Egg Quality Matters
In IVF, egg quality is as important as the number of eggs. Having many eggs can help, but it’s the quality that really matters. Good egg quality means better chances for fertilization, implantation, and a healthy baby.
Age-Related Factors in Egg Quality
Age is a big factor in egg quality. As women get older, their eggs get older too. This can lead to genetic damage over time.
Age-related decline in egg quality is a big issue in IVF. Women over 35 may see their egg quality drop faster. This makes it harder to get pregnant.
Genetic Normalcy and Embryo Development
Egg quality affects genetic health and embryo development. Poor-quality eggs often have chromosomal problems. This can cause implantation failure or miscarriage.
Research shows that euploid embryos (with the right number of chromosomes) have a better chance of success. They are more likely to lead to a live birth than aneuploid embryos.
When Fewer High-Quality Eggs Outperform More Poor-Quality Eggs
Having fewer high-quality eggs can be better than many poor-quality ones. High-quality eggs are more likely to be fertilized and develop into healthy embryos. This increases the chances of a successful pregnancy.
Studies have found that one high-quality egg can lead to a successful IVF outcome. But many poor-quality eggs may not result in a viable pregnancy.
Factors Affecting Your Follicle Count
Many factors can change your follicle count during IVF. Knowing these factors helps manage your hopes and improve your treatment plan.
Age and Diminished Ovarian Reserve
Age is a big factor in follicle count. As women get older, their ovaries make fewer eggs. Women under 35 usually respond better to IVF, but those over 40 might face more challenges.
This change happens slowly but gets worse after 35. Knowing how age affects follicle count helps us tailor IVF plans better.
Medical Conditions Impacting Follicle Development
Some medical issues can really affect follicle growth and count. For example, Polycystic Ovary Syndrome (PCOS) can make too many follicles, making IVF harder. On the other hand, Primary Ovarian Insufficiency (POI) can lead to fewer follicles.
Other health problems, like thyroid issues or endometriosis, can also affect the ovaries. It’s key to manage these conditions well before starting IVF.
Medication Protocols and Response Variations
The medications used in IVF can greatly impact follicle count. Different treatments can work differently for each person. Customized treatment plans based on age, weight, and health history help improve follicle growth.
Some people might need to adjust their treatment because of how they react to medications. Watching closely at the start helps find the best treatment.
Lifestyle Factors That May Influence Follicle Development
Lifestyle choices can also affect follicle growth. Keeping a healthy weight is important, as being too heavy or too light can harm the ovaries. Also, smoking can damage the ovaries, reducing follicle count.
While some lifestyle choices are up to us, others are not. We help patients improve what they can control and find ways to deal with what they can’t.
Monitoring Follicle Development During IVF
Monitoring follicle growth is key in IVF. We watch how follicles grow and mature to know when to take eggs. We use ultrasound and hormone tests to guide the treatment for each patient.
Ultrasound Monitoring
Ultrasound is a big part of tracking follicles. We use it to see the ovaries and count follicles. This is done many times in the IVF cycle to adjust the treatment.
Hormone Level Testing
We also test hormone levels to see how well the treatment is working. Estradiol, made by follicles, is what we mostly check. This helps us know when to give the trigger shot.
Timing of the Trigger Shot
The trigger shot is a key step in IVF. It’s given when follicles are ready. We use ultrasound and hormone data to pick the best time for the shot.
Preparing for Egg Retrieval
After the trigger shot, we get ready for egg retrieval. Follicle size and hormone levels help plan the procedure. This planning increases the chances of getting eggs and fertilizing them.
Options for Patients with Low Follicle Counts
Patients facing a low follicle count have many IVF strategies to boost their chances of success. A low follicle count is a challenge, but it doesn’t mean IVF won’t work.
Many patients worry about a low follicle count during IVF. But, there are several ways to increase their chances of success.
Modified Stimulation Protocols
Modified stimulation protocols are a good option for those with low follicle counts. These protocols aim to grow more follicles safely.
- Gentle Stimulation: Lower doses of medications are used to avoid overstimulation.
- Alternative Medications: Different medications might work better for low follicle counts.
- Personalized Protocols: The protocol is adjusted based on how the patient responds.
Multiple Retrieval Cycles and Banking Embryos
Some patients choose to do multiple retrieval cycles and bank embryos. This strategy builds up embryos over time, raising the chances of a healthy embryo for transfer.
Benefits of Multiple Cycles: More chances to get eggs, even with low numbers in each cycle.
Mini-IVF and Natural Cycle Approaches
Mini-IVF and natural cycle IVF are options for low follicle counts. These methods use little or no stimulation.
- Mini-IVF: Uses lower doses of medications to get fewer but higher-quality eggs.
- Natural Cycle IVF: No stimulation is used, relying on the natural cycle for one egg.
These methods are good for those sensitive to fertility meds or worried about overstimulation.
Alternative Family-Building Paths to Consider
Some patients might look into alternative paths to building a family, if traditional IVF isn’t working.
- Donor Eggs: Donor eggs can be very effective for those with very low follicle counts or poor egg quality.
- Adoption: Adoption is a viable option for building a family.
- Surrogacy: Surrogacy involves another woman carrying the pregnancy.
It’s important for patients to talk to their healthcare provider about these options. This helps find the best approach for their situation.
Conclusion: Making Informed Decisions About Your IVF Journey
Understanding follicle count and its role in IVF success is key. This article has covered how follicles affect IVF, the best follicle numbers, and what impacts success.
As you go through IVF, working with your healthcare team is vital. They can tailor your treatment to fit your needs. This includes your age, health, and lifestyle.
It’s important to look at follicle count, egg quality, and other factors together. This way, you can make the best choices for your IVF. It helps you move closer to becoming a parent.
FAQ
What is a good number of follicles for IVF?
The ideal number of follicles for IVF varies. But, 6-15 follicles are often seen as the sweet spot. This balance helps increase the chances of getting multiple eggs while avoiding ovarian hyperstimulation syndrome (OHSS).
How many follicles are needed for a successful IVF cycle?
The number needed can differ. But, 4-5 follicles are usually enough for success. The quality of the eggs and other factors also matter a lot.
What is the average number of eggs retrieved in IVF?
The number of eggs retrieved in IVF varies. It depends on age, ovarian reserve, and more. But, it usually ranges from 8 to 12 eggs.
How does follicle count affect IVF success rates?
Follicle count is key to IVF success. More follicles often mean higher success rates. But, there’s a limit where the risk of OHSS increases.
Can I have a successful IVF with 4 follicles?
Yes, success with 4 follicles is possible. But, the chances are lower than with more follicles. Results can vary a lot.
How does egg quality impact IVF success?
Egg quality is very important for IVF success. High-quality eggs lead to better embryos and pregnancies, even in older women or those with low ovarian reserve.
What factors affect follicle count during IVF?
Many things can affect follicle count. These include age, medical conditions, treatment protocols, and lifestyle. Working closely with a healthcare provider is key to optimizing treatment.
How is follicle development monitored during IVF?
Monitoring follicle development involves ultrasound and hormone tests. These help decide the best time for the trigger shot and egg retrieval.
What are my options if I have a low follicle count?
If follicle count is low, options include modified treatment plans, multiple cycles, or alternative paths like egg donation or adoption.
Is it possible to improve follicle count for IVF?
Some factors affecting follicle count can’t be changed, like age. But, lifestyle and treatment protocols can be improved. This might help increase follicle count and IVF success.