In vitro fertilization (IVF) has changed family planning for millions facing infertility. At Liv Hospital, we think it’s key to know the pros and cons of assisted reproduction before making a choice.
IVF mixes eggs from the female partner with sperm from the male in a lab. This method has many benefits. Yet, studies show important IVF disadvantages that patients need to understand.
IVF is used in about 1 to 3 percent of births in developed countries. We’ll look at the main challenges of IVF. This will help you understand the risks involved.
Key Takeaways
- Understanding the pros and cons of IVF is essential for patients.
- IVF is associated with increased pregnancy complications.
- The risk of congenital malformations is higher with IVF.
- IVF can have significant financial and emotional demands.
- Patients should be aware of the possible risks and considerations.
Understanding In Vitro Fertilization (IVF)
In vitro fertilization, or IVF, is a complex process that has changed many lives. It offers a solution to infertility, helping couples and individuals have children. For those facing infertility, IVF is a beacon of hope.
What is IVF and How Common is it?
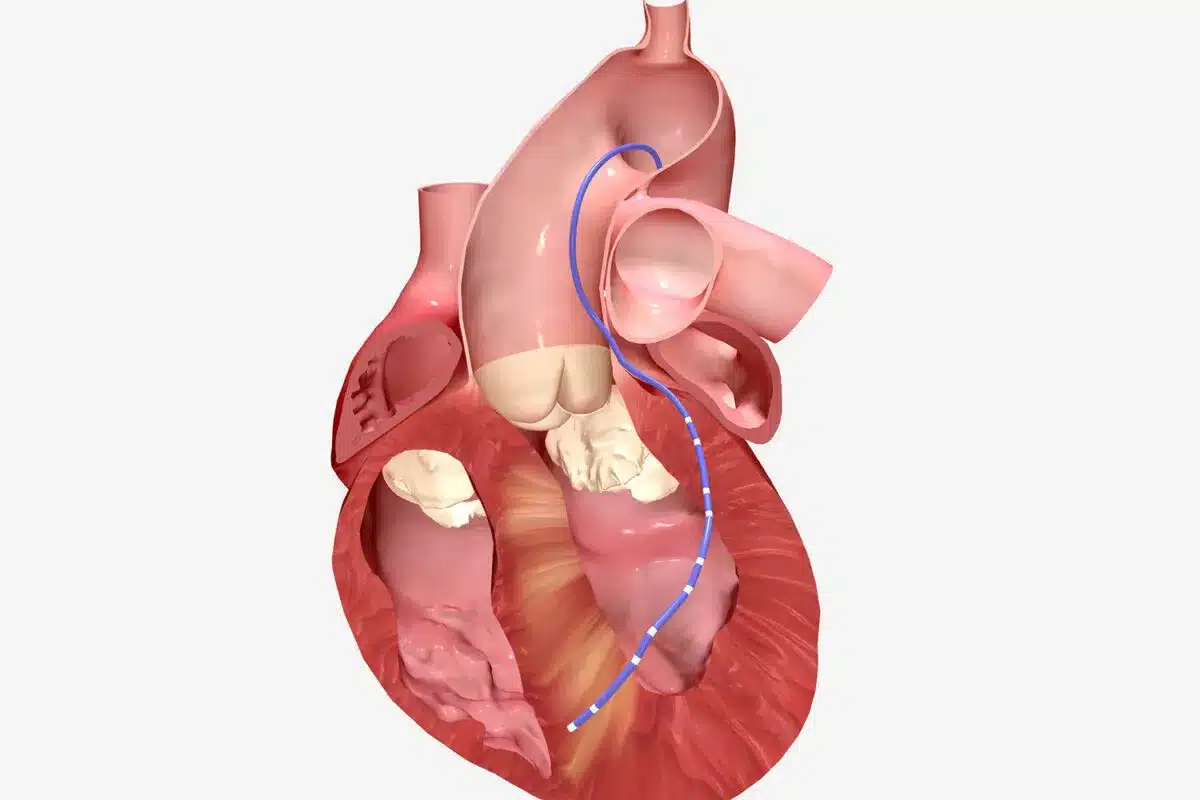
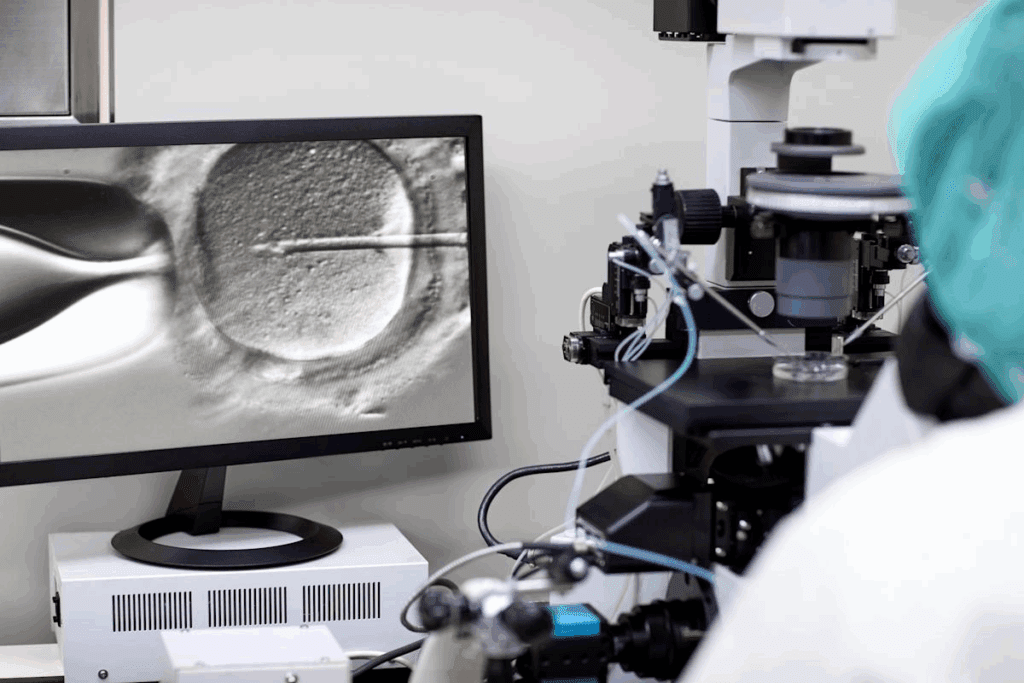
IVF is a type of assisted reproductive technology (ART) where an egg is fertilized with sperm outside the body. It involves several steps, from initial consultation to embryo transfer. IVF has become more common, with thousands of cycles done every year worldwide.
The procedure’s popularity comes from its success in solving fertility issues. This includes blocked fallopian tubes, low sperm count, and unexplained infertility.
The prevalence of IVF is notable, with many fertility clinics reporting successful outcomes. As medical technology advances, IVF success rates keep improving, making it a preferred option for many.
The Basic IVF Process
The IVF process starts with an initial consultation. A fertility specialist assesses the individual’s or couple’s medical history and fertility status. This is followed by ovarian stimulation, where medications are used to stimulate the ovaries to produce multiple eggs. Monitoring is critical during this phase to ensure the eggs are developing properly.
Once the eggs are ready, they are retrieved through a minor surgical procedure. The eggs are then fertilized with sperm in a laboratory. The resulting embryos are cultured for 3-5 days. Then, one or more embryos are transferred to the uterus, and any remaining embryos can be frozen for future use.
Who Typically Seeks IVF Treatment
IVF is typically sought by individuals or couples facing various fertility challenges. This includes those with blocked fallopian tubes, endometriosis, low sperm count, or unexplained infertility. Same-sex couples and single individuals may also opt for IVF as a means to conceive.
The decision to undergo IVF is often made after other fertility treatments have failed. It’s a personal choice that involves careful consideration of the physical, emotional, and financial implications.
Financial Burden: The First Major Disadvantage
IVF comes with a big price tag. The cost can be overwhelming. It’s key for those thinking about IVF to know the financial side before starting.
Average Costs in the United States
In the U.S., IVF costs vary a lot. It depends on where you are, the clinic, and what treatments you need. A single IVF cycle can cost between $12,000 and $15,000.
Medications add to the cost. Some fertility drugs can cost over $3,000 per cycle. So, the total for one cycle, including meds, can be up to $18,000 or more.
Service | Average Cost |
IVF Cycle | $12,000 – $15,000 |
Medications | $1,000 – $3,000 |
Total Cost per Cycle | $13,000 – $18,000 |
Insurance Coverage Limitations
Insurance for IVF varies a lot. Some plans cover parts of fertility treatment, but many have limits or exclusions. This can mean big costs for patients.
A study by the American Society for Reproductive Medicine showed in 2019, about 28% of U.S. insurance plans covered fertility treatments. But, how much they covered varied a lot.
“The lack of full insurance coverage for fertility treatments like IVF is a big hurdle for many wanting to start a family.”
Hidden Costs and Multiple Cycle Requirements
There are extra costs with IVF, like for multiple cycles, tests, and other services. Many need more than one cycle to get pregnant. This increases the total cost a lot.
Hidden costs include:
- Pre-IVF tests and checks
- Freezing and storing embryos
- Testing embryos for genetic issues
- Using donor eggs or sperm
Knowing these extra costs is important for those planning IVF. It helps them budget and prepare financially.
Physical and Emotional Toll on Patients
IVF can deeply affect a person’s health and mood. It’s vital to grasp the full impact it has on those going through it.
Side Effects of Hormonal Medication
Hormonal meds in IVF can cause many side effects. These range from mild to severe. Issues like bloating, mood swings, and tiredness are common. In some cases, these meds can lead to serious problems like Ovarian Hyperstimulation Syndrome (OHSS).
Common side effects of IVF hormonal meds include:
- Bloating and weight gain
- Mood swings and irritability
- Fatigue and sleep disturbances
- Headaches and breast tenderness
Psychological Impact of Treatment
The mental effects of IVF should not be ignored. The journey can be emotionally tough, with highs and lows. This rollercoaster can lead to anxiety and depression for some.
It’s crucial for healthcare providers to offer support and counseling. This helps patients deal with the emotional ups and downs of IVF.
Relationship Strain and Social Challenges
IVF can put a strain on relationships and friendships. The stress and uncertainty of treatment can affect how we connect with others. It can also make people feel like they’re going through it alone.
We believe in the importance of open communication. Couples and individuals should talk openly about their feelings and fears.
Understanding the physical and emotional effects of IVF helps us support patients better. We aim to provide care that covers both the medical and emotional sides of their journey.
Increased Risk of Multiple Pregnancies
IVF treatments can lead to more chances of having twins or more. This is because doctors often transfer more than one embryo at a time. This increases the risk for both the mother and the babies.
Statistics on Multiple Births with IVF
IVF pregnancies are more likely to have multiple births than natural ones. Reports show that IVF pregnancies have a higher rate of twins, triplets, and more. This is because transferring more embryos increases the chances of success.
Key statistics include:
- The rate of twin births with IVF is about 20-30%, compared to 3% in natural conceptions.
- The rate of triplet or higher-order births with IVF is 1-5%, much higher than the less than 0.1% rate in natural conceptions.
Health Risks Associated with Multiple Pregnancies
Multiple pregnancies pose health risks for both mothers and babies. These risks include:
- Premature birth: Multiple gestations are more likely to result in preterm labor, leading to complications for the babies.
- Low birth weight: Babies from multiple pregnancies often have lower birth weights, which can lead to health issues.
- Pregnancy complications: Mothers carrying multiples are at a higher risk for gestational diabetes, hypertension, and other complications.
Financial and Practical Implications of Multiple Births
Having multiple babies comes with significant financial and practical challenges. Raising twins, triplets, or more requires a lot of resources, including:
- Increased medical costs: Multiple pregnancies often lead to higher medical expenses due to more frequent prenatal care and possible complications.
- Practical challenges: Caring for multiple newborns at once can be overwhelming, requiring extra support for childcare and household management.
- Emotional strain: The emotional and psychological impact of managing multiple infants can be significant, affecting family dynamics and parental well-being.
It’s important to understand these risks and implications before considering IVF. Talking to healthcare providers about the number of embryos to transfer is essential for making informed decisions.
Higher Rates of Premature Delivery
Studies show that women who have IVF are more likely to have premature babies than those who conceive naturally. This is a big worry because early birth can harm a baby’s health.
Statistical Evidence from Meta-Analyses
Many meta-analyses have looked into IVF and premature birth. They all agree: IVF babies are more likely to be born early. The risk is 1.54 to 2.20 times higher than for naturally conceived babies.
A big study found that IVF babies are at a higher risk of early birth than naturally conceived ones. This is true for single babies.
Study | Odds Ratio for Preterm Birth | Confidence Interval |
Meta-Analysis 1 | 1.54 | 1.23-1.93 |
Meta-Analysis 2 | 2.20 | 1.85-2.62 |
Short and Long-term Consequences of Premature Birth
Premature birth can cause problems right away and later on. Babies might have trouble breathing, get sick, or need to stay in the hospital longer. They could also face delays in development, learning issues, and higher risks of chronic diseases.
It’s important for women having IVF to know these risks. They should talk to their doctors to keep their pregnancy safe.
Potential Causes for Increased Prematurity Risk
The reasons for higher premature birth risk in IVF pregnancies are complex. Infertility issues, the IVF process, and more multiple births with IVF might play a part. More research is needed to understand this better.
We need to learn more about how IVF affects early birth. We also need to find ways to lower this risk.
Disadvantages of In Vitro Fertilization: Congenital Malformation Risks
IVF might slightly increase the chance of birth defects. This is something to think about for those planning to have a baby. We need to know the risks and what kind of defects are possible.
Overall Risk Increase
IVF babies might face a 33% higher risk of birth defects than naturally conceived ones. This is a big worry for parents thinking about IVF.
Specific Risks: Cardiac, Musculoskeletal, and Genitourinary Malformations
Studies have found specific risks with IVF. There’s a 29% higher risk for heart defects, 35% for muscle and bone issues, and 58% for urinary tract problems.
Type of Malformation | Relative Risk |
Cardiac Malformations | 1.29 |
Musculoskeletal Malformations | 1.35 |
Genitourinary Malformations | 1.58 |
Contributing Factors to Malformation Risk
Several things might make birth defects more likely in IVF babies. These include the reasons for infertility, the parents’ age, and the IVF method used.
Research Limitations and Ongoing Studies
Even though research helps, there are some limits. Different studies and people can make results hard to compare. More studies are needed to understand the risks better.
It’s important to know about IVF risks to make good choices. As research gets better, we can help parents understand the good and bad of IVF.
Pregnancy Complications and Maternal Health Concerns
IVF doesn’t just end with a positive pregnancy test. It comes with its own set of challenges. Women who undergo IVF are at a higher risk of pregnancy complications. These can impact their health and well-being.
Gestational Diabetes Risk
One big concern with IVF pregnancies is the risk of gestational diabetes. Studies show that IVF pregnancies are more likely to develop gestational diabetes. Rates can be as high as 24.5% compared to spontaneous conceptions.
A study in the Journal of Clinical Endocrinology and Metabolism found a higher risk of gestational diabetes in IVF pregnancies. This is due to various factors, including infertility causes and hormonal treatments used in IVF.
“The risk of gestational diabetes is a significant concern for women undergoing IVF treatment, and healthcare providers should closely monitor these patients to mitigate possible complications.”
Hypertensive Disorders During Pregnancy
Hypertensive disorders are more common in IVF pregnancies. These disorders can range from mild hypertension to severe preeclampsia. Preeclampsia is a condition with high blood pressure and damage to organs like the kidneys and liver.
Hypertensive Disorder | IVF Pregnancies | Spontaneous Conceptions |
Mild Hypertension | 15% | 8% |
Preeclampsia | 8% | 4% |
Placental Abnormalities and Other Complications
IVF pregnancies also have a higher risk of placental abnormalities. These include placenta previa and placental abruption. These conditions can lead to serious complications for both the mother and the baby, such as preterm labor and fetal distress.
Other complications in IVF pregnancies include a higher risk of cesarean section, postpartum hemorrhage, and maternal ICU admission. While these are rare, they highlight the need for careful monitoring and management of IVF pregnancies.
Long-term Maternal Health Considerations
The health implications of IVF pregnancies go beyond the pregnancy itself. Women who undergo IVF may face a higher risk of long-term cardiovascular disease and other health issues. It’s important for healthcare providers to consider the long-term health needs of these women.
We recommend that women who have conceived through IVF receive regular follow-up care. This is to monitor their health and address any complications early.
Lower Success Rates for Certain Demographics
IVF success rates vary and depend on factors like age and health conditions. It’s important for those thinking about IVF to understand these factors.
Age-Related Success Decline
Age is a big factor in IVF success. As women get older, their eggs quality and number go down. This makes it harder to get pregnant.
Women under 35 usually have better success rates with IVF, often over 50% per cycle.
To show how age affects IVF success, here’s a table:
Age Group | Average Live Birth Rate per IVF Cycle |
Under 35 | 50% |
35-37 | 40% |
38-40 | 25% |
41-42 | 15% |
43-44 | 5% |
Over 44 | Less than 5% |
Impact of Pre-existing Health Conditions
Health conditions like PCOS, endometriosis, and thyroid issues can also affect IVF success. These conditions can mess with ovulation and egg quality.
Talking to your doctor about your health is key to understanding how it might affect your IVF journey.
Unexplained Infertility Challenges
Those with unexplained infertility face special challenges with IVF. Without knowing the cause, treatments may need to be changed many times. This can lower success chances.
Using advanced tests and custom treatment plans can help these patients more.
Emotional Impact of Failed Cycles
Failed IVF cycles can really take a toll on emotions. Patients often feel sad, frustrated, and disappointed.
Getting support from doctors, counselors, and support groups is very important. It helps patients deal with these tough feelings.
Ethical and Religious Considerations
IVF technology raises complex ethical questions. These questions affect individuals, families, and society. It’s important to think about the ethical, religious, and societal impacts of IVF.
Embryo Creation and Disposition Concerns
Creating and dealing with embryos is a big ethical issue in IVF. Often, IVF makes multiple embryos, leading to tough decisions. Decisions on embryo disposal, donation, or storage are emotionally and ethically complex. These decisions touch on deep beliefs about life and personhood.
Religious Perspectives on IVF
Religions have different views on IVF. Some see it as a way to fulfill the command to be fruitful and multiply. Others object to the separation of reproduction from marriage. Understanding these diverse perspectives is key for those considering IVF.
Societal and Legal Implications
IVF has legal and societal implications. Laws on IVF vary, affecting access and rights. Societal attitudes towards IVF also matter, influencing support and resources. We need to see how IVF fits into society and how it’s regulated.
Looking at these ethical, religious, and societal aspects helps us understand IVF better. This deeper understanding is vital for making informed choices and shaping policies and practices around IVF.
Balancing Risks and Benefits: Making Informed Decisions
When thinking about IVF, it’s key to look at both the good and the bad sides. IVF can be a big help for many people trying to have a baby. But, it’s important to think about health, feelings, and money too.
When IVF May Be Worth the Risks
For some, the good things about IVF are more important than the bad. This is true for those who have tried other ways to have a baby or have health issues that IVF can help with. “Choosing IVF should be based on a deep look at your own situation,” says Medical Expert, a fertility expert.
Some reasons IVF might be a good choice include:
- Having a known fertility problem that IVF can fix
- Not getting pregnant with other treatments before
- Feeling strongly about trying every option
Alternative Fertility Options
IVF is not the only way to try to have a baby. Other options are:
- Intrauterine Insemination (IUI)
- Medicine to help with ovulation
- Surgery to fix fertility problems
Looking at these other choices can help you understand your options better. This way, you can make a choice that feels right for you.
Questions to Ask Your Healthcare Provider
Deciding on IVF means asking the right questions to your doctor. Some important questions to ask include:
- What are the risks and benefits of IVF for me?
- What are my chances of getting pregnant with IVF, and what affects this?
- Are there other treatments that might be better for me?
- What will it cost, and will my insurance cover it?
Support Resources for Decision-Making
Choosing to do IVF can be tough, both in your head and in reality. Luckily, there are many places to get help, like:
- Fertility support groups, online or in-person
- Counseling for fertility issues
- Info and resources from trusted fertility groups
Using these resources and talking openly with your doctor can help you make a better choice. This way, you can move forward on your path to having a family.
By doing this, you can work towards creating the family you’ve always wanted.
Conclusion: Navigating the IVF Journey
In vitro fertilization (IVF) is a common way to have a baby, used in about 1 to 3 percent of births in rich countries. Understanding the ups and downs of IVF is key as we go through this journey.
IVF gives hope to many who want to have children. It has its good points and tough spots. Knowing the downsides, like the cost, physical and emotional strain, and higher risks of pregnancy problems, helps people make smart choices about their fertility.
As we wrap up our look at IVF, we stress the need to weigh the pros and cons. This way, people can move forward with confidence, knowing all about this fertility help.
FAQ
What are the main disadvantages of IVF?
IVF can be very expensive. It also takes a toll on your body and mind. There’s a higher chance of having twins or more, which can lead to health issues for the baby.
It may also cause early birth and birth defects. Success rates can be lower for some people.
How much does IVF typically cost in the United States?
IVF costs in the U.S. vary a lot. It can be between $12,000 to $15,000 per try. You also have to add costs for medicines and tests.
Does insurance typically cover IVF?
Insurance for IVF varies a lot. Some plans help pay for it, but others don’t. This can leave you with big bills.
What are the physical side effects of IVF treatment?
IVF can make you feel bloated and moody. You might also feel really tired. This is because of the hormones used to help grow eggs.
How does IVF affect mental health?
IVF can really affect your mind. It can cause stress, anxiety, and even depression. This is more common if you need to try many times or if it doesn’t work.
What is the risk of multiple pregnancies with IVF?
IVF increases the risk of having twins or more. About 40% of IVF babies are born in multiple births. This is much higher than the 3% rate in regular pregnancies.
Are IVF pregnancies associated with higher risks of complications?
Yes, IVF pregnancies have a higher risk of problems. This includes gestational diabetes, high blood pressure, and issues with the placenta. There’s also a higher chance of early birth.
Does IVF increase the risk of congenital malformations?
Research shows IVF might slightly increase the risk of birth defects. This includes heart, muscle, and urinary tract issues.
How does age affect IVF success rates?
Age is very important for IVF success. Women under 35 have better chances. But, women over 40 face much lower success rates because egg quality drops with age.
What are the ethical considerations surrounding IVF?
IVF raises many ethical questions. This includes how to handle embryos and what religions think about it. These issues can affect people’s choices.
Are there alternative fertility options to IVF?
Yes, there are other ways to try to have a baby. This includes IUI, ovulation induction, and surrogacy. These might be better for some people or couples.
What questions should I ask my healthcare provider about IVF?
When thinking about IVF, ask your doctor about risks and benefits. Also, ask about success rates, costs, and other options. Find out what to expect during treatment.
What are the benefits of assisted reproductive technology like IVF?
IVF and other assisted reproductive technologies offer hope. They help people and couples who are struggling to have a baby. They provide a way to build a family despite reproductive challenges.
What are the cons of in vitro fertilization?
The downsides of IVF include the cost, physical and emotional strain, and higher risks of multiple births. There’s also a higher chance of premature birth, birth defects, and pregnancy complications.
Are there any long-term health considerations for IVF mothers?
Yes, IVF mothers might face long-term health issues. This includes a higher risk of heart disease. This could be due to the reasons for infertility or the IVF process itself.
References
- Tocariu, R., et al. (2022). Incidence of complications among in vitro fertilization pregnancies: hypertension, gestational diabetes, prematurity. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC10165528/