In vitro fertilization (IVF) is a complex process. It creates multiple embryos to boost the chances of a successful pregnancy. But, not all embryos are used in the treatment. Understanding the options and the complex decisions faced when you choose to discard embryos.
Every year, about 1.5 to 1.9 million embryos from IVF don’t lead to live births. This brings up big questions about their fate. It includes embryo disposal and the choices couples face with unused embryos.
At Liv Hospital, we get how tough these decisions are. We offer caring, clear care to help patients through these tough choices.
Key Takeaways
- IVF involves creating multiple embryos to maximize pregnancy chances.
- Not all embryos created during IVF are used.
- The fate of unused embryos is a significant decision for couples.
- Liv Hospital provides expert care and support for IVF patients.
- Understanding embryo disposal options is key for making informed decisions.
The IVF Process and Why Multiple Embryos Are Created
Understanding IVF is key. It creates many embryos to boost pregnancy chances. The IVF journey is detailed and includes several important steps.
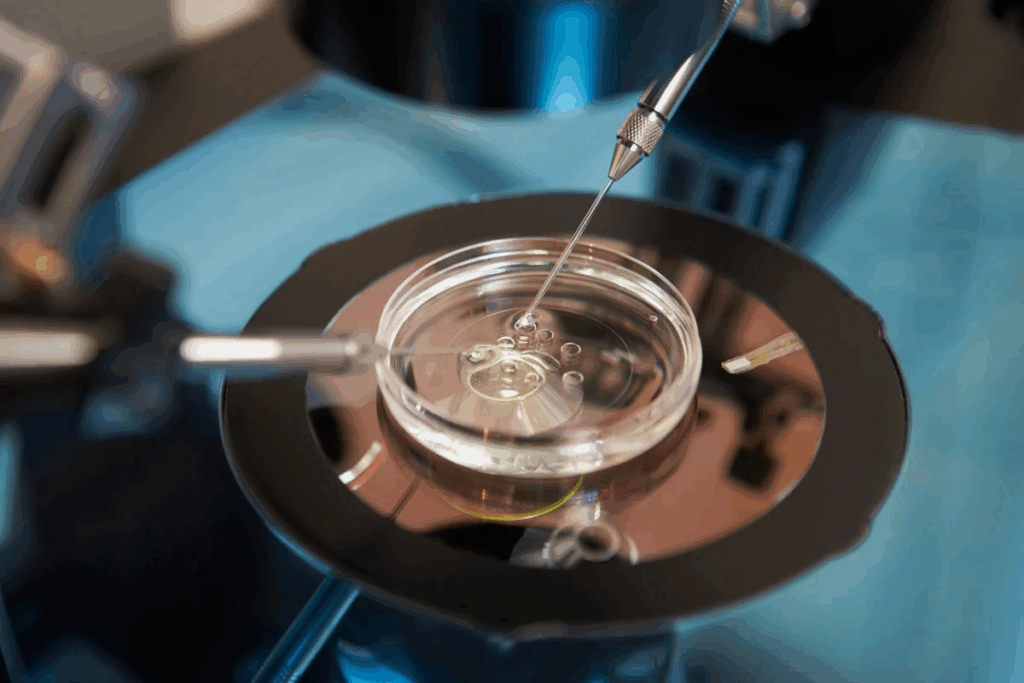
Ovarian Stimulation and Egg Retrieval
The first step is ovarian stimulation. Medications are used to make the ovaries produce many eggs. This step increases the chance of getting healthy eggs for fertilization.
Medical Expert, a fertility specialist, notes, “Ovarian stimulation is a key step. It lets us get multiple eggs, raising the chance for successful fertilization and embryo growth.”1 After stimulation, egg retrieval is done. This is usually under sedation.
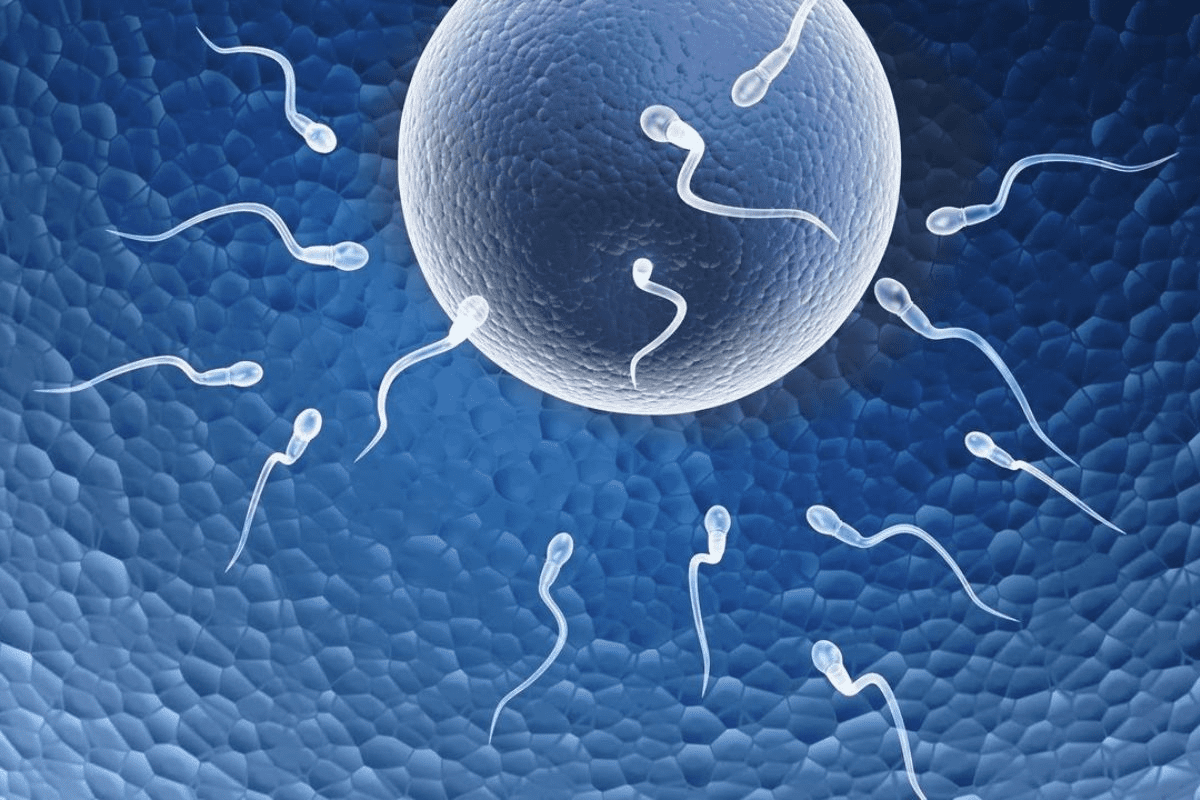
Fertilization and Embryo Development
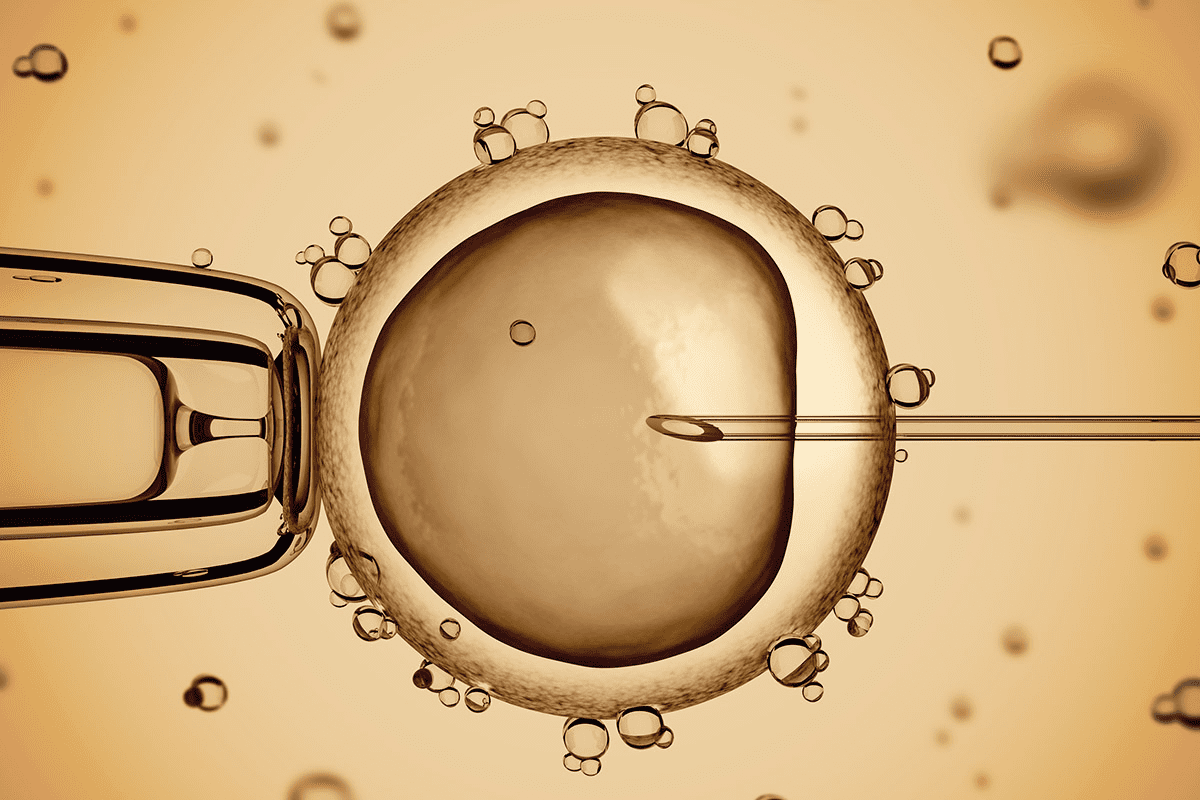
After egg retrieval, eggs are fertilized with sperm in the lab. This is called insemination or intracytoplasmic sperm injection (ICSI).
The embryos then grow for 3-5 days. Embryologists watch their development, checking their quality and health.
“Growing embryos in the lab is a precise and careful process,” says Medical Expert, an embryologist. “We watch each embryo’s growth to pick the best ones for transfer.”
The Purpose of Creating Extra Embryos
Making many embryos is a key part of IVF. The main goal is to increase the chance of a successful pregnancy.
Having many embryos lets doctors choose the healthiest ones for transfer. This boosts the chance of a successful outcome.
As noted by the ‘Society for Assisted Reproductive Technology, making many embryos is standard in IVF. It increases pregnancy chances while reducing the need for more cycles.’
Extra embryos can also be frozen for later use. This gives patients another chance at pregnancy without starting a new IVF cycle.
We know IVF is tough physically and emotionally. But making many embryos greatly improves pregnancy chances. This makes the journey worth it for many.
Statistics on Unused Embryos in IVF Treatment
The IVF industry faces a big challenge with unused embryos. This raises questions about their fate. Looking into IVF treatment statistics shows the problem of unused embryos is big.
1.5-1.9 Million Embryos Never Born Annually
About 1.5 to 1.9 million embryos from IVF are never born each year. This huge number shows how much embryo wastage there is in fertility treatments. Many factors contribute to this, like the number of embryos created and the choice of which to implant.
80.2% Embryo Wastage Rate in Fresh Cycles (2004-2013)
Studies found an embryo wastage rate of 80.2% in fresh non-donor cycles from 2004 to 2013 in the U.S. This high rate shows how complex and inefficient IVF can be. It’s due to embryo quality and implantation success rates.
Average Yield and Discard Rate Per IVF Cycle
The number of embryos created and discarded in IVF cycles varies a lot. IVF tries to make many embryos to boost pregnancy chances. But not all are good or chosen for transfer. So, many are thrown away, adding to the unused embryo statistics.
It’s key for patients and doctors to understand these numbers. By looking at data on unused embryos, we can see the big picture of IVF. We also see the ethical issues of embryo disposal.
Why Embryos Are Not Used in IVF Procedures
When it comes to IVF, the decision on what to do with embryos is complex. It depends on how well the embryos are doing and what the patient needs. Several things influence this choice.
Quality and Viability Assessments
One big reason is the quality and health of the embryos. Doctors check how the embryos look, grow, and are doing overall. If an embryo doesn’t meet certain standards, it might not be good for transfer.
Genetic Testing Results
Genetic tests are also key. These tests look for any big problems in the embryos. This helps pick the healthiest one for implantation.
These test results are very important. Preimplantation genetic testing (PGT) finds genetic issues in embryos before they’re put in the uterus.
Family Size Completion
Some people might not use their embryos if they’ve already had the family size they want. This choice is personal and varies a lot.
Financial Constraints for Continued Treatment
Money is another big factor. IVF is expensive, and keeping embryos frozen adds to the cost. Some might stop treatment because of the money.
Let’s look at some stats on why embryos aren’t used:
Reason for Not Using Embryos | Percentage |
Poor Embryo Quality | 40% |
Genetic Abnormalities | 25% |
Completed Family Size | 20% |
Financial Constraints | 15% |
The table shows that poor embryo quality is the main reason. But other factors like genetic issues, family size, and money also play a part.
Knowing these reasons helps patients make better choices about their IVF treatment and what to do with unused embryos.
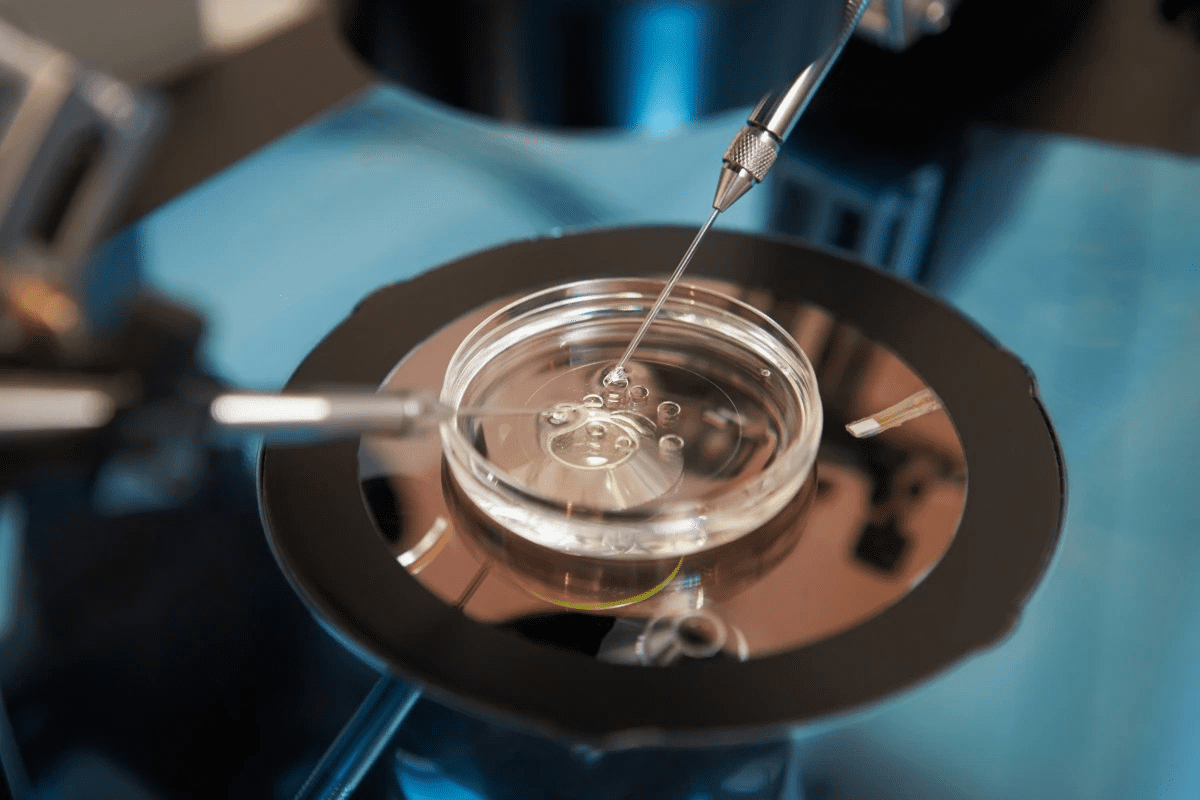
Cryopreservation: The Process of Freezing and Storing Embryos
Embryo cryopreservation has changed IVF forever. It lets embryos be frozen and used later. This has greatly increased the success of IVF.
Vitrification Techniques
Vitrification quickly freezes embryos to keep them safe. It stops ice crystals from forming, which can harm cells. This method uses special chemicals and quick freezing with liquid nitrogen.
Key benefits of vitrification include:
- High survival rates of embryos post-thawing
- Reduced risk of ice crystal damage
- Improved pregnancy rates with frozen embryos
Success Rates with Frozen Embryos
Thanks to better vitrification, frozen embryos work just as well as fresh ones. Some clinics even see better results with frozen embryos. This means patients can try again without needing more egg retrieval and fertilization.
The advantages of using frozen embryos include:
- Reduced risk of ovarian hyperstimulation syndrome (OHSS)
- Improved endometrial receptivity
- Flexibility in planning transfer cycles
Duration and Limitations of Storage
How long embryos can be stored varies by clinic and law. Usually, it’s up to 10 years, but some places offer longer. Storage is limited by laws, ethics, and patient consent renewal.
Factors influencing storage duration include:
- Legal regulations governing embryo storage
- Clinic policies on storage limits
- Patient preferences and consent
The Current State of Frozen Embryo Storage in the US
More IVF procedures have led to a big jump in frozen embryo storage. Now, there are about 1.4 million embryos in the US. This number shows the big challenge in managing, storing, and deciding what to do with these embryos.
1.4 Million Frozen Embryos in Storage
The number of frozen embryos in the US shows how far IVF technology has come. 1.4 million embryos mean a big investment of emotions, money, and medical effort for those involved.
Storage Costs and Financial Burden
One big problem with frozen embryo storage is the cost. Storage fees can change a lot based on where you are and what you get. This can be very expensive for people trying to have a baby.
The Growing Challenge of Long-Term Storage
With more embryos being stored, managing them for a long time gets harder. Clinics and storage places have to deal with keeping a lot of embryos safe. They also have to think about how to store them well and handle the ethics of keeping them for a long time.
Thinking about long-term storage and what to do with embryos is key. Options include donating, keeping them stored, or getting rid of them. As fertility treatments change, we need to tackle the tough issues of frozen embryo storage.
The Problem of Abandoned Embryos
IVF clinics are dealing with a growing problem. Many embryos are left unclaimed by patients. This has raised concerns among fertility experts and questions about what to do with unused embryos.
Nationwide Abandonment Rates
Research shows that 5-7% of embryos are abandoned nationwide. This means thousands of embryos are left unclaimed in the U.S. each year.
Clinic Reports on Abandonment
Some clinics report even higher rates, up to 18%. These numbers show the complexity of the issue. They highlight the need for a deeper understanding of the factors involved.
There are many reasons for these high rates. Some include:
- Changes in personal circumstances or family planning goals
- Financial constraints that prevent patients from continuing their IVF treatment
- Emotional or psychological factors that lead patients to disengage from the IVF process
- Loss of contact due to relocation or changes in communication details
Reasons Patients Lose Contact with Clinics
Patients lose contact for various reasons. These include:
- Relocation to a different city or country without updating their contact information
- Changes in personal circumstances, such as divorce or separation, that affect their IVF plans
- Financial difficulties that lead to a discontinuation of IVF treatment
- Achieving their desired family size and not needing the remaining embryos
The issue of abandoned embryos shows the need for better support during IVF. By understanding why embryos are abandoned, clinics can help their patients. This addresses the ethical and emotional challenges of IVF treatment.
Patient Options for Unused Embryos
The journey of IVF doesn’t end with the creation of embryos. Patients must then decide what to do with those that remain unused. This decision is both personal and complex, involving ethical, emotional, and practical considerations.
Continued Storage
One option for patients is to continue storing their unused embryos. This can be done on an indefinite or time-limited basis. Continued storage allows patients to keep their options open, potentially for future use in another IVF cycle.
It also means ongoing storage costs and the need to periodically review their decision.
Storage costs can be a significant factor, varying by clinic and location. Patients must weigh these costs against the benefits of keeping their embryos frozen.
Donation to Other Couples
Another option is donating unused embryos to other couples or individuals struggling with infertility. This process is often referred to as “embryo adoption.” It allows patients to give the gift of life to others while also bringing closure to their own reproductive journey.
Donation involves several steps, including matching with recipient couples and legal agreements. It’s a generous act that can be emotionally rewarding for all parties involved.
Donation for Scientific Research
Patients may also choose to donate their unused embryos for scientific research. This can contribute to advancements in reproductive medicine, genetics, and our understanding of early human development.
Donation for research is typically done with informed consent and under strict regulatory guidelines. It provides an opportunity for patients to contribute to the greater good of medical science.
Compassionate Transfer
For some patients, a compassionate transfer might be an option. This involves transferring the embryos at a time when pregnancy is less likely, avoiding the emotional and physical process of a failed cycle.
This option is less commonly discussed but can be a compassionate way to conclude the IVF process. It avoids the distress of a failed implantation.
How Clinics Discard Embryos: Methods and Protocols
Clinics have strict rules for getting rid of embryos. They make sure the process is respectful and follows the rules. This is because handling embryos is very sensitive.
39% Direct Disposal in Fresh Cycles
About 39% of embryos are thrown away right away in fresh cycles. This means embryos that can’t be used or frozen are disposed of immediately.
36.7% Direct Disposal in Frozen Cycles
In frozen cycles, around 36.7% of embryos are also thrown away right away. This is for frozen embryos that are not needed or can’t be used anymore.
Thawing Procedures Prior to Disposal
Frozen embryos are thawed before they’re thrown away. This thawing is important for safe disposal. It helps prevent any risks.
Documentation and Witnessing Requirements
Clinics must keep detailed records and have witnesses during embryo disposal. This makes the process clear, accountable, and respectful to the embryos.
Getting rid of embryos is a complex task. It’s not just about throwing them away. Clinics must also think about ethics and rules. They need to balance disposing of embryos with respect and care.
Key aspects of embryo disposal protocols include:
- Strict adherence to regulatory guidelines
- Careful documentation of the disposal process
- Witnessing requirements to ensure accountability
- Respectful handling of embryos during disposal
By sticking to these rules, clinics can make sure embryo disposal is both respectful and follows the law.
Patient Decision-Making: Statistics and Factors
IVF patients face a tough choice about what to do with extra embryos. This choice is shaped by many things. These include personal beliefs, medical advice, and ethical thoughts.
Statistics on Patient Choices
Recent studies have shown how IVF patients decide about their unused embryos. About 50.6% choose to discard them. On the other hand, 45.4% decide to donate. These numbers show the different ways patients make this tough decision.
Decision | Percentage |
Discard Embryos | 50.6% |
Donate Embryos | 45.4% |
Factors Influencing Patient Decisions
Choosing to discard or donate embryos is a big decision. Many things affect this choice. These include the embryos’ quality, genetic test results, and if the family is complete. Money issues and the emotional impact of storage or disposal also matter a lot.
Can an embryo stop growing after implantation? This is a common question. While the main focus is on what to do with unused embryos, knowing about growth is key. The embryo’s quality and the environment in the uterus can affect its growth.
Psychological Impact of Disposal Decisions
The emotional impact of deciding on unused embryos is huge. Patients feel a lot of stress, whether they choose to discard or donate. It’s important for clinics to offer support and resources. This helps patients deal with these complex choices.
Resources for Making Informed Choices
Clinics and healthcare providers are key in supporting patients. They should give detailed counseling and info on options. This helps patients make choices that fit their values and situation.
Legal Framework Governing Discarded Embryos
It’s important to know the laws about discarded embryos for patients and doctors in IVF. The rules are complex and depend on state laws and ethical rules.
State-by-State Variations in the US
In the US, laws about throwing away embryos differ a lot from state to state. Some states have clear laws about it, while others use court decisions or agreements between patients and clinics.
State | Specific Statute on Embryo Disposition | Case Law Influence |
California | No | Yes |
New York | Yes | No |
Texas | Yes | Yes |
Consent Requirements and Documentation
Getting consent is key in the laws about embryo disposal. Clinics ask patients to sign forms about what to do with their embryos. These forms are important and tell clinics what to do if embryos are thrown away.
Ownership and Disposition Rights
Who owns the embryos and can decide what to do with them is a big debate. Courts look at contracts and state laws to figure out who has the right to decide.
Recent Legal Developments and Court Cases
New court cases are changing the laws about embryo disposal. For example, cases about what to do with embryos in divorce have led to important legal decisions.
Knowing these legal points helps patients and doctors understand IVF better. It helps them make good choices about what to do with embryos.
Ethical Considerations Around Embryo Disposal
The topic of embryo disposal is complex, with many views from religious, secular, and medical groups. As more people use IVF, the debate over what to do with embryos grows. We need to understand these different views carefully and with respect.
Religious Perspectives on Embryo Status
Religious groups have different beliefs about when life starts and the value of embryos. Some think life begins at conception, giving embryos full moral value. Others see embryos as having moral value, but not absolute. It’s important to know these beliefs to respect those going through IVF.
Secular Views on Moral Status of Embryos
Secular views also vary on embryo morality. Some say embryos have inherent value because they could become humans. Others believe their value depends on if they can feel or experience. These views often focus on dignity and personal choice in reproductive matters.
Balancing Reproductive Autonomy and Ethical Concerns
It’s hard to balance personal reproductive rights with broader ethical issues. People have the right to decide about their embryos from IVF. Yet, there are big ethical questions about embryos and what happens to them. We must respect personal choices while considering these ethics.
Perspectives from Bioethicists and Medical Professionals
Bioethicists and doctors add important insights to the embryo disposal debate. They stress the need for informed consent and clear rules for embryo handling. Their knowledge helps us understand the complex mix of personal rights, ethics, and embryo value.
Conclusion: The Future of Embryo Management in IVF
IVF technology keeps getting better, and managing embryos is key. We’ve looked at the challenges of making, storing, and getting rid of embryos. It’s clear we need to make informed choices and care for each other.
New IVF methods will shape how we manage embryos. Better freezing and genetic tests could make IVF more successful. This might mean fewer embryos are left unused.
It’s important to focus on the person, not just the technology. We need to give people the help and support they need. This way, we can handle the tough parts of IVF better and help more people.
We must keep talking about the big questions around embryo management. This includes the ethics, laws, and social issues. We need to make sure IVF stays in line with what people value and need today.
FAQ
What happens to embryos that are not used in IVF?
Unused embryos can be frozen for later use, donated to other couples, or used for research. The choice depends on personal beliefs, family size, and financial status.
How are IVF embryos discarded?
Embryos are thawed before being discarded. Clinics follow strict rules to handle and dispose of them respectfully, based on local laws.
How many embryos are destroyed in IVF each year?
About 1.5 to 1.9 million embryos are not born each year. This shows a large number of embryos not used in IVF.
What is the rate of embryo wastage in IVF?
Studies found an 80.2% embryo wastage rate in fresh cycles from 2004-2013. This indicates many embryos are not used.
Can an embryo stop growing after implantation?
Yes, embryos can stop growing after implantation. This can happen due to chromosomal issues or other viability problems.
How are frozen embryos destroyed?
Frozen embryos are thawed before disposal. Once thawed, they are non-viable and disposed of according to clinic rules.
Are embryos fertilized in IVF?
Yes, in IVF, eggs are fertilized with sperm in a lab. This creates embryos.
How many frozen embryos are there in the US?
There are about 1.4 million frozen embryos in the US. This poses a challenge for long-term storage and management.
Why do embryos stop developing after day 3?
Embryos may stop developing for many reasons. These include chromosomal issues, poor culture conditions, or other viability problems.
What are the options for managing unused embryos?
Unused embryos can be stored, donated to other couples, donated for research, or transferred compassionately.
What are the ethical considerations surrounding embryo disposal?
Embryo disposal raises ethical questions. Views vary from religious to secular and bioethical. It’s important to balance personal rights with ethical concerns.
What is the legal framework governing discarded embryos?
Laws on discarded embryos vary by state in the US. There are differences in consent, ownership, and disposition rights. Legal developments and court cases are shaping the rules.
How do clinics handle abandoned embryos?
Clinics face challenges with abandoned embryos. Abandonment rates range from 5-7% nationwide, and up to 18% in some clinics. Reasons include loss of contact and financial issues.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9975076/