Understanding the journey of IVF treatment is key for those planning their fertility. It’s important to know how many fertilized eggs turn into blastocysts.do all fertilized eggs become embryosWhere do embryonic stem cells come from?
Generally, 40% to 60% of fertilized eggs become blastocysts. But, this can change based on several things. These include the woman’s age, egg and sperm quality, and the clinic’s techniques.
At places like Liv Hospital, we use the latest science and care for each patient. We focus on improving blastocyst success. We watch the IVF fertilization rate and IVF attrition rate closely to give the best care.
Key Takeaways
- The percentage of fertilized eggs that make it to blastocyst stage varies between 40% and 60%.
- Factors such as age, egg and sperm quality, and clinic techniques influence IVF success rates.
- Modern fertility clinics use advanced technology and personalized care to optimize blastocyst outcomes.
- Understanding IVF fertilization and attrition rates is key for managing expectations.
- Quality embryo development directly impacts pregnancy success.
The Embryo Development Process in IVF
The IVF process starts with egg retrieval, then moves to fertilization, and ends with embryo culturing. Knowing each step is key for those going through fertility treatments.
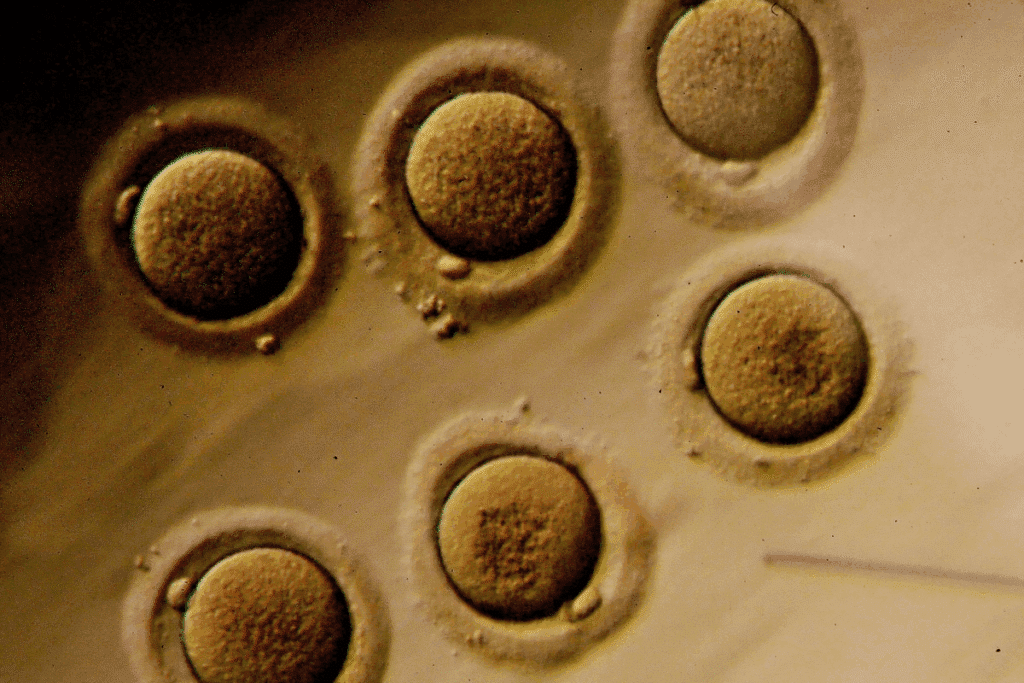
From Egg Retrieval to Fertilization
Egg retrieval is the first step in IVF. Eggs are taken from the ovaries and fertilized with sperm in a lab. This is called insemination.
It can be done through conventional IVF or ICSI, where one sperm is injected into the egg.
Fertilization happens 12-24 hours after egg retrieval. The embryos then grow in a special medium.
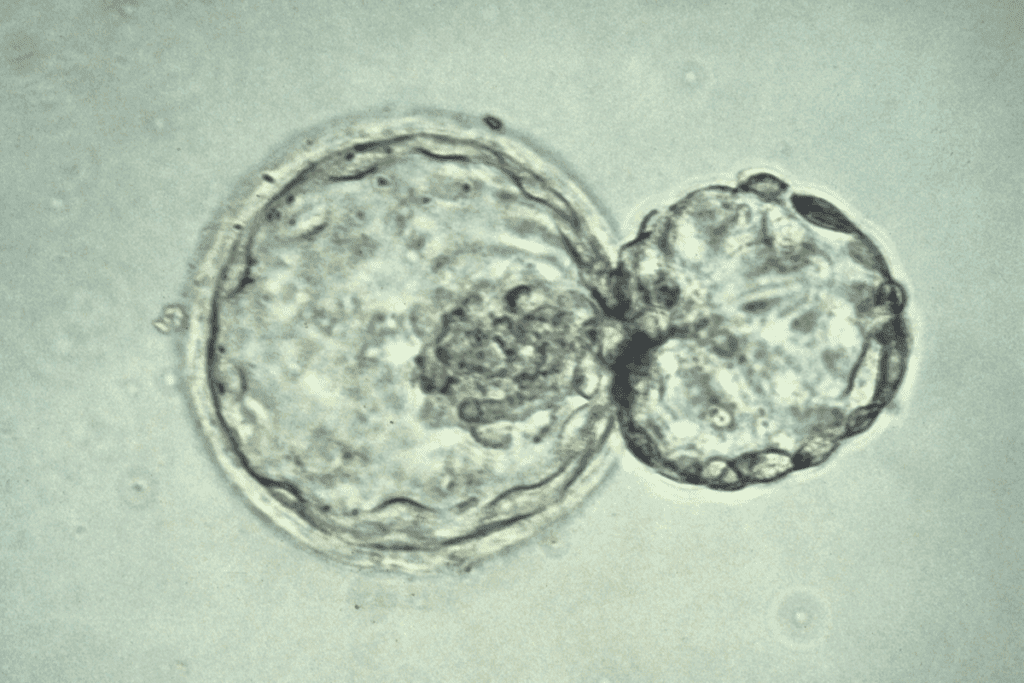
Early Embryo Development Stages
After fertilization, embryos start dividing. On Day 1, they are at the pronuclear stage. By Day 2 and Day 3, they have more cells.
The quality of embryos is checked by their cell count, fragmentation, and symmetry.
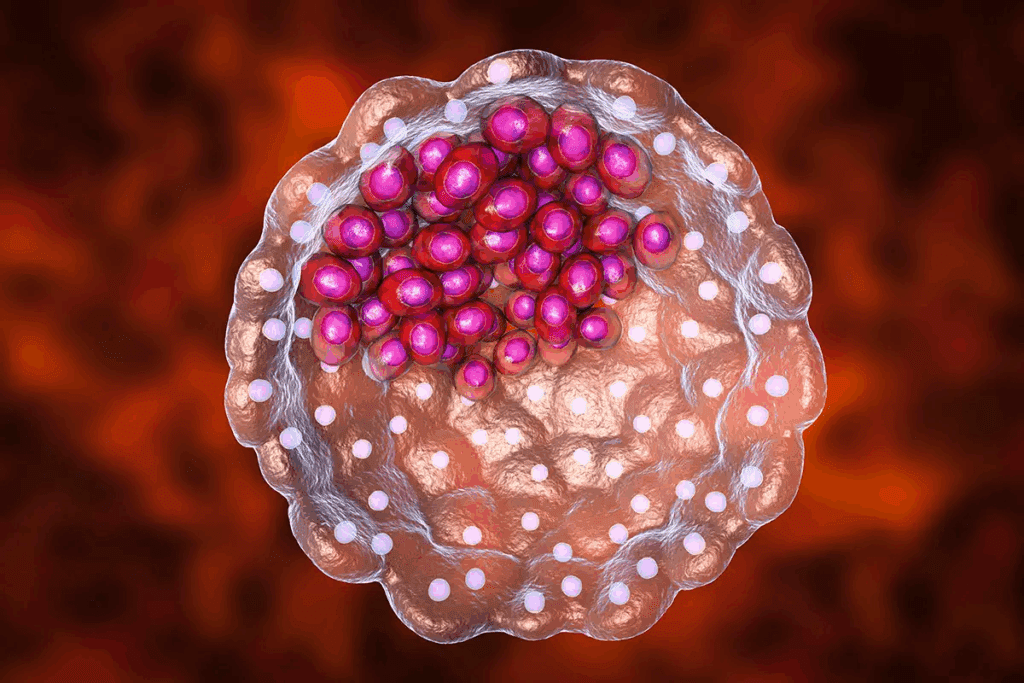
Reaching the Critical Blastocyst Stage
By Day 5, embryos become blastocysts. A blastocyst has a fluid-filled cavity and an inner cell mass. This is a key stage in development.
Not all embryos reach this stage. The blastocyst formation rate shows how successful IVF can be.
Knowing about embryo development helps patients understand the IVF process better.
IVF Fertilization Rate: What to Expect
Knowing the IVF fertilization rate is key for those starting their fertility journey. This rate shows how likely IVF treatment will succeed. We’ll look at average success rates, what affects fertilization, and what’s considered normal or abnormal.
Average Fertilization Success Percentages
The average fertilization rate for IVF is about 80% for mature eggs. This means 8 out of 10 mature eggs might fertilize successfully. But, this number can change based on egg and sperm quality and fertilization method.
Here are some stats to help you understand better:
Category | Average Fertilization Rate |
Mature Eggs | 80% |
Immature Eggs | Lower than 80% |
Eggs with Abnormalities | Significantly Lower than 80% |
Factors Influencing Initial Fertilization
Many things can affect the initial fertilization rate in IVF. These include:
- Egg quality and maturity
- Sperm quality and motility
- The fertilization method (conventional IVF vs. ICSI)
- Patient age and overall health
Normal vs. Abnormal Fertilization Patterns
Normal fertilization shows two pronuclei (2PN) after fertilization. Abnormal patterns, like 0PN, 1PN, or 3PN, can happen due to egg or sperm issues.
Not all fertilized eggs become viable embryos. Clinics watch embryo development closely to find the best ones for implantation.
By understanding the IVF fertilization rate and its factors, patients can better plan their fertility journey. This helps them make informed treatment choices.
Day 1 to Day 5 Embryo Survival Rate
The first five days are key for embryo growth in IVF. During this time, embryos grow and change a lot. Not all make it to the blastocyst stage.
About 50-70% of embryos don’t reach the blastocyst stage. This is called embryo attrition. It happens in the lab and is affected by many things, like embryo quality and lab conditions.
Understanding Embryo Attrition
Embryo attrition means some embryos stop growing in the lab. It’s a big part of IVF that patients should know about. Attrition can happen for many reasons, like genetic problems or lab issues.
Medical Expert, a fertility expert, says,
“Embryo attrition is a natural process, but it’s essential for patients to understand that it’s not a reflection of the quality of care provided by the fertility clinic.”
Why Some Embryos Stop Developing
Many things can cause embryo attrition. These include:
- Genetic problems in the embryo
- Not ideal lab conditions
- Problems with the culture medium
- Older age and egg quality of the mother
The table below shows the average survival rates of embryos from day 1 to day 5:
Day | Average Survival Rate |
Day 1 | 100% |
Day 3 | 70-80% |
Day 5 | 30-50% |
The Natural Selection Process in the Lab
The lab environment is very important for embryo growth. Embryologists try to mimic natural conditions. But, some embryos may not do well for various reasons.
Knowing the survival rate from day 1 to day 5 is key for IVF treatment. Attrition is natural, but lab improvements help more embryos develop successfully.
What Percent of Fertilized Eggs Make It to Blastocyst?
Knowing how many fertilized eggs turn into blastocysts is key for IVF patients. The path from fertilization to blastocyst is full of challenges and many factors play a role.
Current Success Rate Statistics
Recent studies show a big jump in blastocyst formation rates thanks to new IVF tech and lab practices. Now, 40-60% of fertilized eggs reach the blastocyst stage. This change is because of things like patient age, egg quality, and the IVF methods used.
Thanks to better culture media, advanced incubators, and improved embryo picking, IVF success has gone up. These steps have made IVF treatments more effective.
Historical Improvement in Blastocyst Formation
In the last 20 years, the rate of blastocyst formation has gone up a lot. Back then, it was only 30-40%. This boost is thanks to better lab tools and techniques, like time-lapse imaging and advanced culture media.
Thanks to ongoing work by doctors, scientists, and embryologists, IVF success rates keep getting better. Their teamwork has led to these improvements.
Comparing Clinic Success Rates
It’s important to remember that blastocyst formation rates differ between IVF clinics. Things like the skill of the embryology team, the quality of lab gear, and the IVF methods used all play a part.
When looking at clinic success rates, consider these points:
- What IVF protocols and technologies each clinic uses
- The experience and skills of the embryology team
- Success rates for different age groups
By knowing these details, patients can make better choices about their IVF treatment.
Starting with 4 Fertilized Eggs Day 1: Expected Outcomes
The journey of IVF starts with fertilization. For those with 4 fertilized eggs on day 1, knowing what to expect is key. This is a critical time, filled with hope and many questions.
Typical Development Trajectory
Starting with 4 fertilized eggs on day 1 is a big moment. The first few days are vital for embryo growth. By day 3, they should be at the cleavage stage.
By day 5, some may become blastocysts, a major step in IVF.
About 30-50% of fertilized eggs become blastocysts by day 5. So, from 4 eggs, patients might see 1-2 become blastocysts.
Statistical Probabilities for Blastocyst Formation
The chance of blastocyst formation varies. It depends on egg and sperm quality, and the lab’s skill. While averages help, results can vary a lot.
IVF is very personal. Age, medical history, and treatment plans all play a role in success rates.
Managing Expectations with a Small Cohort
It’s important to manage your hopes when starting IVF with just a few eggs. Success rates give a general idea, but be ready for anything. Talk to your fertility specialist to understand your chances better.
Some might not get any blastocysts, but this is rare. Others might get more than expected. Stay open to any outcome.
How Many Embryos Make It to Day 5?
Figuring out how many embryos make it to day 5 is key in IVF. This stage is important because it shows if an embryo can implant and lead to pregnancy. The journey from day 1 to day 5 is full of complex developmental stages.
Average Blastocyst Formation Rates
Research shows that about 40-60% of fertilized eggs become blastocysts by day 5. This means half of the eggs might develop into blastocysts. But, this number can change based on egg and sperm quality and the IVF method used.
Patients want to know their chances of success. Knowing the average blastocyst formation rates helps set realistic hopes.
The Critical Day 3 to Day 5 Transition
The move from day 3 to day 5 is very important in embryo growth. During this time, embryos go through many changes. By day 3, they are at the cleavage stage, and by day 5, they should be blastocysts.
This stage is key because it’s when we check if an embryo can implant. Not all embryos make it through this stage. Many things can affect their growth.
Quality Grading of Day 5 Blastocysts
By day 5, we grade the blastocysts’ quality. We look at size, cell count, and the health of the inner cell mass and trophectoderm. This helps pick the best embryos for transfer.
Top-quality blastocysts have a higher chance of implanting and leading to pregnancy. Our fertility experts carefully check each blastocyst to decide the best plan for each patient.
From 8 Eggs Retrieved IVF: Realistic Expectations
Having 8 eggs retrieved during IVF raises many questions. People wonder about the chances of successful fertilization and blastocyst development. Knowing what to expect can help prepare for the next steps in fertility.
Maturation Rate Predictions
Not all eggs are ready for fertilization. About 80-90% of eggs are mature, but the rest are not. This percentage can change based on age, health, and more.
With 8 eggs, we might see 6-7 mature ones. But, this number can vary a lot from person to person.
Expected Fertilization Numbers
After eggs mature, they need to be fertilized. The success of fertilization depends on sperm quality and egg health.
Usually, 60-70% of mature eggs fertilize. So, with 6-7 mature eggs, we might see 3-4 fertilized ones.
Typical Blastocyst Development Outcomes
Then, we see how many fertilized eggs become blastocysts by day 5 or 6. About 40-60% of fertilized eggs reach this stage.
Starting with 8 eggs and ending with 3-4 fertilized ones, we might see 1-2 become blastocysts. But, actual results can vary a lot.
Stage | Average Success Rate | Expected Number (out of 8 eggs) |
Maturation | 80-90% | 6-7 |
Fertilization | 60-70% | 3-4 |
Blastocyst Development | 40-60% | 1-2 |
Knowing these expectations can help patients feel more prepared for IVF. While results can vary, understanding the process makes the journey clearer.
12 Fertilized Eggs: How Many Blastocysts to Expect
Looking into the growth of 12 fertilized eggs gives us key insights into IVF success. Patients often wonder how many will reach the blastocyst stage.
Statistical Analysis of Medium-Sized Cohorts
Studies show that about 3-4 eggs usually turn into blastocysts from a group of 12. This success rate depends on many things. These include the quality of the eggs and sperm, and how well the IVF lab works.
Let’s dive into the numbers more:
Number of Fertilized Eggs | Average Blastocyst Formation Rate | Expected Number of Blastocysts |
12 | 30-40% | 3-4 |
10 | 30-40% | 3 |
8 | 30-40% | 2-3 |
Quality Distribution Patterns
The quality of blastocysts matters a lot. They are graded on how well they look, including the inner cell mass and trophectoderm. High-quality blastocysts have a better chance of implantation and successful pregnancy.
Here’s how blastocyst quality usually breaks down:
- High-quality blastocysts: 20-30%
- Average-quality blastocysts: 40-50%
- Low-quality blastocysts: 20-30%
Freezing and Success Rates
Blastocysts that are good for transfer or freezing are considered viable. Freezing, or vitrification, has greatly improved thawed blastocyst survival. Studies show that vitrification can achieve survival rates of over 90%.
Not all blastocysts are frozen. The choice to freeze depends on the blastocyst’s quality and how well it’s doing.
Understanding these patterns and factors helps patients set realistic goals. It also helps them make better choices for their IVF journey.
Outcomes with 30 Eggs Retrieved IVF
Getting 30 eggs during an IVF cycle shows a strong ovarian response. But what does this mean for the outcome? For patients who are classified as high responders, it’s important to understand the journey from egg retrieval to possible pregnancy.
High Responder Statistics
Being a high responder can be both a blessing and a challenge. Studies show that women who produce many eggs have a higher chance of getting pregnant. But they also face increased risks of certain complications.
Recent statistics say that patients with 30 retrieved eggs can expect about 80% maturation. This means about 24 eggs will be mature and ready for fertilization.
Maturation and Fertilization in Large Cohorts
The process of maturation and fertilization is complex. With a large number of eggs, the chances of successful fertilization increase. But, there are more variables that can affect the outcome.
Typically, with 24 mature eggs, the fertilization rate can range between 60% to 80%. This results in roughly 15 to 20 fertilized embryos. Not all fertilized embryos will develop into viable blastocysts.
Expected Blastocyst Numbers
The journey from a fertilized egg to a blastocyst is complex. Blastocysts are embryos that have developed for about 5 days after fertilization. They are a critical stage in IVF treatment.
On average, out of 15-20 fertilized embryos, about 6-10 are expected to develop into blastocysts. This number can vary based on several factors, including egg and sperm quality, as well as the expertise of the embryology lab.
Stage | Average Number | Percentage |
Eggs Retrieved | 30 | 100% |
Mature Eggs | 24 | 80% |
Fertilized Embryos | 15-20 | 60-80% |
Blastocysts | 6-10 | 30-50% |
Potential Complications with High Egg Numbers
While having a large number of eggs can increase the chances of successful IVF, it also comes with risks. One of the most significant complications is Ovarian Hyperstimulation Syndrome (OHSS). This condition can range from mild to severe.
“The risk of OHSS is higher in women who produce many eggs in response to stimulation. Careful monitoring and tailored treatment protocols can help mitigate this risk.”
– Medical Expert, Fertility Specialist
Understanding these risks and working closely with a fertility specialist can help manage risks and optimize outcomes.
IVF Attrition Rate: Understanding the Numbers
The IVF journey has many stages, each with its own hurdles, like embryo attrition rate. This rate shows how many fertilized eggs don’t make it to the blastocyst stage. Knowing this rate helps set realistic goals and make better choices during IVF.
Average Drop-Off at Each Development Stage
IVF has several steps, from egg retrieval to blastocyst formation. At each step, embryos can fail to progress. Studies reveal that:
- Not all retrieved eggs mature
- Not all mature eggs fertilize
- Not all fertilized eggs develop into blastocysts
Attrition rates can be quite high. For example, starting with 10 eggs, some may not mature, others may not fertilize, and some fertilized eggs may not develop.
Age-Related Attrition Patterns
Age greatly affects IVF attrition rates. As women get older, their eggs’ quality and number decrease, leading to higher attrition. Women under 35 usually have lower attrition rates than those over 40. This decline impacts both the number and quality of eggs.
Here’s how age influences IVF attrition:
Age Group | Average Attrition Rate |
Under 35 | Lower attrition (e.g., 20-30%) |
35-40 | Moderate attrition (e.g., 30-50%) |
Over 40 | Higher attrition (e.g., 50-70%) |
Emotional Preparation for Embryo Attrition
Dealing with embryo attrition is emotionally tough for many. It’s key to have realistic hopes and emotional support during IVF. Talking about possible outcomes with doctors can help set expectations.
Patients should be ready for the chance that not all fertilized eggs will become viable embryos. Having emotional strength and a support network is vital in facing these challenges.
How Many Blastocysts Are Normal for IVF?
IVF patients often ask about the normal number of blastocysts. This number varies based on several factors. These include the patient’s age, egg quality, and the number of eggs retrieved.
Defining “Normal” Results by Age Group
The number of blastocysts can change with age. Younger patients usually have more because their eggs are better. We divide patients into age groups to better understand these expectations.
Age Group | Average Number of Blastocysts |
Under 35 | 4-6 |
35-37 | 3-5 |
38-40 | 2-4 |
41-42 | 1-3 |
Statistical Averages from Clinical Studies
Clinical studies give us insights into blastocyst numbers in IVF. For patients under 35, the average is 4 to 6 blastocysts. Patients aged 35-37 usually have 3-5 blastocysts.
When to Consider Additional Retrieval Cycles
Some patients may not get enough blastocysts in their first cycle. We then consider more cycles based on several factors. These include the patient’s ovarian reserve, how well they respond to stimulation, and their overall health.
It’s key for patients to talk to their healthcare provider about their situation. This way, they can understand what to expect from their IVF journey.
Conclusion: Setting Realistic Expectations for Your Fertility Journey
As we wrap up our look at IVF and blastocyst development, it’s key to know setting realistic hopes is vital. IVF success rates change a lot. This depends on age, egg quality, and the clinic’s skill.
Understanding IVF’s stages helps you know what to expect. From egg retrieval to blastocyst formation, it’s a complex journey. Many factors can affect the outcome.
To have realistic hopes, think about your own situation. This includes your age and egg or sperm quality. Your fertility specialist can offer advice tailored to you. This helps you make smart choices about your care.
Being informed and ready helps you face your fertility journey with confidence. We’re here to support you, providing top-notch healthcare and support for international patients.
FAQ
What percentage of fertilized eggs make it to blastocyst?
About 40% to 60% of fertilized eggs reach the blastocyst stage. This success rate can change between clinics. It depends on their protocols, equipment, and expertise.
How many fertilized eggs make it to day 5?
Not all eggs make it to day 5. The blastocyst formation rate is around 40-60%. The quality of these blastocysts is also checked, which is key for their viability.
What is the IVF fertilization rate?
About 80% of mature eggs get fertilized. But, this rate can change based on egg and sperm quality, and fertilization technique.
What is IVF attrition?
IVF attrition is when fewer viable embryos are left during the IVF process. This happens at different stages, from egg retrieval to blastocyst formation.
How many blastocysts are normal for IVF?
The number of normal blastocysts for IVF varies. It depends on the patient’s age, egg quality, and how many eggs are retrieved. Clinical studies give averages to help patients understand what to expect.
If I start with 4 fertilized eggs on day 1, how many blastocysts can I expect?
Usually, 1-2 embryos turn into blastocysts by day 5. With 4 fertilized eggs, expecting fewer blastocysts is common.
If I have 8 eggs retrieved, what are my chances of getting blastocysts?
With 8 eggs, some will fertilize and become blastocysts. The exact number depends on egg maturation, fertilization, and typical blastocyst development.
If I have 12 fertilized eggs, how many blastocysts can I expect?
About 3-4 embryos from 12 fertilized eggs usually become viable blastocysts. The quality of these blastocysts and their freezing and transfer options are also important.
What happens if I have 30 eggs retrieved during IVF?
Having 30 eggs can lead to many blastocysts. But, consider the risks of ovarian hyperstimulation syndrome (OHSS) and the maturation and fertilization rates.
How does age affect IVF attrition rates?
Age greatly affects attrition rates, with older women facing higher rates. Knowing how age impacts IVF success helps set realistic expectations for fertility.
When should I consider additional retrieval cycles?
Deciding on more retrieval cycles depends on blastocyst numbers, age, and egg quality. Clinical studies offer averages to guide when more cycles might be needed.
References
National Center for Biotechnology Information. Fertilized Egg to Blastocyst Conversion Rate in IVF. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8236141/