Expert ICSI Guide: Injecting Sperm Safely
Injecting sperm into an egg, or ICSI, is a powerful technique. This complete guide explains how it works, why it’s used, and success rates. Immature Ovarian Follicles are key to female reproductive health. They are very important in polycystic ovary syndrome (PCOS). This condition affects about 10-15% of women of childbearing age worldwide.
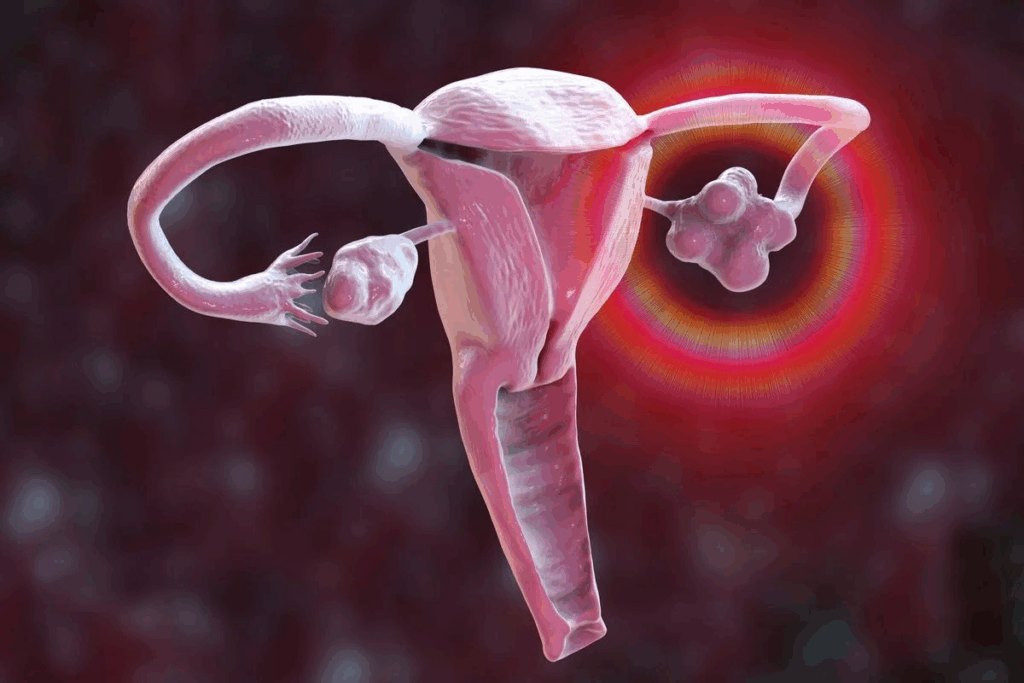
Ovarian follicles are tiny sacs in the ovaries. They hold eggs at different stages of growth. In women with PCOS, these follicles often don’t mature right. This can stop ovulation and make it hard to get pregnant.
At Liv Hospital, we know how important it is to understand and manage Immature Ovarian Follicles. We aim to improve fertility by following international medical standards. Our care is focused on each patient’s needs.
Key Takeaways
- Immature Ovarian Follicles are a hallmark of PCOS, affecting ovulation and fertility.
- Understanding the causes of immature follicles is key for effective management.
- Liv Hospital offers detailed care for women with PCOS, with plans tailored to each patient.
- Advanced medical protocols can enhance reproductive health.
- Patient-centered care is vital for meeting each patient’s unique needs.
The Normal Ovarian Follicle Development Process
Ovarian follicle development is key for reproductive health. It’s about the growth and maturation of follicles in the ovaries. These follicles hold and release eggs. Knowing this process helps us understand issues with immature follicles.
The growth of ovarian follicles happens in two phases. The first is the pre-antral phase, where follicles grow without gonadotropins. The second is the antral phase, where follicles need gonadotropins like FSH to grow and mature.
Stages of Follicular Growth and Maturation
Follicular development goes through several stages. It starts with primordial follicles and ends with preovulatory follicles. Primordial follicles are the first stage, with an oocyte and flat granulosa cells. They grow into primary follicles, then secondary follicles, and lastly antral follicles, which have a fluid-filled cavity.
Stage | Description |
Primordial | Oocyte surrounded by flat granulosa cells |
Primary | Oocyte surrounded by a single layer of cuboidal granulosa cells |
Secondary | Oocyte surrounded by multiple layers of granulosa cells |
Antral | Fluid-filled cavity (antrum) forms, containing the oocyte |
Preovulatory | Fully mature follicle ready for ovulation |
Hormonal Regulation of Follicle Development
Hormones are vital for follicular growth and maturation. FSH helps follicles grow by stimulating granulosa cells. LH (Luteinizing Hormone) triggers ovulation by releasing the mature oocyte. The balance between FSH and LH is essential for egg release.
Keeping hormone levels balanced is critical for follicular development. Any imbalance can cause issues like immature follicles. This is often seen in conditions like Polycystic Ovary Syndrome (PCOS).
What Are Immature Ovarian Follicles?
Understanding Immature Ovarian Follicles is key to diagnosing and managing PCOS. These follicles are follicles that have arrested development. They fail to mature and release an egg, leading to reproductive issues.
We will look into the traits of these follicles and how they are spotted, mainly in women with PCOS. Women with PCOS often have small follicles in both ovaries.
Defining Characteristics of Arrested Follicles
Arrested follicles don’t grow as they should. They stay small and underdeveloped, usually between 2-9 mm in size. Having many small follicles in both ovaries is a sign of this issue.
Measuring and Identifying Immature Follicles
To spot Immature Ovarian Follicles, ultrasound imaging is used. It checks the number and size of follicles in the ovaries. A diagnosis is made if there are multiple small follicles, 20 or more, measuring 2-9 mm.
Transvaginal ultrasound helps us measure and count follicles accurately. Seeing bilateral ovarian follicles is a big clue. Our experts know how to spot these signs.
Polycystic Ovary Syndrome: Primary Cause of Immature Ovarian Follicles
Polycystic ovary syndrome (PCOS) is a complex disorder that leads to Immature Ovarian Follicles. It is marked by large ovaries with many small cysts, irregular periods, and high levels of male hormones.
PCOS is a big health problem for women of childbearing age. Knowing how common it is and why follicles don’t mature is key to treating it well.
PCOS Prevalence Among Reproductive-Age Women
PCOS affects a lot of women around the world. Studies show it affects 8% to 13% of women of childbearing age. But, the exact number can change based on who is studied and how they are diagnosed.
Women with PCOS often face other health issues like insulin resistance, type 2 diabetes, and trouble getting pregnant. A big sign of PCOS is having many small follicles in both ovaries. This makes it hard to diagnose and treat.
- Prevalence rates vary globally, with some regions reporting higher rates due to genetic and environmental factors.
- The diagnosis of PCOS is typically made based on the Rotterdam criteria, which include ovarian morphology, ovulatory dysfunction, and clinical or biochemical signs of hyperandrogenism.
Pathophysiology of Follicular Arrest in PCOS
PCOS’s causes are complex, involving hormones and metabolism. A big part of it is when follicles stop growing, leading to many immature ones.
Several things cause follicles to stop growing in PCOS, including:
- Hyperandrogenism: High levels of male hormones mess with follicle growth.
- Insulin Resistance: When the body can’t use insulin well, it makes more androgens.
- Hormonal Imbalance: The wrong levels of hormones like LH and FSH mess up follicle growth.
The exact reasons for follicular arrest in PCOS are not fully understood. But, it’s clear that hormones and metabolism play a big role.
Understanding PCOS is key to finding good treatments. By tackling the root causes of follicular arrest, doctors can help women with PCOS more effectively.
Multiple Bilateral Ovarian Follicles: What They Mean
When doctors find multiple bilateral ovarian follicles, they often diagnose Polycystic Ovary Syndrome (PCOS). This condition shows up as many small follicles in both ovaries, mostly on the edges. Seeing these follicles is key to diagnosing PCOS, a common issue for women of childbearing age.
Distribution Patterns of Immature Follicles
In PCOS, immature follicles spread out in a specific way. They form a “string of pearls” look on ultrasound. This look is a clear sign of PCOS. The follicles are found around the edge of the ovary, making it easy to spot.
Small Peripheral Follicles in Both Ovaries
The main sign of PCOS is small peripheral follicles in both ovaries. These follicles don’t grow and release an egg. Hormonal imbalances and other PCOS factors stop them from maturing.
Knowing about ovarian follicles bilaterally is key to treating PCOS. Ultrasound shows these follicles clearly. This helps doctors make the right diagnosis and plan the best treatment.
Hormonal Imbalances Leading to Follicular Development Arrest
Hormonal imbalances play a big role in stopping ovarian follicle growth. Women with polycystic ovary syndrome (PCOS) often face these issues. This leads to the formation of Immature Ovarian Follicles.
One major hormonal imbalance is hyperandrogenism. This means having too much testosterone. It stops ovarian follicles from growing properly.
Hyperandrogenism and Elevated Testosterone Levels
Hyperandrogenism is a key feature of PCOS. It affects how ovarian follicles grow. High testosterone levels mess with the feedback loops that control follicle growth, causing them to stop growing.
Research shows that women with PCOS have more androgens. These hormones help cause follicles to stop growing. The exact reasons are complex, involving androgens, insulin, and other hormones.
Luteinizing Hormone Abnormalities
Luteinizing hormone (LH) levels are also important. LH helps control follicle growth and ovulation. In PCOS, LH levels are too high. This messes up the LH/FSH ratio and stops follicles from growing.
This imbalance in LH and FSH stops follicles from growing right. They stay immature.
Secondary FSH Suppression Mechanisms
High LH and androgen levels also lower FSH. This disrupts follicle growth even more. It’s another way hormonal imbalances affect follicles.
Here’s a table showing how hormonal imbalances affect follicular development:
Hormone | Normal Levels | Levels in PCOS | Effect on Follicular Development |
Testosterone | Low | Elevated | Disrupts normal follicular growth |
LH | Normal LH/FSH ratio | Elevated | Disrupts LH/FSH ratio, contributing to follicular arrest |
FSH | Normal | Suppressed | Impairs follicular maturation |
Understanding these hormonal imbalances is key. It helps us find better ways to manage follicular development. By fixing these hormonal issues, we can help follicles grow better and improve reproductive health.
Insulin Resistance and Its Impact on Ovarian Function
Insulin resistance is key in PCOS, affecting how ovaries work. We’ll look at how it impacts ovarian function. This includes its role in metabolic issues and how it affects insulin and androgen levels.
Metabolic Dysfunction in Follicular Development
Insulin resistance messes with how follicles grow. It causes too much insulin, which stops follicles from growing right. This leads to many immature follicles, a sign of PCOS.
The process of follicular development is complex. It involves insulin, androgens, and other hormones. Hyperinsulinemia makes more androgens, which stops follicles from growing.
Metabolic Factor | Impact on Follicular Development |
Hyperinsulinemia | Increases androgen production, disrupting follicular growth |
Insulin Resistance | Leads to hyperinsulinemia, affecting follicular maturation |
Androgen Excess | Contributes to follicular arrest and PCOS pathology |
Insulin-Androgen Interactions in the Ovary
Insulin and androgens work together in the ovary, which is key in PCOS. Insulin helps make more androgens, and androgens make insulin resistance worse. This creates a cycle that’s hard to break.
“The synergistic effect of insulin and androgens on the ovary exacerbates metabolic dysfunction, leading to the characteristic features of PCOS, including multiple immature follicles.”
Knowing how insulin and androgens interact is important. It helps us find better ways to manage PCOS and improve fertility.
Diagnosing Immature Follicles Through Imaging
Imaging techniques are key in spotting Immature Ovarian Follicles. Getting the diagnosis right is essential for managing issues like polycystic ovary syndrome (PCOS). This condition often shows up with many immature follicles.
Transvaginal Ultrasound Criteria
Transvaginal ultrasound is a top tool for checking ovarian shape. It looks for ≥20 follicles that are 2-9mm in size per ovary. This method gives a clear view of the ovaries and is great for spotting PCOS signs.
“The use of transvaginal ultrasound has changed how we diagnose ovarian issues,” say experts in reproductive medicine.
Transabdominal Imaging Standards
Transabdominal imaging is useful when transvaginal ultrasound can’t be used. It looks for ≥10 follicles. Though it’s not as detailed as transvaginal ultrasound, it’s good for seeing where follicles are.
Bilateral Ovarian Follicles on Ultrasound Interpretation
PCOS is marked by follicles on both ovaries. Doctors look for even follicle distribution in both ovaries. Seeing many small follicles on the edges is a sign of PCOS.
Getting a good diagnosis and treatment for immature follicles depends on reading imaging results well. By using both clinical checks and advanced imaging, doctors can create specific treatment plans to tackle follicle issues.
The Rotterdam Criteria for Polycystic Ovarian Morphology
Understanding the Rotterdam criteria is key for diagnosing polycystic ovarian morphology. It ensures doctors follow the same steps to diagnose PCOS. This makes sure diagnoses are consistent everywhere.
Diagnostic Standards for Clinical Practice
The Rotterdam criteria say up to 25% of healthy women can have polycystic ovaries. This shows how important it is to have clear rules for diagnosing PCOS. It helps tell the difference between normal and abnormal.
Key diagnostic features include:
- Presence of 20 or more follicles in each ovary
- Follicular size between 2-9 mm
- Ovarian volume greater than 10 mL
These rules help doctors diagnose PCOM correctly. They prevent doctors from missing or overdiagnosing the condition.
When Multiple Follicles Are Considered Normal
Sometimes, having many follicles is just normal, not PCOS. The Rotterdam criteria remind doctors to look at ultrasound results with symptoms and hormone levels. This is important.
“The presence of polycystic ovarian morphology on ultrasound is not sufficient for a diagnosis of PCOS; clinical correlation is essential.”
This careful approach helps doctors give the right care. It also prevents unnecessary treatments.
Clinical Consequences of Persistent Immature Follicles
Persistent immature follicles can have big effects on women’s health. These effects reach beyond just fertility, touching on overall well-being.
Anovulation and Fertility Challenges
One major issue with immature follicles is anovulation. This makes it hard to get pregnant. Women with polycystic ovary syndrome (PCOS) often face this problem.
Women with these follicles struggle with getting pregnant. This can cause a lot of emotional pain.
Menstrual Irregularities and Hormonal Symptoms
Women with immature follicles often have irregular periods. This can mean periods that are too short or too long, or even no periods at all. Hormonal imbalances, like hyperandrogenism, can cause acne, extra hair, and balding.
These symptoms can hurt how a woman feels about herself. They can affect her self-esteem and overall happiness.
Long-term Health Risks Associated with Follicular Arrest
There are serious long-term health risks with persistent immature follicles. Women with PCOS are at higher risk for metabolic syndrome. This includes problems like insulin resistance, high blood pressure, and bad cholesterol levels.
They also face a higher risk of cardiovascular disease. This is because of the metabolic and hormonal issues. It’s important to manage these risks over time.
We need to tackle these health issues head-on. Understanding the effects of immature follicles helps us create better care plans. This way, we can improve the lives of women affected.
Medical Management Approaches
Managing Immature Ovarian Follicles needs a mix of strategies. We’ll look at medical ways to handle this, focusing on treatments that help follicles grow and improve reproductive health.
Hormonal Treatments to Regulate Follicular Development
Hormonal treatments are key in managing Immature Ovarian Follicles. Birth control pills are often used to control menstrual cycles and lower androgen levels. They help balance hormones in women with polycystic ovary syndrome (PCOS), a main cause of these follicles.
Also, clomiphene citrate is given to women trying to get pregnant. It helps release hormones needed for ovulation, boosting fertility chances.
Insulin-Sensitizing Medications
Medicines like metformin are vital for managing Immature Ovarian Follicles, mainly in women with insulin resistance. They make the body more sensitive to insulin, lowering insulin and androgen levels. This helps in regular ovulation.
Research shows metformin can make menstrual cycles regular and improve ovulation in women with PCOS. This tackles some reasons behind Immature Ovarian Follicles.
Anti-Androgen Therapies
Anti-androgen therapies help with symptoms of too much androgen, like hair growth and acne. Spironolactone blocks androgen effects, easing these symptoms.
Lowering androgen levels helps create a better environment for follicle growth. This can lead to better ovulation and fertility.
Lifestyle Interventions for Women with Immature Follicles
Lifestyle changes are key for women with Immature Ovarian Follicles. Adopting healthier habits can greatly improve well-being and follicular health.
Dietary Modifications to Improve Follicular Health
Changing your diet is essential for managing immature follicles. Eating a balanced diet can help balance hormones and improve insulin sensitivity.
- Eat more whole foods like vegetables, fruits, and whole grains
- Drink less processed foods and sugars
- Add healthy fats and lean proteins to your meals
A study in the Journal of Clinical Endocrinology and Metabolism shows diet changes can help women with PCOS. This is a common cause of immature follicles.
“Lifestyle modification, including diet and exercise, is a cornerstone in the management of PCOS, improving insulin sensitivity and hormonal balance.” Journal of Clinical Endocrinology and Metabolism
Exercise Recommendations and Benefits
Regular exercise is vital for women with immature follicles. It helps with weight control, improves insulin sensitivity, and lowers androgen levels.
Exercise Type | Benefits | Recommended Frequency |
Aerobic Exercise | Improves insulin sensitivity, reduces androgen levels | At least 150 minutes per week |
Resistance Training | Enhances muscle mass, improves metabolic health | 2-3 times per week |
High-Intensity Interval Training (HIIT) | Effective for weight loss, improves cardiovascular health | 2-3 times per week |
Weight Management Strategies
Weight management is tough for many women with immature follicles, like those with PCOS. Losing a little weight can improve menstrual cycles, ovulation, and hormone balance.
Effective weight management strategies include:
- Set realistic weight loss goals
- Combine diet changes with regular exercise
- Keep track of progress and adjust plans as needed
By making these lifestyle changes, women with immature follicles can see big improvements. This can greatly enhance their quality of life.
Conclusion: Future Directions in Understanding and Treating Immature Ovarian Follicles
Understanding Immature Ovarian Follicles is key to solving reproductive health problems, like Polycystic Ovary Syndrome (PCOS). Research into PCOS and follicle issues is leading to better ways to manage them.
Future treatments will aim to fix the problems at their source. New research on PCOS could lead to better treatments. This could greatly help women with these conditions.
As we learn more about how follicles grow, we’ll find new ways to help. This research could greatly improve fertility and reproductive health for many women.
Supporting more research on follicles and related issues is important. It could lead to better, more tailored care for women. This could greatly improve their lives.
Frequently Asked Questions
What are Immature Ovarian Follicles, and how do they relate to PCOS?
Immature Ovarian Follicles are not fully grown in the ovaries. They are common in Polycystic Ovary Syndrome (PCOS). This is a hormonal disorder that affects women of childbearing age.
How are immature ovarian follicles diagnosed?
Doctors use ultrasound to find these follicles. They look for many small follicles in the ovaries. The Rotterdam criteria help diagnose PCOS by looking at these follicles and other signs.
What is the significance of multiple bilateral ovarian follicles?
These follicles are a key sign of PCOS. They show a higher risk of not ovulating and fertility issues. Their small size and location are also typical of PCOS.
How do hormonal imbalances contribute to follicular development arrest?
Hormonal problems, like too much androgen, can stop follicles from growing. This leads to the formation of immature follicles.
What is the role of insulin resistance in the development of immature ovarian follicles?
Insulin resistance, linked to PCOS, affects how follicles grow. It causes metabolic problems and disrupts hormone levels, leading to immature follicles.
What are the clinical consequences of persistent immature follicles?
These follicles can cause not ovulating, fertility issues, and irregular periods. They also raise the risk of metabolic and heart diseases over time.
What are the treatment options for immature ovarian follicles?
Treatments include hormonal therapies and medications that help insulin sensitivity. Anti-androgen treatments and lifestyle changes like diet and exercise are also options.
Can lifestyle changes improve follicular health in women with PCOS?
Yes, making healthy lifestyle choices can improve follicular health. This includes eating right, exercising, and managing weight.
What is the future of research on immature ovarian follicles and PCOS?
Research is ongoing to better understand these follicles and PCOS. The goal is to find more effective treatments and management strategies.









