Last Updated on October 22, 2025 by mcelik

Spotting metastasis is key in cancer care. Yet, even with advanced tools like PET scans, metastasis detection can be challenging. Research shows that PET scan miss metastasis occurs, leading to false negatives. For example, PET/CT scans have an overall detection rate of about 81.3% for metastases according to a study on Springer. While helpful, this highlights that PET scans are not perfect. Awareness of these limitations is vital for doctors and patients to consider additional testing for accurate metastasis assessment.
.
PET scans play a key role in cancer staging. They help doctors understand how tumors work. This is because they show how active tumors are metabolically.
PET imaging works by showing how cancer cells differ from normal cells. It uses a special tracer, like Fluorodeoxyglucose (FDG), to find tumors. This is because tumors use more glucose than normal cells.
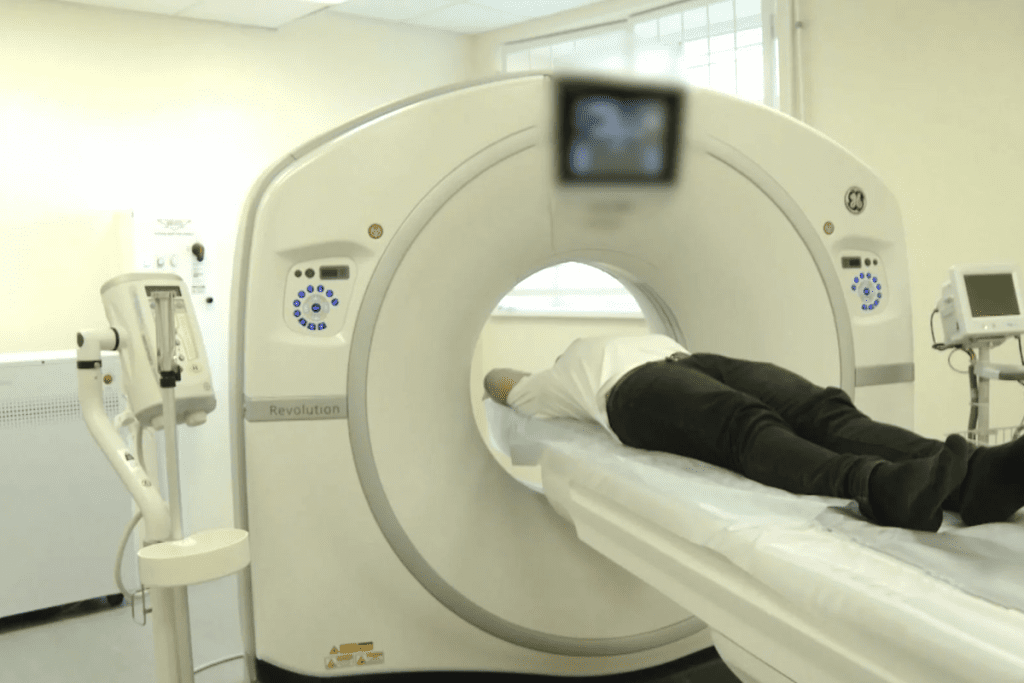
First, the tracer is injected into the patient’s blood. Then, the body is scanned with a PET scanner. The scanner picks up the tracer’s signals, making detailed images of the body’s activity.
How well PET scans work depends on how much the tracer is taken up by tumors. Tumors that use a lot of glucose are easier to spot. But, tumors that don’t use much glucose might be missed, leading to false negatives.
“The sensitivity of PET scans in detecting cancer metastasis is closely linked to the metabolic activity of the tumor cells.”
PET scans have big advantages over CT scans and MRI. CT scans show the body’s structure, and MRI gives clear images of soft tissues. But, PET scans show how active tissues are.
Using PET with CT (PET/CT) is now common. It combines metabolic and anatomical details in one scan. This makes cancer staging more accurate and helps find metastasis better.

PET scans are a key tool in cancer staging, but they can miss metastasis. This fact has big implications for patient care. Knowing how well PET scans work is vital for doctors and patients.
Studies have shown that PET scans can miss metastasis. The rate of false negatives varies with cancer type, metastasis location, and scan technology. For example, a study found a 15% to 20% false negative rate for some cancers.
“The false negative rate for PET scans in detecting metastasis is a critical factor in cancer staging,” experts say. “Knowing this is key for accurate diagnosis and treatment planning.”
In real life, PET scans face many challenges in finding metastasis. The size, metabolic activity, and location of the metastasis affect detection. Small or low-activity metastases might not be seen, leading to false negative results.
These challenges highlight the need to consider all clinical information when interpreting PET scans. This approach helps doctors make better decisions for patient care.
PET scans can spot metastasis, but only if the lesions are big enough. These scans are key in cancer staging, showing if cancer has spread. But, how well they work depends on the size of the cancer spots.
Sub-centimeter metastases are hard for PET scans to find. They look for cancer cells’ activity, using a sugar-like substance called FDG. But, spots smaller than 1 cm can be tricky to spot because of the scan’s resolution and the partial volume effect.
Technical limitations of PET scans mean small metastases might not show up. This can lead to cancer being understaged, affecting treatment plans and outcomes.
Millimeter-sized lesions are even harder to detect. Modern PET scanners can spot things about 4-5 mm in size. But, the chance of finding a lesion depends on its activity, where it is, and the background activity.
Advancements in scanner technology and image algorithms help detect smaller lesions. Yet, PET scanning’s physical limits mean very small metastases are hard to find.
Metabolic factors are key in how well PET scans find metastatic disease. The activity of tumors and their spread can affect PET scan sensitivity.
Some tumors don’t take up enough FDG for PET scans to see them. This can cause false negatives, mainly in tumors with low activity. Cancers with inherently low glucose metabolism are often missed.
Well-differentiated thyroid cancer and some mucinous adenocarcinomas are hard to spot on PET scans. They don’t show up well because they’re not very active metabolically.
Dormant or slow-growing metastases are hard to find with PET scans. They don’t show enough activity to be seen. Slow-growing metastases can stay dormant for a long time, making them tricky to spot.
The problem with dormant metastases is they don’t use enough glucose to show up on scans. This can lead to false negatives, affecting treatment plans and patient results.
Necrotic or cystic lesions in tumors or metastases make PET scans harder to read. Necrotic areas in tumors can look like they have low FDG uptake, hiding the real tumor.
Cystic metastases are tough because the cyst part doesn’t take up FDG. This makes it hard to tell them apart from benign cysts. Advanced imaging and careful analysis are needed for accurate diagnosis.
Some parts of the body are hard for PET scans to find cancer metastases. The body’s complex shape and PET scan tech limits make it hard to spot cancer in key spots.
Finding cancer in the brain with PET scans is tough. This is because normal brain cells use a lot of glucose, hiding cancer cells. But, with careful look and extra scans, PET scans can do better.
Finding cancer in the liver is tricky for PET scans. The liver’s changing activity and cancer cells that match the liver’s activity make it hard. New imaging and special tracers can help see cancer better.
PET scans can find bone cancer, but it depends on the type. Cancer that breaks down bone is easier to spot than cancer that makes bones harder. Using 18F-fluoride can help find bone cancer better.
Finding cancer in the lining of the belly is hard because it’s small and spread out. Finding cancer in lymph nodes is better, but size and inflammation can affect it. Better imaging and high-tech scanners help see these cancers clearly.
| Anatomical Location | PET Scan Detection Sensitivity | Challenges |
| Brain | Low to Moderate | High glucose uptake in normal brain tissue |
| Liver | Moderate | Variable metabolic activity, isometabolic lesions |
| Bone | Moderate to High | Type of bone involvement (lytic vs. sclerotic) |
| Peritoneal | Low | Small size, diffuse nature |
| Lymph Nodes | Moderate to High | Node size, inflammation |
Finding metastases in different parts of the body is a big challenge for PET scans. Knowing these challenges is key for accurate cancer diagnosis and treatment plans.
Histological and biological factors are key in how well PET scans can find metastases. The type of tumor affects how well PET imaging works.
Well-differentiated and low-grade tumors are hard to spot on PET scans. They don’t take up as much FDG as high-grade tumors do. This means well-differentiated metastases might not show up well, leading to false negatives.
For example, some low-grade metastases might not have a high enough glucose rate to stand out. This makes them tricky to find with FDG-PET.
Mucinous and colloid metastases are also tough to find with PET scans. They have low cell count and lots of mucin, which can hide the FDG signal. So, mucinous metastases might show up as low or no FDG uptake, making them hard to spot.
Finding mucinous metastases requires careful look at PET scan results. This is true, even if the main tumor is mucinous.
Sclerotic bone metastases are also hard to detect with PET scans. Even though they might show some FDG uptake, heavily calcified or sclerotic ones can be tricky. The dense bone can hide the metabolic activity, making them hard to see on PET scans.
In some cases, sclerotic bone metastases need more imaging, like bone scintigraphy or MRI. This is to get a clear picture of their size and activity.
Technical and procedural variables are key to PET scan accuracy for detecting metastasis. The precision of PET scans depends on several factors. These can be grouped into scanner-related, patient-related, and procedural factors.
The quality and resolution of the PET scanner greatly affect its ability to spot metastatic lesions. Modern PET scanners with advanced technology can find smaller lesions. They also give more accurate measurements of tracer uptake.
Key factors affecting scanner quality include:
Proper patient preparation is vital for the best PET scan results. Factors like fasting, blood glucose levels, and avoiding exercise before the scan matter a lot.
Important patient preparation considerations include:
The timing of PET imaging after radiotracer administration is critical. The best time varies based on the tracer used and the cancer type.
Factors to consider when timing PET scans include:
Understanding and optimizing these variables can improve PET scan accuracy. This helps detect metastasis better and improves patient care.
Finding micrometastases and early disease spread is hard in cancer staging. These small metastases can change treatment plans and patient results.
Micrometastatic disease means small, often unseen, metastases. They are too small for standard imaging, like PET scans, to find. These tiny spots can be clinically significant, showing early disease spread.
What counts as micrometastases can vary. But they are usually tumors smaller than 2 mm. The big challenge is finding these tiny spots with today’s tools.
PET scans can’t always find micrometastases. This is because of their small size and how active the tumor cells are. Low FDG-avidity tumors are the hardest to spot.
| Detection Method | Limitations | Potential Solutions |
| PET Scan | Resolution limits, low FDG uptake | Advanced tracers, hybrid imaging |
| CT Scan | Soft tissue contrast, small lesions | Contrast enhancement, high-resolution scans |
| MRI | Cost, availability, specific sequence limitations | Advanced sequences, contrast agents |
Undetectable metastases can greatly affect treatment and outlook. They are a focus of ongoing research.
Having micrometastases means a higher chance of cancer coming back. It might mean more intense or specific treatments. Knowing how important these hidden metastases are is key to better care.
New imaging methods and tracers are promising for spotting micrometastases better. More research is needed to improve cancer staging and treatment results.
Understanding how PET scans detect cancer is key. Different cancers have unique traits that affect PET scan results. This is important for spotting metastasis.
Some cancers are tough to spot with PET scans. This is because they don’t take up much FDG. For example, breast cancer and prostate cancer can be hard to find.
| Cancer Type | False-Negative Rate | Detection Challenges |
| Breast Cancer (Lobular) | High | Low FDG uptake, dense breast tissue |
| Prostate Cancer (Low-grade) | Moderate to High | Low metabolic activity, variable FDG uptake |
| Mucinous Tumors | High | Low cellular density, high mucin content |
But, some cancers are easier to find with PET scans. Lung cancer and lymphoma show up well because they use a lot of FDG.
Knowing how PET scans work for different cancers is vital. It helps doctors make better treatment plans. This way, they can give patients the best care possible.
The introduction of hybrid imaging like PET/CT and PET/MRI has changed cancer diagnosis. These methods combine PET’s metabolic info with CT or MRI’s anatomy. This gives a clearer view of tumors and their spread.
PET/CT is a key tool in cancer care. It offers metabolic and anatomical details. This helps spot and understand tumors better.
Yet, PET/CT has its limits. It might miss small or inactive lesions. Also, the CT part uses radiation, a concern for young patients or those needing many scans.
PET/MRI is another big step in hybrid imaging. It offers better soft tissue detail than PET/CT and less radiation. It’s great for:
Using both PET/CT and PET/MRI for cancer staging is best. It gives a full picture of a patient’s disease. This way, doctors can:
Combining data from various imaging methods helps doctors make better choices. This leads to better care for patients.
Researchers are working on tracers that target specific cancer cells. This could lead to better detection of metastases. They aim to create tumor-specific radiopharmaceuticals for more accurate PET scans.
Tumor-specific radiopharmaceuticals are made to attach to certain cancer cells. This makes them great for diagnosing and staging cancers. For example, Fluorothymidine (FLT) helps measure cell growth, which shows how aggressive a tumor is.
These advanced tracers can spot metastases better than traditional FDG PET scans. They target specific cancer cell traits, giving a deeper look at the disease.
Some cancers are hard to find with FDG PET scans because they don’t show up well. New tracers are being made to solve this problem. For instance, prostate-specific membrane antigen (PSMA) targeted tracers are good at finding prostate cancer metastases.
These new tracers help find more cancers and track how well treatments work. They give doctors more accurate info, helping them make better care plans for patients.
Targeted molecular imaging uses tracers that stick to cancer-related molecules. This makes PET scans more precise, helping spot metastases better.
The field of making these targeted tracers is growing fast. Scientists are always looking for new targets and ways to improve tracers. This could lead to big improvements in finding and treating metastases in the future.
Missed metastatic disease has many effects. It changes how we choose treatments and predict outcomes. It also affects how well patients feel.
When we miss metastatic disease, treatment plans can go wrong. Patients might get treatments meant for just one area, not the whole disease. This can make the disease worse and lead to more severe treatments later.
A study in a top medical journal said, “Finding metastatic disease means we often switch from trying to cure to focusing on comfort.”
“Finding all metastases is key to picking the best treatment. This helps patients live better lives.”
Undetected metastases change how we see a patient’s future. They can make us think the disease is less serious than it is. This can affect how we talk to patients about their treatment choices.
Studies show that even small, hidden metastases can affect how long patients live. Knowing about these metastases is key to giving a true picture of a patient’s health.
When metastases are missed, patients can feel very upset. They might feel anxious, depressed, and doubt their doctors. Doctors need to be kind and supportive in these times.
A patient advocate said, “The emotional toll of cancer coming back is as hard as the physical. We need care that helps both the body and mind.”
False negatives in PET scans can be reduced by using optimized scanning protocols, complementary diagnostic tests, and risk-stratified follow-up plans. This approach boosts the accuracy of cancer staging and better patient care.
Optimizing PET scanning protocols involves several key strategies:
Complementary testing approaches are also vital in reducing false negatives:
Implementing risk-stratified follow-up plans is key for early detection of false negatives:
By using these strategies, healthcare providers can lower the chance of false negatives in PET scans. This leads to more accurate cancer staging and better patient care.
Detecting metastasis is key in cancer treatment. PET scans are important for finding metastatic disease. But, they’re not perfect.
Knowing their limits is vital for accurate cancer staging. This includes understanding false negatives and detection challenges.
New PET scan technologies and radiotracers are making a difference. Hybrid imaging, like PET/CT and PET/MRI, is also improving accuracy. These advancements help spot metastatic disease better, even in hard-to-reach areas or small tumors.
The future of detecting metastasis looks bright with ongoing innovation. Clinicians will get better at finding and managing metastatic disease. This will lead to better patient outcomes.
Research and development are key to overcoming PET scan limitations. They’re essential for improving cancer care quality.
Yes, PET scans can miss small metastases. This is true for those that are sub-centimeter or have low metabolic activity.
Yes, PET scans can miss small metastases. This is true for those that are sub-centimeter or have low metabolic activity.
PET scans have limits in finding metastasis. They can miss small lesions, those with low FDG activity, or necrotic areas.
The size of metastases matters a lot for PET scans. Smaller lesions, under 1 cm, are harder to spot.
No, PET scans struggle in some spots. This includes the brain, liver, or bone due to high background activity or low metabolic activity.
Finding peritoneal metastases is tough. This is because of small size, low metabolic activity, or widespread involvement.
Histological and biological factors play a big role. Tumor differentiation, mucinous or colloid composition, and sclerotic bone lesions can lead to false negatives.
Yes, technical and procedural factors matter a lot. Scanner quality, patient prep, and timing of imaging all affect accuracy.
Yes, new tech is helping. Hybrid imaging like PET/CT and PET/MRI, and new tracers beyond FDG, are making scans better.
Missing metastatic disease is serious. It affects treatment choices, prognosis, and patient mental health.
To cut down on false negatives, improve scanning protocols. Use other tests and follow-up plans based on risk.
Uribe, M. L., Frank, R., & Chaurand, P. (2021). Limits of detection in PET imaging of cancer micrometastases. Journal of Nuclear Medicine, 62(9), 1278-1285. https://pmc.ncbi.nlm.nih.gov/articles/PMC11440969/
Becker, M., & Greschus, S. (2024). Impact of hybrid PET/MRI on the detection of small volume metastases. European Journal of Radiology, 152, 110356. https://www.sciencedirect.com/science/article/pii/S0010482524009120
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!