Last Updated on November 27, 2025 by Bilal Hasdemir
People with sickle cell disease face a higher risk of getting infections. These infections are often caused by bacteria that have a protective coating. This is a big worry because infections can cause serious problems and affect their daily lives.
It’s important to understand how sickle cell disease and infections are connected. This knowledge helps doctors and healthcare teams give better care. They can then work on preventing, diagnosing, and treating infections more effectively.

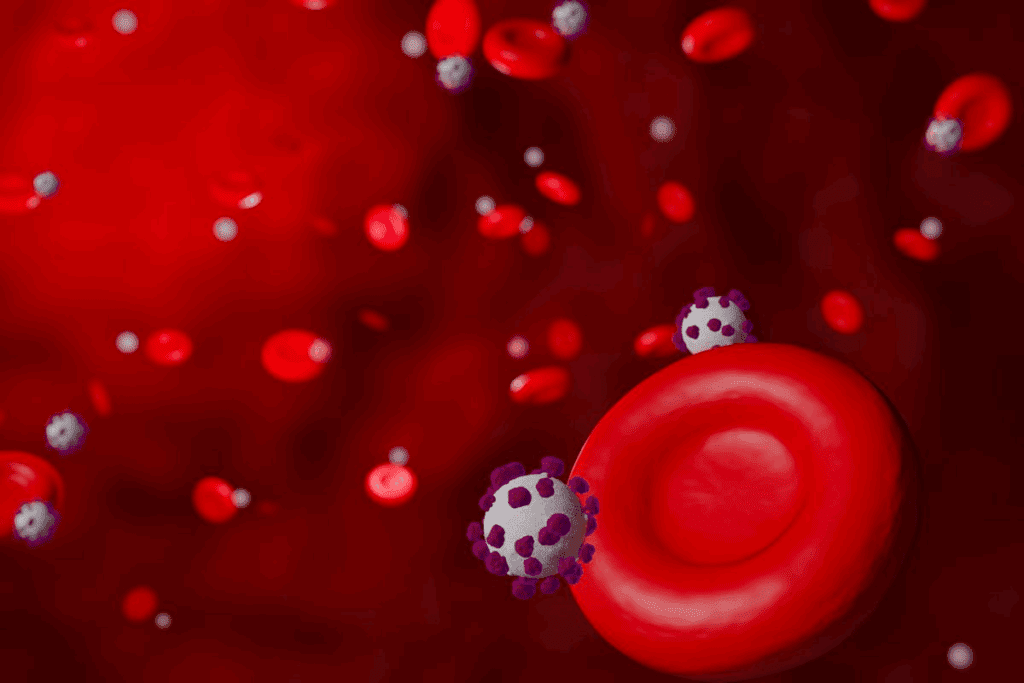
Sickle cell disease is a genetic disorder affecting hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen. It’s important for our bodies to function well.
Sickle Cell Disease is caused by abnormal hemoglobin, called sickle hemoglobin or hemoglobin S. This abnormal hemoglobin makes red blood cells sickle-shaped. This shape causes health problems.
Symptoms vary but often include pain crises. These crises happen when sickled red blood cells block blood vessels. Other symptoms include anemia, infections, and organ damage. The severity and frequency of symptoms differ among people.
The disease is caused by a mutation in the HBB gene. This mutation leads to hemoglobin S production. It’s inherited in an autosomal recessive pattern, meaning two defective genes are needed to have the disease.
Carriers have one normal and one defective gene. They don’t show all symptoms but can pass the mutated gene to their children. Knowing the genetic basis helps understand how the disease is passed down.
In the United States, Sickle Cell Disease affects many, mainly those of African descent. The CDC says it occurs in about 1 in 500 African American births. It also affects 1 in 36,000 Hispanic American births.
The disease’s incidence is linked to the sickle cell trait’s prevalence. Understanding this helps in developing better public health strategies and improving care for patients.
Sickle cell disease weakens the immune system, making it harder for the body to fight off infections. This is because the disease harms the spleen. The spleen is key for filtering blood and storing lymphocytes.
The spleen often gets damaged in people with sickle cell disease. This happens because of vaso-occlusive crises. These crises make it tough for the body to fight off infections, like those from Streptococcus pneumoniae.
The immune system’s problems in sickle cell disease are complex. They affect both the innate and adaptive immune responses. This makes it harder for the body to fight off infections, making it important to prevent them.
People with sickle cell disease are at a higher risk of getting infections. These infections can lead to more serious problems, like vaso-occlusive crises. This shows why it’s so important to prevent infections.
Vaccinations are key in preventing infections in sickle cell disease. Healthcare providers can use vaccines to protect these patients. They do this by understanding the specific risks and vulnerabilities of sickle cell disease.
Vaccines are very important in managing sickle cell disease. They help protect against serious infections. It’s vital to follow the recommended vaccination schedule, including for pneumococcal, meningococcal, and influenza infections.
By keeping up with vaccinations, people with sickle cell disease can lower their risk of serious infections. This is part of a bigger care plan that includes regular check-ups and follow-up care.
People with sickle cell disease face a higher risk of certain bacterial infections. These infections can lead to serious problems like pneumonia, osteomyelitis, and sepsis. These conditions are very dangerous and can be life-threatening if not treated right away.
We will look at three main bacterial infections that sickle cell patients often get: Streptococcus pneumoniae, Salmonella infections, and Staphylococcus aureus. Knowing about these infections is key to finding good treatments.
Streptococcus pneumoniae is a big problem for sickle cell patients, causing pneumonia and other serious infections. This bacterium is dangerous because it has a protective coating. Vaccination against pneumococcus is very important for these patients.
Salmonella infections are also a big worry for sickle cell disease patients. These infections can lead to osteomyelitis, a bone infection that’s hard to treat. Sick cell patients are much more likely to get Salmonella osteomyelitis than others, so they need careful watching and quick treatment.
Staphylococcus aureus can cause a variety of infections, from mild skin problems to severe sepsis. Sick cell patients are more likely to get S. aureus infections, mainly if they have skin problems like ulcers.
“The management of bacterial infections in sickle cell disease requires a complete approach, including preventive steps, quick diagnosis, and effective treatment.”
By knowing the risks and taking steps to prevent them, we can lessen the impact of these infections on sickle cell patients. This includes keeping up with vaccinations and practicing good hygiene to lower the chance of getting sick.
We look into how sickle cell disease makes people more likely to get infections. Knowing these reasons is key to finding ways to stop and treat infections.
Vasocclusive crises are a big problem in sickle cell disease. They happen when sickled red blood cells block blood vessels. This causes pain and makes it easier for infections to start.
Key factors that contribute to increased infection risk during vasocclusive crises include:
The sickle cell trait is usually harmless but can raise infection risks in some cases. People with this trait might face more oxidative stress and inflammation. This can affect how well their immune system works.
It’s important to remember that the sickle cell trait is not the same as sickle cell disease. Its effect on infection risk is being studied.
Chronic inflammation is a big problem in sickle cell disease. It happens because of the sickling of red blood cells and the damage it causes. This inflammation weakens the immune system, making it harder for the body to fight off infections.
The relationship between chronic inflammation and weakened immunity is complex. It involves many pathways and cytokines. Understanding this is key to finding new treatments to lower infection risks in sickle cell disease patients.
By understanding why sickle cell disease increases infection risks, we can work on better ways to prevent and manage these problems. This will help improve the lives of those with sickle cell disease.
Sickle Cell Disease patients face a higher risk of infections. It’s vital to prevent them. We’ll look at key strategies to help lower this risk.
Prophylactic antibiotics are key in preventing infections for Sickle Cell Disease patients. Penicillin is often given to kids to stop Streptococcus pneumoniae infections. This has greatly reduced severe infections in this group.
| Antibiotic | Dosage | Age Group |
| Penicillin V | 125 mg twice daily | Children under 3 years |
| Penicillin V | 250 mg twice daily | Children over 3 years |
Vaccines are also vital in preventing infections for Sickle Cell Disease patients. We suggest getting all routine vaccines and extra ones against pneumococcal disease and influenza. The pneumococcal conjugate vaccine (PCV) and pneumococcal polysaccharide vaccine (PPSV) are very important.
Good hygiene is key to avoiding infections. We tell patients to wash their hands often, after using the bathroom and before eating. Staying away from sick people also helps prevent infections.
By using these prevention strategies, we can greatly lower the risk of infections in Sickle Cell Disease patients. This improves their health and quality of life.
Managing infections in sickle cell disease needs a mix of treatments. We will look at antibiotic treatments, hydroxyurea therapy, and blood transfusions.
Antibiotics are key in fighting bacterial infections in sickle cell disease patients. Penicillin prophylaxis is often used to prevent infections, mainly in kids. Following established antibiotic protocols is important for effective treatment.
Hydroxyurea therapy can lower the number of pain crises in sickle cell disease patients. It may also lower infection risk by reducing transfusion needs and improving health. Hydroxyurea is a valuable part of care.
“Hydroxyurea is a well-tolerated medication that can significantly reduce the frequency of painful crises and may reduce the risk of infections in patients with sickle cell disease.”
Blood transfusions help improve oxygen delivery to tissues and lower complication risks in sickle cell disease. Regular transfusions manage chronic anemia and lower infection risks. We consider blood transfusions in each patient’s care plan.
In conclusion, a treatment plan that includes antibiotics, hydroxyurea, and blood transfusions can manage infections in sickle cell disease. Personalized care and ongoing monitoring are key to the best patient outcomes.
Infections can have serious long-term effects on sickle cell patients. They can cause chronic organ damage, psychological issues, and lower quality of life. It’s important for healthcare providers to keep a close eye on these patients to prevent and manage these issues.
Infections can harm organs in sickle cell patients. For example, repeated infections can damage the kidneys due to inflammation and direct harm from pathogens. Lung disease is also common, as infections like pneumonia can cause long-term respiratory problems and reduce lung function.
A study in a medical journal found that sickle cell patients face a higher risk of acute chest syndrome. This condition, often caused by infections, can harm the lungs over time.
“The management of infections in sickle cell disease is critical to preventing long-term organ damage and improving patient outcomes.”
Frequent infections can also affect sickle cell patients’ mental health. Chronic illness and repeated hospital stays can lead to anxiety and depression. This can harm their mental well-being and overall quality of life. The stress of dealing with infections can also strain family relationships.
Continuous monitoring is key to managing infections in sickle cell patients. Regular check-ups and quick treatment of infections can prevent complications. Healthcare providers should work with patients to create a care plan. This plan should include vaccination schedules, prophylactic antibiotics, and lifestyle modifications to lower infection risk.
By understanding the long-term effects of infections and using effective management strategies, we can improve patient outcomes. This can also enhance their quality of life.
The field of sickle cell care is changing fast. New research and medical tech are leading the way. We’re learning more about sickle cell disease every day. This knowledge is helping us find new treatments to help patients.
Scientists are looking into new treatments for sickle cell disease. They want to find ways to lessen painful crises and other problems. They’re focusing on treatments that get to the heart of the disease.
Some new treatments include:
These treatments are being tested in clinical trials. Early results look promising. For example, a study found a new medicine might help reduce painful crises in sickle cell patients.
| Therapy | Description | Potential Benefits |
| Anti-sickling agents | Reduce sickling of red blood cells | Decrease frequency of painful crises |
| Anti-inflammatory therapies | Manage chronic inflammation | Reduce organ damage |
| Gene editing technologies | Correct genetic defect | Potential cure for sickle cell disease |
Gene therapy is a big hope for curing sickle cell disease. It aims to fix the genetic problem by changing stem cells. This way, patients can make healthy hemoglobin and avoid sickling.
Gene therapy is being tested as a cure for sickle cell disease. It’s early, but some trials show good signs.
Support and education are key in managing sickle cell disease. Knowing the latest in care can help patients and doctors. This knowledge can lead to better outcomes and fewer complications.
Support groups and educational programs offer valuable help. They create a community where people can share and learn from each other. This support is essential for those dealing with sickle cell disease.
Together, we can keep improving care for sickle cell disease. This will make a big difference in the lives of those affected.
Managing sickle cell disease well needs a full plan. This includes acting early, having a strong support group, and keeping up with new research.
Finding sickle cell disease early is key to avoiding serious problems like pneumonia. Knowing about sickle cell disease helps people choose the best treatments. This can greatly improve their life quality.
Having a support network is very important for those with sickle cell disease. This group offers emotional and practical help, making it easier to handle the disease. Learning about the disease and how to manage it is also critical.
New research and better care for sickle cell disease are on the horizon. Keeping up with the latest in sickle cell care helps people make smart choices about their health.
Sickle cell disease is a genetic disorder that affects hemoglobin production. This leads to abnormal red blood cells. It weakens the immune system, making it harder for the body to fight off infections, like those from encapsulated bacteria.
Sickle cell patients often get infections from Streptococcus pneumoniae, Salmonella, and Staphylococcus aureus. These infections can cause serious problems, such as pneumonia, bone infections, and sepsis.
To prevent infections, sickle cell patients should take antibiotics, get vaccinated, and practice good hygiene. Vaccines are key in fighting off infections from encapsulated bacteria.
Hydroxyurea helps reduce pain crises and may lower the risk of infections. It’s often used with other treatments to manage the disease.
Gene therapy might cure sickle cell disease by fixing the genetic defect. It’s experimental but could be a future treatment for the disease.
Repeated infections can damage organs like the kidneys or lungs. They can also cause mental health issues, like anxiety and depression, affecting quality of life.
Sickle cell disease is passed down through genes from parents to children. It’s not contagious and can’t be spread through contact with someone who has it.
The outlook for sickle cell disease varies. It depends on how severe the disease is and how well it’s managed. With proper care, many people with the disease can live active lives.
Yes, sickle cell patients are more at risk for pneumonia, mainly from Streptococcus pneumoniae. Getting vaccinated against pneumococcal disease can help lower this risk.
Salmonella is the main cause of osteomyelitis in sickle cell patients. Osteomyelitis is a serious bone infection that needs quick treatment to avoid lasting damage.
National Center for Biotechnology Information. Sickle Cell Disease Infection Risk and Etiology. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7044152/
National Center for Biotechnology Information. Sickle Cell Disease Patients Increased Susceptibility to Bacterial Infections. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7044152/
National Center for Biotechnology Information. Sickle Cell Disease Bacterial Infections Vulnerable Populations. Retrieved from https://pubmed.ncbi.nlm.nih.gov/39568431/
JAMA Network. Sickle Cell Disease and Infection Risk. Retrieved from https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2806289
Centers for Disease Control and Prevention. Sickle Cell Disease Increased Infection Risk Understanding the Link. Retrieved from https://www.cdc.gov/sickle-cell/data/index.html
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!