Hepatoblastoma is a rare pediatric liver cancer that affects kids. Early detection is key for effective treatment Stage 1 hepatoblastoma.
Stage1 hepatoblastoma has a localized tumor. It hasn’t spread to other parts of the body. This makes it a critical stage for treatment. We will look into the diagnosis, treatment options, and prognosis for this condition.
Understanding early-stage hepatoblastoma is vital. It helps parents and healthcare providers make informed decisions.
Key Takeaways
- Stage1 hepatoblastoma is a localized tumor.
- Early detection is critical for effective treatment.
- Treatment options vary based on the tumor’s characteristics.
- Prognosis improves with timely intervention.
- Understanding the condition is key for informed decisions.
Understanding Hepatoblastoma in Children

Hepatoblastoma is a rare liver cancer in kids. It starts in the liver and worries doctors a lot. We’ll look at what it is, how common it is, who gets it, and why.
Definition and Prevalence of Pediatric Liver Cancer
Hepatoblastoma is a cancer that comes from young liver cells. It’s very rare, making up about 1% of all cancers in kids. It happens in about 1.5 cases for every million kids under 15.
Prevalence Statistics:
| Age Group | Incidence Rate |
| 0-1 year | 1 in 100,000 |
| 1-2 years | 1.5 in 100,000 |
| 2-3 years | 1 in 100,000 |
Risk Factors and Genetic Predispositions
What causes hepatoblastoma isn’t fully known. But, some things increase the risk. These include:
- Genetic syndromes like Beckwith-Wiedemann and Familial Adenomatous Polyposis (FAP)
- Being born too small or too early
- Exposure to certain substances in the womb
Age Groups Most Commonly Affected
Hepatoblastoma mostly hits babies and toddlers. Most cases are found before kids turn 3. The average age at diagnosis is about 18 months. It’s very rare in kids over 5.
Age Distribution:
| Age at Diagnosis | Percentage of Cases |
| 0-1 year | 40% |
| 1-2 years | 30% |
| 2-3 years | 15% |
| 3+ years | 15% |
The Hepatoblastoma Staging System Explained

Staging hepatoblastoma correctly is key to making a good treatment plan. The staging system helps doctors understand how far the disease has spread. This information guides decisions on surgery and chemotherapy.
PRETEXT and POST-TEXT Classification
The PRETEXT system is a common way to stage hepatoblastoma. It looks at the tumor’s size in the liver before treatment starts. The liver is divided into four parts, and the system checks how many are affected by the tumor.
Key aspects of the PRETEXT classification include:
- Assessment of the number of liver sectors involved
- Evaluation of vascular involvement and extrahepatic spread
- Identification of possible metastatic sites
The POST-TEXT system is used after chemotherapy to see how much tumor is left. It helps plan surgery and predict how well the child will do.
COG and SIOPEL Staging Approaches
The Children’s Oncology Group (COG) and the International Childhood Liver Tumors Strategy Group (SIOPEL) have their own staging systems for hepatoblastoma.
The COG system looks at if the tumor can be removed by surgery and if it has spread. It sorts tumors into stages based on these factors.
The SIOPEL approach, using the PRETEXT classification, focuses on the pre-treatment extent of the disease. This system gives a detailed look at the tumor’s size and its relation to major blood vessels. This is important for planning treatment.
Importance of Accurate Staging for Treatment Planning
Accurate staging of hepatoblastoma is very important for several reasons:
- It helps decide the best treatment, like surgery, chemotherapy, or both.
- It gives information about what to expect, helping families and doctors.
- It helps the team caring for the child communicate better.
- It helps sort patients into different risk groups, guiding how intense treatment should be.
By accurately staging hepatoblastoma, we can tailor treatment to each child’s needs. This can improve outcomes and reduce harm from treatment.
Stage1 Hepatoblastoma: Defining Characteristics
Stage1 hepatoblastoma is a type of liver cancer that can be fully removed by surgery. It is in its early stages, which means it’s easier to treat. This stage is very important for choosing the right treatment and has a better chance of success compared to later stages.
Complete Resection with Clear Margins
A key feature of Stage1 hepatoblastoma is the ability to remove the tumor completely. This means all cancer cells are taken out, leaving no trace behind. Having clear margins is key to preventing the cancer from coming back and improving survival chances.
To remove the tumor fully, doctors use advanced imaging and careful planning. They aim to take out the tumor while keeping as much healthy liver as possible.
Tumor Confined to Liver Segments
In Stage1 hepatoblastoma, the tumor stays within one or more liver segments. This makes it easier to remove surgically. When the tumor is in specific liver areas, doctors can plan and perform the surgery more easily.
The liver’s structure allows for removing certain segments without harming the rest. This is very important for kids, as their livers can grow back quickly.
Absence of Metastasis or Vascular Invasion
Another key feature of Stage1 hepatoblastoma is that it hasn’t spread to other parts of the body. There’s no sign of cancer cells in the blood vessels. This is a good sign and helps doctors focus their treatment.
- The cancer is localized, making it more treatable.
- There is no evidence of the cancer having spread to other organs.
- Vascular invasion, which can complicate treatment, is not present.
Knowing these characteristics is vital for creating a good treatment plan. By understanding Stage1 hepatoblastoma, doctors can give patients the best care possible.
Early Signs and Symptoms of Stage1 Hepatoblastoma
It’s important to know the early signs of Stage 1 Hepatoblastoma for quick medical help. Spotting these signs early can greatly improve treatment results.
Abdominal Distension and Mass
Abdominal distension and a palpable mass are common signs of Stage 1 Hepatoblastoma. The tumor in the liver makes the abdomen swell. Parents or caregivers might see a bigger abdomen or feel a hard mass.
Key characteristics of abdominal distension and mass include:
- Painless swelling of the abdomen
- A hard, firm mass upon palpation
- Possible discomfort or feeling of fullness
Changes in Appetite and Weight
Children with Stage 1 Hepatoblastoma might eat less and lose weight. The tumor can make them feel full or uncomfortable. This can lead to not gaining weight as they should.
Monitoring these changes is key. If a child’s appetite or weight changes, see a doctor right away.
Laboratory Abnormalities
Laboratory tests are vital for diagnosing Stage 1 Hepatoblastoma. Blood tests can show high alpha-fetoprotein (AFP) levels, which mean a liver tumor. Liver function tests might also show abnormalities.
Laboratory abnormalities associated with Stage 1 Hepatoblastoma may include:
- Elevated AFP levels
- Abnormal liver enzymes
- Other nonspecific changes in blood chemistry
Knowing these early signs is important. It helps parents, caregivers, and doctors work together for early diagnosis and treatment.
Diagnostic Approaches for Early-Stage Liver Tumors
Finding liver tumors early is key to better treatment results. We use many methods to spot them early. This is vital for managing and treating them well.
Ultrasound and Initial Imaging
Ultrasound is often the first tool used to find liver tumors. It’s easy, available everywhere, and gives important info about the tumor’s size and where it is. Ultrasound technology has gotten better, giving clear images to help understand the tumor.
CT and MRI for Precise Staging
CT (Computed Tomography) and MRI (Magnetic Resonance Imaging) are used for detailed tumor staging. They show the liver in cross-section, helping to see how big the tumor is and if it has spread. CT scans are great for finding calcium in tumors, while MRI shows soft tissues better.
CT and MRI are key for planning surgery and checking how well treatments work. They help see how the tumor relates to blood vessels and other important parts, which is important for surgery planning.
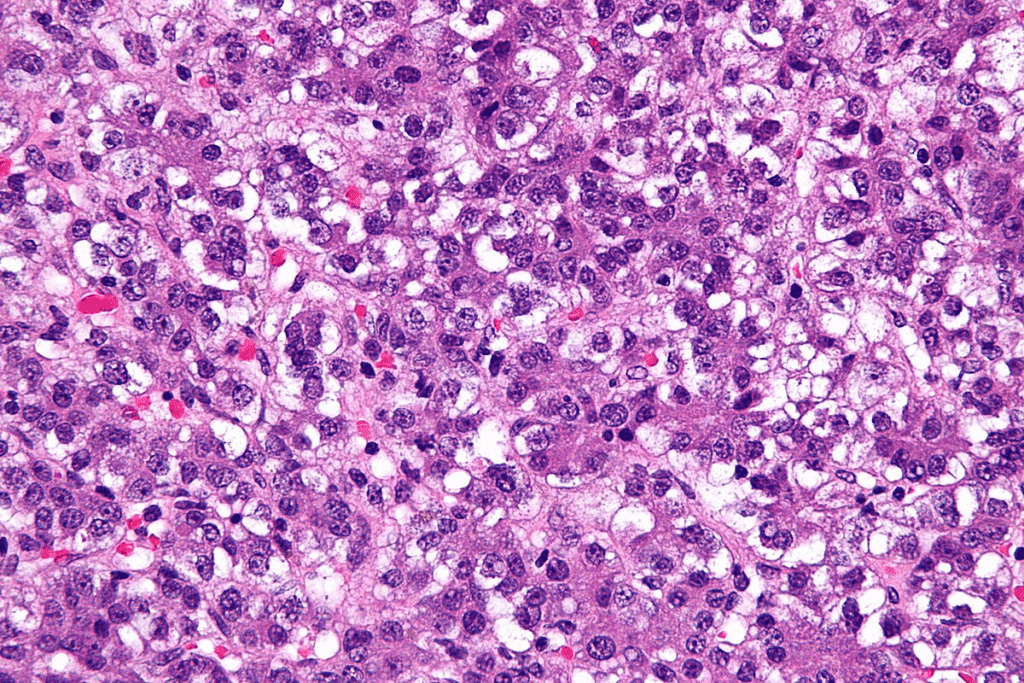
Biopsy Techniques and Considerations
Biopsy is the best way to confirm liver tumor diagnosis, by looking at tissue samples. There are many biopsy methods, like needle, laparoscopic, and surgical biopsies. The choice depends on the tumor’s location, size, and the patient’s health.
Biopsy techniques are chosen to get enough tissue for diagnosis safely. The tissue exam confirms the diagnosis and helps decide the best treatment.
Treatment Options for Stage1 Hepatoblastoma
Managing Stage1 hepatoblastoma needs a detailed plan. It must consider the tumor’s unique traits and the child’s health. The treatment usually includes surgery, chemotherapy, and sometimes liver transplant.
Surgical Resection as Primary Treatment
Surgery is often the first step in treating Stage1 hepatoblastoma. The goal is to remove the tumor completely. Complete surgical resection is key for a good outcome. Surgeons use advanced imaging to plan the surgery carefully.
Adjuvant Chemotherapy Protocols
After surgery, adjuvant chemotherapy may be needed. It helps kill any cancer cells left behind. The chemotherapy plan is made based on the child’s risk and tumor details. Common drugs include cisplatin, vincristine, and 5-fluorouracil.
Liver Transplantation Considerations
If the tumor can’t be removed by surgery, a liver transplantation might be considered. This option is for children who can’t have regular surgery. The decision to transplant involves looking at the child’s health and the risks and benefits.
Combining these treatments helps improve outcomes for children with Stage1 hepatoblastoma. It leads to high survival rates and fewer side effects.
Survival Rates and Prognosis for Localized Hepatoblastoma
Localized hepatoblastoma, like Stage 1, shows good survival rates thanks to early treatment. Knowing the prognosis helps patients and their families deal with this tough diagnosis.
Five-Year Survival Statistics
The five-year survival rate for hepatoblastoma has gone up a lot. Studies show kids with Stage 1 have a much better survival rate than those with later stages. “The overall survival rate for children with hepatoblastoma has increased to over 80% in recent years,” a leading pediatric oncology research group notes.
Prognostic Factors Specific to Stage1
Several factors are important for Stage 1 hepatoblastoma patients. These include how well the surgery went, if there’s no spread, and the tumor’s type. Early detection is vital for a better chance of recovery.
- Complete surgical resection with clear margins
- Absence of vascular invasion or metastasis
- Favorable histological features
Long-term Outcomes and Quality of Life
Children with Stage 1 hepatoblastoma often have a good quality of life after treatment. But, they need to be watched closely for any late effects. A study found, “Long-term survivors of hepatoblastoma require thorough follow-up care to handle treatment-related issues.”
It’s key to have a team approach to care. This ensures patients get all the support they need during and after treatment.
Post-Treatment Monitoring and Follow-up Care
The journey doesn’t end with treatment; patients with Stage 1 Hepatoblastoma need ongoing monitoring and follow-up care. We know that finishing treatment is a big step. But it’s just as important to keep up with a follow-up care plan. This plan includes regular check-ups, watching for recurrence through alpha-fetoprotein (AFP) levels, and handling any side effects from treatment.
Surveillance Imaging Schedules
Surveillance imaging is key in post-treatment care. We suggest a schedule with regular ultrasounds, CT scans, or MRIs. The timing of these tests depends on the patient’s risk factors and how well they’ve responded to treatment. Usually, tests are more often in the first year and then less often over time.
| Time After Treatment | Imaging Frequency | Type of Imaging |
| 0-12 months | Every 3 months | Ultrasound, CT, or MRI |
| 1-2 years | Every 4-6 months | Ultrasound, CT, or MRI |
| 2-5 years | Every 6-12 months | Ultrasound, MRI |
AFP Monitoring for Recurrence
AFP monitoring is vital in follow-up care. High AFP levels can mean the cancer is coming back, even before symptoms or tumors show up. We check AFP levels often, at the same time as imaging tests. This helps us catch any signs of cancer coming back quickly.
Managing Treatment-Related Effects
Treatment for Stage 1 Hepatoblastoma can have lasting effects. These can include liver issues, hearing loss from some chemo drugs, and other side effects. We help patients manage these effects, which might mean more treatments, lifestyle changes, or ongoing checks. Our aim is to lessen these effects and improve the patient’s quality of life.
Recent Advances in Stage1 Hepatoblastoma Management
Stage1 hepatoblastoma treatment has made big strides in recent years. These changes have improved patient outcomes and quality of life. They cover all stages of care, from diagnosis to follow-up.
There’s a big change in how we treat Stage1 hepatoblastoma. This change comes from new research and clinical trials. It’s making patient care better.
Targeted Therapies and Clinical Trials
Targeted therapies are a key area of progress. They aim to hit cancer cells directly, sparing healthy tissues. Ongoing clinical trials are checking if these treatments work well in kids with Stage1 hepatoblastoma.
Clinical trials are very important. They give us the data we need to improve treatments. They also let patients try new, promising therapies.
Improvements in Surgical Techniques
Surgery is a big part of treating Stage1 hepatoblastoma. New surgical techniques, like minimally invasive surgery, are making things better. These methods help patients heal faster and leave less scar tissue.
Also, better imaging and planning before surgery are helping. This means surgeons can do their jobs more accurately, leading to better results for patients.
Risk-Adapted Treatment Approaches
Using risk-adapted treatment approaches is another big step forward. This method tailors treatment based on how high a patient’s risk is. It makes sure patients get the right care without getting too much of the bad stuff.
By sorting patients by risk, we can make treatment plans better. This could lead to higher survival rates and fewer side effects from treatment.
In short, treating Stage1 hepatoblastoma is getting better fast. We’re seeing better care thanks to targeted therapies, new surgery methods, and tailored treatments. As we keep researching, we’ll see even more progress in treating this disease.
Conclusion: Navigating a Childhood Liver Cancer Diagnosis
Getting a diagnosis of childhood liver cancer is tough for families. It needs a lot of support and care for both patients and their families. Stage1 hepatoblastoma requires knowing its details, treatment options, and what to expect.
We’ve looked at how important accurate staging and treatment are. Knowing about surgery and chemotherapy helps families make good choices for their child. Keeping up with new treatments and trials is key.
Dealing with a childhood liver cancer diagnosis is more than just medical stuff. It’s also about handling the emotional and practical sides. A strong support network is vital. Working with healthcare teams helps ensure the best care for the child, boosting their chances of a good outcome.
FAQ
What is Stage1 hepatoblastoma?
Stage1 hepatoblastoma is an early-stage liver cancer in kids. It’s found in the liver and can be removed completely.
What are the risk factors for developing hepatoblastoma?
Certain genetic conditions like Beckwith-Wiedemann syndrome increase the risk. Low birth weight also plays a role.
How is hepatoblastoma staged?
Doctors use PRETEXT and POST-TEXT systems to check the tumor’s size in the liver. They also look at COG and SIOPEL stages for more details.
What are the symptoms of Stage1 hepatoblastoma?
Symptoms include a big belly, a mass in the belly, and changes in appetite. Weight loss and high alpha-fetoprotein (AFP) levels are also signs.
How is Stage1 hepatoblastoma diagnosed?
Doctors use ultrasound, CT, and MRI scans to see the tumor. A biopsy confirms the diagnosis.
What are the treatment options for Stage1 hepatoblastoma?
Treatment includes surgery to remove the tumor. Chemotherapy is used to prevent it from coming back. Sometimes, a liver transplant is needed.
What is the prognosis for Stage1 hepatoblastoma?
The outlook is good, with high survival rates. This is true when the tumor is removed completely.
How is post-treatment monitoring done for Stage1 hepatoblastoma?
Monitoring includes regular scans and checking AFP levels. This helps catch any signs of the cancer coming back early.
What are the recent advances in the management of Stage1 hepatoblastoma?
New treatments like targeted therapies are helping. Better surgery techniques and tailored treatment plans are also improving outcomes.
What support is available for families dealing with a childhood liver cancer diagnosis?
Families get a lot of support. This includes emotional help, practical aid, and guidance during treatment.



































