
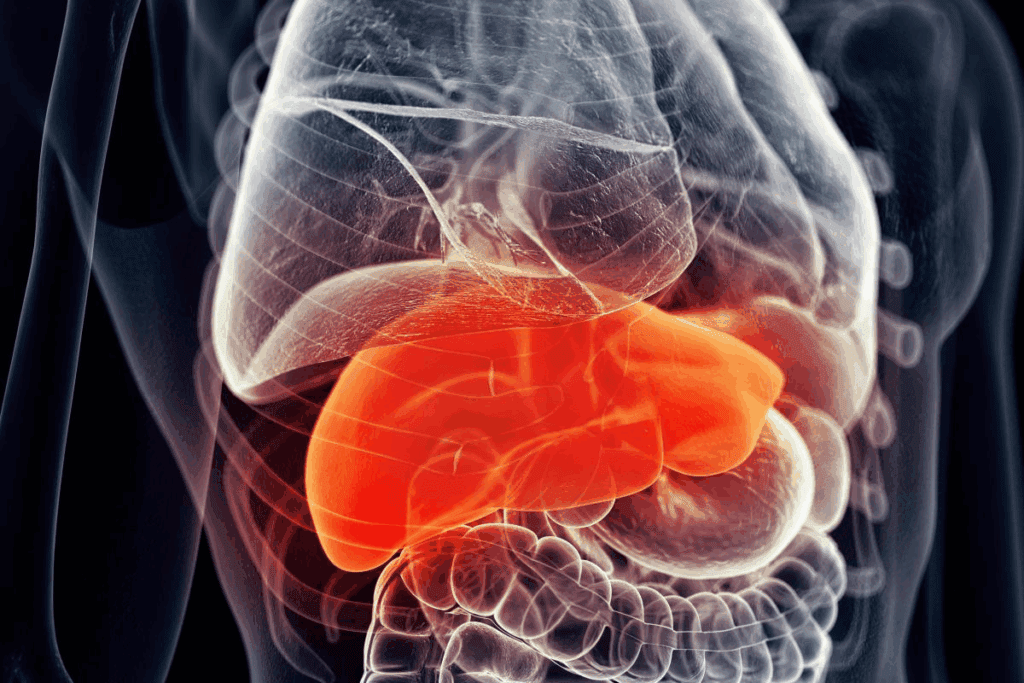
Diagnosing liver cancer in children needs a good understanding of its looks. Hepatoblastoma is a rare liver cancer that mostly hits kids under three.
Spotting the tumor characteristics is key for correct diagnosis and treatment plans. We look at the liver tumor features that help spot this condition.
Knowing the hepatoblastoma tumor characteristics is important for doctors to give the best care. By looking at the visual signs of this condition, we can understand its effects better. This helps in creating specific treatment plans.
Key Takeaways
- Understanding the visual characteristics of hepatoblastoma is key for diagnosis.
- Liver tumor features are important in spotting the condition.
- Pediatric liver cancer presentation varies, needing careful check-ups.
- Accurate diagnosis is vital for effective treatment planning.
- Hepatoblastoma mainly affects kids under three.
Understanding Hepatoblastoma: An Overview
To understand hepatoblastoma, we need to look at its definition, how common it is, and what increases the risk. It’s a rare and aggressive liver tumor mainly found in kids. Knowing the basics is key to spotting it early and treating it effectively.
Definition and Epidemiology
Hepatoblastoma is a rare tumor that makes up about 1% of all cancers in kids. It’s the most common liver cancer in children, often found in the first two years of life. The exact number of cases varies worldwide, but it’s considered rare.
Epidemiological studies show that more boys get it, and it’s most common in kids under three. Its rarity and age make it hard to diagnose and treat. Knowing this helps doctors create better screening and treatment plans.
Risk Factors and Etiology
The exact cause of hepatoblastoma is not known, but some genetic syndromes and conditions raise the risk. For example, Beckwith-Wiedemann syndrome, Familial Adenomatous Polyposis (FAP), and Low Birth Weight are linked to it. We’ll look into these risk factors and what they mean for the disease’s cause.
The causes of hepatoblastoma are complex, involving genetics and possibly the environment. Research has found genetic links to its development. Knowing these factors helps in finding ways to prevent and treat the disease.
Hepatoblastoma Appearance: Macroscopic Features
Knowing the macroscopic features of hepatoblastoma is key for diagnosis and treatment. The gross pathological characteristics tell us a lot about the tumor’s nature and how it might behave.
Gross Pathological Characteristics
Hepatoblastoma usually shows up as a big, clear mass in the liver. It can feel soft or firm and look variegated because of hemorrhage, necrosis, or calcification. A study in a top medical journal says, “The gross appearance of hepatoblastoma can vary a lot, showing its complex histological nature.”
“The gross appearance of hepatoblastoma can vary significantly, reflecting its complex histological nature.”
The cut surface of the tumor often has a mix of colors, like tan, yellow, or green, due to bile production. The tumor’s edge can be well-circumscribed or infiltrative, which affects how easy it is to remove.
Tumor Size and Shape Variations
Hepatoblastoma can be a single large mass or multiple smaller nodules. Its size can range from a few centimeters to a big mass that takes up most of the liver. The shape can be round, oval, or irregular, based on where it grows and how it spreads.
The differences in size and shape are important for diagnosis and treatment. Bigger tumors might need more aggressive treatments, like neoadjuvant chemotherapy and surgery.
- Tumor size and shape affect treatment choices.
- Bigger tumors might need neoadjuvant chemotherapy.
- Surgery is often needed to remove the tumor.
By understanding the macroscopic features of hepatoblastoma, doctors can better diagnose and manage this complex tumor.
Histological Appearance of Hepatoblastoma
Knowing how hepatoblastoma looks under a microscope is key for the right diagnosis and treatment. This tumor has many different looks, which help doctors classify and treat it.
Hepatoblastoma’s look can be split into several types, mainly based on the cells found in the tumor.
Epithelial Subtypes
Epithelial types of hepatoblastoma have cells that look like those in an embryo’s liver. These types are split based on how much the cells look like normal liver cells.
Fetal subtype has cells that look very much like normal fetal liver cells. They have a uniform look and show little abnormality.
Embryonal subtype has cells that are more like the very early stages of liver development. These cells show a higher ratio of nucleus to cytoplasm, indicating a more aggressive tumor.
Mixed Epithelial and Mesenchymal Subtypes
Mixed types of hepatoblastoma have both epithelial and mesenchymal parts. The mesenchymal parts can include undifferentiated spindle cells, osteoid, or cartilaginous tissue.
Diagnosing mixed types can be tricky. It often requires a close look at the cells and sometimes extra tests.
Knowing about these subtypes is vital for creating effective treatment plans and better patient care.
Clinical Presentation of Pediatric Liver Tumors
Pediatric liver tumors, like hepatoblastoma, show symptoms that are not always clear. It’s important for doctors to know about these signs. This helps them find the right treatment for each child.
Physical Examination Findings
Children with hepatoblastoma might have a big belly. This is because the tumor is growing inside. They might also lose weight, feel tired, or not want to eat.
Key physical examination findings may include:
- Abdominal distension or swelling
- Palpable abdominal mass
- Weight loss or failure to thrive
- Fatigue or lethargy
Laboratory Markers and Their Correlation with Tumor Appearance
Laboratory tests are key in finding and treating hepatoblastoma. Alpha-fetoprotein (AFP) is a big marker for this tumor. When AFP levels go up, it often means the tumor is there.
The link between AFP levels and tumor details is being studied. Research shows that high AFP levels might mean the tumor is bigger or has certain types. Watching AFP levels helps see how well treatment is working.
Knowing how to spot hepatoblastoma symptoms and markers is vital. This helps doctors find and treat the tumor early. It also helps kids with this rare liver cancer get better faster.
Ultrasound Appearance of Hepatoblastoma
The ultrasound appearance of hepatoblastoma can vary a lot. It’s key to know its typical features. Ultrasound helps a lot in checking hepatoblastoma, giving important info about the tumor.
Echogenicity Patterns and Texture
Hepatoblastoma can show different echogenicity patterns on ultrasound. Some tumors look hyperechoic, while others are hypoechoic or isoechoic compared to the liver. The texture can also change, with some tumors looking uniform and others showing spots of necrosis, hemorrhage, or calcification.
- Hyperechoic areas might mean the tumor has dense cells or calcifications.
- Hypoechoic spots could point to necrosis or cystic changes.
- Isoechoic tumors might blend in with the liver, making them harder to spot.
Doppler Flow Characteristics
Doppler ultrasound is key for checking the blood flow in hepatoblastoma. Tumors often have more blood flow, which Doppler imaging can show. The blood flow details help figure out how aggressive the tumor is and guide treatment plans.
- Tumors with lots of blood flow might need more intense treatment.
- Doppler ultrasound can spot vascular invasion, which is important for staging.
- Arteriovenous shunts in the tumor can be found with Doppler flow analysis.
Knowing how hepatoblastoma looks on ultrasound is very important. It helps doctors diagnose and plan treatment better. By using these ultrasound signs, doctors can make better choices for patient care.
CT Scan Features of Hepatoblastoma
CT imaging is key for checking hepatoblastoma. It shows the tumor’s size, where it is, and its density. We use CT scans to get clear images for diagnosing and figuring out the stage of this liver tumor.
Pre-contrast Appearance
Before contrast, hepatoblastoma looks like a well-defined mass on CT scans. Its density can be lower, the same, or higher than the liver around it.
Post-contrast Enhancement Patterns
After contrast, hepatoblastoma shows different enhancement patterns. This depends on the tumor’s makeup and blood flow.
Some tumors might show up early in the arterial phase. Others might appear later in the portal venous or delayed phase images.
Tumor Density Characteristics
The density of hepatoblastoma on CT scans tells us about its makeup. High-density tumors might have calcifications or hemorrhage.
| CT Feature | Description | Clinical Significance |
| Pre-contrast Attenuation | Varies from hypoattenuating to hyperattenuating | Indicates tumor composition |
| Post-contrast Enhancement | Heterogeneous enhancement | Reflects tumor vascularity and composition |
| Tumor Density | Can be low, iso, or high density | May indicate calcifications, hemorrhage, or necrosis |
MRI Features of Hepatoblastoma
MRI is key in diagnosing hepatoblastoma. It gives us detailed images needed for treatment plans. We use MRI to understand the tumor’s features, which is vital for effective treatment.
T1-Weighted Imaging Characteristics
On T1-weighted images, hepatoblastoma looks like a mixed mass. The tumor is usually darker than the liver around it. This helps us see where the tumor starts and ends.
The tumor’s look can change based on hemorrhage, necrosis, or calcifications.
T2-Weighted Imaging Characteristics
T2-weighted images show us more about the tumor and its surroundings. Hepatoblastoma is very bright on these images, standing out against the liver. This brightness comes from the tumor’s water content and possible necrosis or cysts.
Contrast Enhancement Patterns
Contrast agents make MRI better for seeing the tumor’s blood flow and how it reacts to the contrast. The tumor’s enhancement is not even. Some parts show up very bright, while others are darker. This tells us about the tumor’s health and how it might respond to treatment.
By looking at T1, T2, and contrast-enhanced images together, we get a full picture of the tumor. This detailed view is essential for accurate diagnosis, staging, and treatment planning. It helps improve patient care.
Solid and Cystic Components in Hepatoblastoma
Understanding hepatoblastoma’s makeup is key for diagnosis and treatment. It can be purely solid or mixed solid-cystic. This liver cancer in kids shows different types that matter for diagnosis and care.
Pure Solid Tumor Characteristics
Pure solid hepatoblastomas look the same everywhere, without cysts. They appear dense and uniform on scans.
These solid tumors can be hard to tell apart from other liver issues.
Mixed Solid-Cystic Lesions
Mixed solid-cystic hepatoblastomas have both solid and cystic parts. The cysts can be different sizes and may have necrotic debris or fluid.
The mix of solid and cystic parts helps doctors diagnose. The ratio of solid to cystic parts affects how the tumor acts and how it responds to treatment.
The different types of hepatoblastoma highlight the need for detailed imaging. Advanced imaging is vital for spotting the various parts of these tumors.
Vascular Features of Hepatoblastoma
Understanding the vascular features of hepatoblastoma is key for effective management. The vascular characteristics of this tumor greatly affect its diagnosis, treatment, and prognosis.
Tumor Vascularity on Diagnostic Scans
Tumor vascularity is about the blood vessels in the tumor. On scans, hepatoblastoma often shows more vascularity. This can help doctors tell it apart from other tumors.
Vascular Invasion Patterns
Vascular invasion means the tumor can grow into nearby blood vessels. This can happen in hepatic veins, portal veins, or other major vessels.
| Imaging Technique | Vascularity Assessment | Vascular Invasion Detection |
| Ultrasound | Can assess blood flow and vascularity | Limited ability to detect vascular invasion |
| CT Scan | Can evaluate tumor vascularity with contrast | Can detect vascular invasion into major vessels |
| MRI | Provides detailed assessment of tumor vascularity | Can detect vascular invasion with high sensitivity |
The vascular features of hepatoblastoma are vital for diagnosis and treatment. Advanced imaging techniques are essential for assessing these features.
Hepatoblastoma Growth Patterns
It’s key to know how hepatoblastoma grows to diagnose and treat it well. This cancer can show up as one big mass or as many smaller ones. How it grows affects how well a patient does.
Unifocal vs. Multifocal Presentation
Hepatoblastoma can be either unifocal or multifocal. Unifocal means there’s just one tumor. Multifocal means there are many tumors in the liver.
Knowing if it’s unifocal or multifocal helps doctors plan treatment. If it’s multifocal, it’s usually a sign of more advanced cancer. This might mean the treatment needs to be stronger.
Infiltrative vs. Well-Circumscribed Borders
Hepatoblastoma can grow in two ways: infiltrative or well-circumscribed. Infiltrative tumors spread into the liver, making surgery hard.
Well-circumscribed tumors, though, have clear edges. This makes surgery easier. The tumor’s edges are very important for how well a patient can be treated.
| Growth Pattern | Description | Clinical Implication |
| Unifocal | Single tumor mass | Easier to resect surgically |
| Multifocal | Multiple distinct tumor nodules | More challenging to treat, often requires aggressive therapy |
| Infiltrative | Tumor invades surrounding liver tissue | Difficult to resect completely |
| Well-Circumscribed | Clear boundaries | Generally easier to resect surgically |
Hepatoblastoma Staging Appearance
Getting the right stage for hepatoblastoma is key for the best treatment. The PRETEXT staging system is used for this. It looks at images to see how big the tumor is in the liver.
PRETEXT Staging System Visual Criteria
The PRETEXT system looks at the liver in four parts. It checks which parts have tumors. This helps figure out how big the disease is.
- The number of liver sectors free of tumor
- The presence of tumor in the main portal vein or its branches
- Involvement of the hepatic veins or inferior vena cava
- Presence of extrahepatic disease
These details help sort tumors into different stages. This is important for planning treatment.
Imaging Characteristics by Stage
How a tumor looks on images changes with its stage. Early tumors might look like a single mass in one liver part. But, bigger tumors can spread to more parts and even outside the liver.
PRETEXT I tumors affect just one part of the liver. As the stage goes up to PRETEXT IV, all four parts are involved. This shows the disease is more widespread.
Knowing how a tumor looks is key for accurate staging. It helps decide the best treatment, like surgery or chemotherapy.
Using the PRETEXT system helps doctors predict how well a patient will do. It lets them make treatment plans that fit each patient’s needs.
Differential Diagnosis: Similar-Appearing Liver Tumors
Several liver tumors in children can look like hepatoblastoma. This makes it important to diagnose them correctly. The right diagnosis helps choose the best treatment and improves patient outcomes.
Hepatocellular Carcinoma vs. Hepatoblastoma
Hepatocellular carcinoma (HCC) is a liver cancer that can be hard to tell apart from hepatoblastoma, mainly in older kids and teens. Both are cancers, but they differ in how they grow and behave.
Key differences:
- Age of onset: Hepatoblastoma usually happens in kids under 3, while HCC is more common in older kids and adults.
- Tumor markers: Alpha-fetoprotein (AFP) is high in both, but very high levels are more typical of hepatoblastoma.
- Imaging features: HCC often looks more mixed on scans because of dead cells and bleeding.
Mesenchymal Hamartoma vs. Hepatoblastoma
Mesenchymal hamartoma is a benign liver tumor mostly seen in young kids. It’s hard to tell apart from hepatoblastoma because they share some imaging traits.
Distinguishing characteristics:
- Cystic components: Mesenchymal hamartomas often have big cystic areas, which are less common in hepatoblastoma.
- Clinical presentation: Mesenchymal hamartomas usually cause belly swelling because of their size.
- Imaging: A well-defined, multiloculated cystic mass is more typical of mesenchymal hamartoma.
Other Pediatric Liver Masses
Other liver masses that might be confused with hepatoblastoma include:
- Focal nodular hyperplasia
- Liver adenoma
- Undifferentiated embryonal sarcoma
- Metastatic lesions
Each of these has its own signs and imaging traits that help tell them apart from hepatoblastoma. A detailed diagnostic process, including scans and tissue tests, is key for the right diagnosis and treatment.
Metastatic Hepatoblastoma Visual Findings
It’s important to know how metastatic hepatoblastoma looks to diagnose and treat it well. When it spreads, it can go to different parts of the body. Each place it goes has its own look on imaging studies.
Pulmonary Metastases Appearance
The lungs are a common place for hepatoblastoma metastasis. On scans, you can see many small nodules in the lungs. These nodules are clear and can be different sizes. On CT scans, they often show up as peripheral lesions, mostly in the lower lobes.
On chest X-rays, big metastases look like rounded opacities. But small ones might not show up. CT scans of the chest are better at finding these nodules. They give detailed info on how many, how big, and where they are.
Other Common Metastatic Sites
While the lungs are the most common place, other organs can also get affected. The abdomen is often involved, with lymph nodes, adrenal glands, and other organs inside it.
Bone metastases are less common but can happen in advanced cases. They look like lytic lesions on X-rays or CT scans, sometimes with soft tissue masses. Brain metastases are rare but can cause symptoms like increased pressure or neurological problems. On MRI, they look like well-defined, contrast-enhancing lesions.
Knowing how metastatic hepatoblastoma looks in different organs is key for full staging and treatment planning. Imaging studies like CT, MRI, and PET scans are vital for finding and understanding metastatic disease.
Hepatoblastoma Appearance After Treatment
After treatment, hepatoblastoma can look very different. This change shows how well the treatment worked. It’s key to understand these changes to plan the next steps in care.
Post-Chemotherapy Changes on Imaging
Chemotherapy is a big part of treating hepatoblastoma, mainly in kids. After treatment, scans like CT and MRI show big changes. These changes might include smaller tumors, different densities, and how the tumor looks with contrast. For example, a treated tumor might not show up as much on scans, showing it’s responding well to treatment.
Chemotherapy can also cause parts of the tumor to die. This looks like dark spots on CT scans or mixed signals on MRI. These signs mean the tumor is responding to treatment. Doctors and radiologists need to know these changes to see how well the treatment is working.
Post-Surgical Appearance
After surgery, the liver looks different on scans. The surgery can change the liver’s shape, showing where the tumor was removed and any complications. Doctors use ultrasound, CT, and MRI to check the liver after surgery.
The liver might look different after surgery, with signs like clips and changes in shape. It’s important to tell apart normal changes and any problems or tumor coming back. For example, a fluid collection could be a hematoma, seroma, or abscess, which need attention.
We must carefully look at scans after treatment to understand the changes in hepatoblastoma. This helps us decide the best care for our patients and aim for the best outcomes.
Advanced Imaging Techniques for Hepatoblastoma
Advanced imaging is key in diagnosing hepatoblastoma. Medical tech keeps getting better, helping us manage this pediatric liver cancer more effectively.
PET/CT Findings
PET/CT scans are now a big help in checking on hepatoblastoma. They mix metabolic activity from PET with CT’s body details. This helps us see how far the disease has spread.
Using PET/CT for hepatoblastoma has many advantages. It:
- Improves how we stage the disease
- Helps us see how well treatments are working
- Finds metastases better
Emerging Imaging Modalities
New imaging methods are being looked into for treating hepatoblastoma. Some of these include:
| Imaging Modality | Potential Benefits |
| Diffusion-weighted MRI | Helps us understand tumors better and see how treatments are doing |
| Contrast-enhanced ultrasound | Allows us to see tumors live without using harmful radiation |
| MR elastography | Measures liver stiffness and might spot fibrosis early |
These new tools could make diagnosing and treating hepatoblastoma even better.
Conclusion: Recognizing Hepatoblastoma’s Distinctive Imaging Features
It’s key to spot the special imaging signs of hepatoblastoma for right diagnosis and treatment. We’ve looked into how imaging helps in spotting this liver cancer. This includes its look, how it acts, and the latest imaging methods.
Knowing how to use tools like ultrasound, CT scans, and MRI is vital. These help doctors see the unique signs of hepatoblastoma. This knowledge helps in making a precise diagnosis and a treatment plan tailored for each child with liver cancer.
Liver tumor imaging is very important for diagnosing hepatoblastoma. Using the latest imaging and knowing its special signs helps in better diagnosing and treating liver cancer in kids. This leads to better health outcomes for them.
FAQ
What are the typical imaging features of hepatoblastoma?
Hepatoblastoma shows up as a big, clear mass in the liver on scans. It can be solid or have cysts. The look changes based on the type of tumor.
How does hepatoblastoma appear on ultrasound?
On ultrasound, it looks like a mixed mass with different textures. It can be solid or have cysts. Doppler shows blood flow in the tumor.
What are the characteristic CT features of hepatoblastoma?
On CT scans, it’s a clear mass that might look the same as the liver before contrast. After contrast, it shows different levels of brightness. The density is not uniform.
How does hepatoblastoma appear on MRI?
MRI shows it as a clear mass with specific T1 and T2 signals. It can enhance differently with contrast. The look is varied.
What is the significance of vascular features in hepatoblastoma?
The blood flow and invasion patterns are key. They help understand the tumor’s behavior and treatment planning.
How does hepatoblastoma staging appearance correlate with treatment?
The PRETEXT system stages hepatoblastoma. Imaging features of each stage guide treatment choices.
What are the differential diagnoses for hepatoblastoma?
Other liver tumors like hepatocellular carcinoma and mesenchymal hamartoma might look similar on scans.
How does metastatic hepatoblastoma appear on imaging?
Metastatic hepatoblastoma shows up as distinct signs on scans. This includes lung metastases and other common sites.
What changes can be expected in hepatoblastoma appearance after treatment?
After treatment, it can change on scans. This includes changes after chemotherapy and surgery. It helps see how well the treatment worked.
What is the role of advanced imaging techniques in hepatoblastoma diagnosis and management?
New imaging like PET/CT and others are key in diagnosing and managing hepatoblastoma.
What is the typical size and shape of hepatoblastoma?
It can be any size or shape but is often a big, clear mass.
Can hepatoblastoma be multifocal?
Yes, it can be in many places. Knowing how it grows is important for diagnosis and treatment.
National Center for Biotechnology Information. Hepatoblastoma tumor characteristics in pediatric diagnosis. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25019441
National Center for Biotechnology Information. Hepatoblastoma tumor characteristics aiding pediatric diagnosis. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25019441
National Center for Biotechnology Information. Hepatoblastoma tumor characteristics in pediatric diagnosis. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25019441
References
Benoist, M. (2002). The natural history of lumbar degenerative spinal stenosis: A comprehensive review. Joint Bone Spine, 69(5), 450-457. https://www.sciencedirect.com/science/article/abs/pii/S1297319X02004293



































