
Chemotherapy-induced neutropenia is a serious condition that affects many patients with cancer. It’s estimated that up to 50% of patients receiving chemotherapy may develop neutropenia, making them more likely to get infections. Essential strategies and protocols that form the comprehensive Neutropenic precautions for nurses when caring for high-risk patients.
As healthcare providers, we know neutropenic precautions are key to keeping these patients safe. Neutropenia nursing care plans help reduce the risk of infections. This ensures the safety of our patients.
Effective care strategies are essential for managing neutropenia patients. Nurses are critical in protecting their patients by understanding and applying these precautions well.
Key Takeaways
- Neutropenia is a common complication of chemotherapy.
- Nurses play a vital role in managing neutropenic patients.
- Neutropenic precautions are essential in preventing infections.
- A well-designed neutropenia nursing care plan is vital for patient safety.
- Minimizing exposure to infection sources is key to effective care.
What is Neutropenia and Its Causes?
It’s important for nurses to know about neutropenia to give the best care to patients. Neutropenia is when there are not enough neutrophils, a type of white blood cell. These cells help fight infections.
Definition of Neutropenia
Neutropenia means having less than 1,500 neutrophils per microliter of blood. It’s severe if it’s less than 500. This makes it harder for the body to fight off infections.
Common Causes of Chemotherapy-Induced Neutropenia
Chemotherapy often leads to neutropenia because it stops the bone marrow from making neutrophils. The type and amount of chemotherapy can also affect the risk. Knowing this helps nurses create a good neutropenia nursing care plan.
Some things that can cause chemotherapy-induced neutropenia include:
- The type and intensity of the chemotherapy regimen
- The dose and frequency of chemotherapy administration
- Patient-specific factors, such as age and overall health
The Role of the Immune System
The immune system is key to keeping the body safe from infections. Neutrophils are a big part of this. When there are not enough neutrophils, the body can’t fight off infections as well. This makes nursing interventions for neutropenia very important to stop and treat infections.
We need to understand how neutropenia affects the immune system and patient health. This helps us give the right care. We need to prevent infections and watch for signs of infection closely.
Importance of Neutropenic Precautions
For patients with neutropenia, taking precautions is key to avoid serious infections. Neutropenia means the body has too few neutrophils, making it hard to fight off infections. As healthcare workers, we know how vital neutropenic precautions are for keeping patients safe.
Why Precautions Are Crucial for Patient Safety
Neutropenic precautions are vital because they lower the chance of infection in those with weak immune systems. These steps include using personal protective equipment (PPE), keeping the environment clean, and following strict hygiene rules. By doing these things, we greatly cut down the risk of harmful germs reaching the patient.
| Precaution | Description | Purpose |
| Personal Protective Equipment (PPE) | Use of gloves, masks, and gowns | To prevent the transmission of pathogens from healthcare workers to patients |
| Environmental Cleaning | Regular disinfection of surfaces and equipment | To reduce the presence of pathogens in the patient’s Page environment |
| Hand Hygiene | Frequent and proper hand washing or use of hand sanitizer | To minimize the transfer of microorganisms to the patient |
The Impact of Neutropenia on Patient Health
Neutropenia can greatly affect a patient’s health, making them more likely to get severe infections. These infections can be deadly if not treated quickly. It not only harms their physical health but also their mental and emotional well-being.
It can lead to longer hospital stays, higher healthcare costs, and a lower quality of life. Knowing this shows how important neutropenic precautions are in our work.
Nursing Responsibilities in Neutropenic Care
The nursing team has many duties in neutropenic care. They assess and educate patients. Nurses are key in managing neutropenia, a condition that needs careful care to avoid infections.
Assessing Patient Risks and Needs
It’s important to assess patient risks and needs in neutropenic care. We look at each patient’s situation to spot risks. Then, we create a nursing care plan for neutropenia just for them.
- Reviewing the patient’s medical history and current condition
- Assessing the patient’s risk for infection or other complications
- Identifying the patient’s educational needs regarding their condition and care
This process helps us tailor our care to each patient. It makes their care safer and more effective.
| Assessment Criteria | Key Considerations |
| Medical History | Previous infections, allergies, and medical conditions |
| Current Condition | ANC levels, presence of fever, signs of infection |
| Educational Needs | Understanding of neutropenia, infection prevention strategies |
Educating Patients and Families on Safety Measures
Teaching patients and families about safety is key. It helps prevent infections and manage neutropenia well. We teach them about neutropenic precautions for nurses and patients. This includes:
- Proper hand hygiene techniques
- Use of personal protective equipment (PPE)
- Avoiding close contact with individuals who are sick
- Safe food handling practices
By teaching them, we help them take charge of their care. This reduces the chance of complications.
Implementing Standard Precautions for Neutropenic Patients

Caring for neutropenic patients means we must take extra steps to prevent infections. These steps are called standard precautions. They help stop the spread of germs and keep patients safe. Let’s look at what these precautions are and why they’re important in neutropenic care.
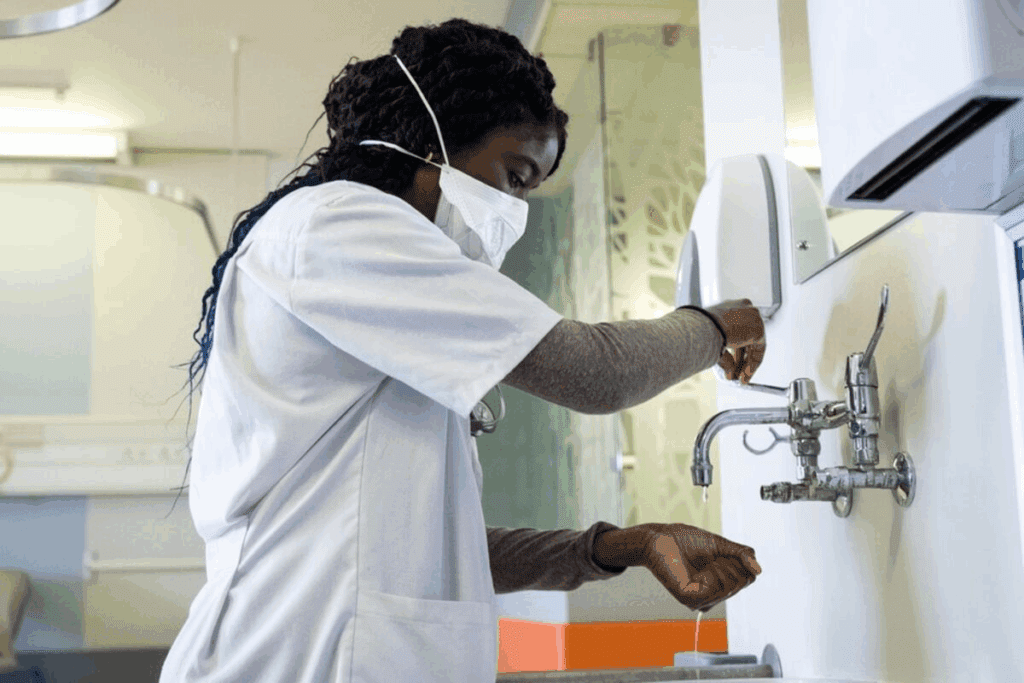
Hand Hygiene Protocols
Keeping hands clean is key to stopping infections. Effective hand hygiene is vital to lower the chance of germ spread. Everyone in the healthcare setting must follow strict hand cleaning rules.
- Alcohol-based hand rubs are a highly effective method for cleaning hands.
- Clean hands before and after touching the patient, after removing gloves, and after touching things that might be dirty.
Use of Personal Protective Equipment (PPE)
Personal Protective Equipment (PPE) is also very important. It includes gloves, gowns, masks, and eye protection. We need to teach everyone about using PPE correctly to keep everyone safe.
- Wear gloves when you might touch bodily fluids, mucous membranes, or broken skin.
- Put on gowns during procedures where you might get splashed with bodily fluids.
- Wear masks to stop airborne germs from spreading.
By following these standard precautions, we can greatly lower the risk of infections in neutropenic patients. This makes their care safer and better.
Environmental Considerations for Neutropenic Patients
Creating a safe environment is key for patients with neutropenia. We must think about many factors. A clean and safe space is vital to prevent infections and keep these patients well.
Maintaining a Clean and Safe Environment
To keep the environment clean and safe, we focus on several important areas. First, we make sure the patient’s room is tidy and free of clutter. Clutter can hide bacteria and other harmful germs. We also clean and disinfect all surfaces, like floors, countertops, and furniture, with the right cleaning solutions.
Key strategies for maintaining a clean environment include:
- Regular cleaning and disinfecting of high-touch areas such as door handles, light switches, and bed rails.
- Using personal protective equipment (PPE) when interacting with patients or their environment.
- Implementing a strict hand hygiene policy for all healthcare workers and visitors.
Cleaning and Disinfecting Procedures
Effective cleaning and disinfecting are essential to stop infections from spreading. We use EPA-registered disinfectants that kill many types of germs. It’s important to follow the product’s instructions carefully, including the right dilution and contact time.
Best practices for cleaning and disinfecting include:
- Cleaning surfaces before disinfecting to remove dirt and debris.
- Using the correct disinfectant for the type of surface being cleaned.
- Ensuring that all staff members understand and follow the cleaning and disinfecting protocols.
By using these strategies and procedures, we can greatly lower the risk of infection for neutropenic patients. This helps create a safer environment for them during their treatment.
Nutrition and Neutropenia: Dietary Considerations
Patients with neutropenia need careful dietary planning to avoid infections and keep their nutrition up. Nurses and healthcare providers should focus on key dietary tips. These ensure patient safety and the best health outcomes.
Safe Food Handling for Neutropenic Patients
Safe food handling is key to preventing infections in neutropenic patients. Here are some important practices:
- Avoid raw or undercooked foods, such as raw eggs, undercooked meat, and unpasteurized dairy products.
- Ensure all food is stored, handled, and cooked properly to prevent cross-contamination.
- Use Page water for drinking, cooking, and making ice.
- Wash hands thoroughly before and after handling food.
Following these guidelines can greatly lower the risk of foodborne illnesses in at-risk patients.
Recommended Nutritional Guidelines
Nutritional guidelines for neutropenic patients aim to provide a balanced diet. We recommend:
- Increasing protein intake to support immune function and overall health.
- Consuming a variety of fruits and vegetables, ensuring they are washed and cooked properly.
- Including whole grains and lean proteins in the diet.
- Avoiding high-risk foods that may harbor infections.
These nutritional strategies help manage neutropenia and improve patients’ overall well-being.
Monitoring and Recognizing Symptoms of Infection
Watching for infection is key for neutropenic patients. We need to be careful and know the signs well. As healthcare workers, spotting infection signs early is vital for helping our patients.
Key Signs and Symptoms to Watch For
Patients with neutropenia face a higher risk of getting infections. This is because their immune systems are weak. Look out for these common symptoms:
- Fever, often the first sign of infection
- Chills or sweating
- Sore throat or mouth sores
- Cough or difficulty breathing
- Pain or burning during urination
- Redness, swelling, or pain around wounds or catheter sites
As part of a detailed neutropenia nursing care plan, it’s important to check patients often for these signs. Using personal protective equipment (PPE) is also key to stop infections from spreading.
Importance of Early Detection and Intervention
Finding infections early in neutropenic patients makes a big difference. Quick action, like starting antibiotic therapy, can lower the risk of serious problems. Knowing the importance of neutropenic precautions and using them right helps keep our patients safe.
In summary, careful monitoring and recognizing symptoms of infection are essential for managing neutropenia well. By watching closely and using the right ppe for neutropenic precautions, we can give our patients the best care.
Medication Management in Neutropenic Patients
Managing medications is key for neutropenic patients. It involves several important strategies. We must understand the role of growth factor therapy and antibiotic prophylaxis in their care.
Understanding Growth Factor Therapy
Growth factor therapy is vital for managing neutropenia. It uses medications to boost the bone marrow’s production of white blood cells. This helps lower the risk of infections.
Granulocyte-colony stimulating factor (G-CSF) is a common growth factor. It has been proven to reduce neutropenia’s incidence and duration.
We give G-CSF as an injection, once a day, starting 24-48 hours after chemotherapy. The dosage and treatment length depend on the medication, patient factors, and neutropenia’s cause. It’s important to check the patient’s white blood cell count to see if the therapy is working.
Antibiotic Prophylaxis Considerations
Antibiotic prophylaxis is also critical in managing neutropenia. We use antibiotics to prevent infections in high-risk patients. The choice of antibiotic and how long to use it depend on the patient’s condition, chemotherapy type, and local resistance patterns.
| Antibiotic | Dosage | Duration |
| Ciprofloxacin | 500 mg twice daily | Until neutrophil recovery |
| Levofloxacin | 500 mg once daily | Until neutrophil recovery |
When starting antibiotic prophylaxis, we must watch for antibiotic resistance and monitor for infection signs or adverse reactions. A good nursing care plan for neutropenia includes managing medications, preventing infections, and educating patients and families about neutropenic precautions.
Understanding growth factor therapy and antibiotic prophylaxis helps us develop effective neutropenic precautions nursing strategies. This improves patient outcomes.
Communication Among Healthcare Team Members
To get the best results for neutropenic patients, it’s key for healthcare teams to talk well. They need to share patient info right and keep everyone updated on the patient’s health.
Importance of Collaboration in Care Delivery
Working together is vital for neutropenic patient care. It lets healthcare pros share knowledge and plan care together. Effective collaboration means regular team talks, clear lines of communication, and a solid care plan.
When teams work well together, they can:
- Lower the chance of infections spreading
- Boost patient results with quick actions
- Make patients and families happier with their care
Reporting and Documenting Changes in Condition
It’s important to report changes in a patient’s health fast and right for neutropenic patients. Prompt documentation in the patient’s file keeps everyone in the loop and helps them act fast.
| Action | Responsibility | Timeline |
| Monitor patient’s temperature | Nursing staff | Every 4 hours |
| Report any temperature elevation | Nursing staff | Immediately |
| Document changes in condition | Nursing and medical staff | Within 1 hour of observation |
By teaming up and keeping communication clear, healthcare teams can give the top-notch care neutropenic patients need.
Educating Patients on Neutropenic Precautions
Nurses play a key role in teaching patients about neutropenic precautions. This education is vital to lower the risk of infections in those with neutropenia.
Informational Resources for Patients
We give patients informational resources to grasp neutropenic precautions. These include educational brochures, online materials, and counseling sessions.
Some key resources we offer are:
- Detailed guides on neutropenic precautions
- Online portals with educational videos and FAQs
- One-on-one counseling sessions with our nursing staff
Empowering Patients to Take Charge of Their Health
Empowering patients means teaching them to keep a safe environment. We also teach them about proper hygiene and how to spot early signs of infection.
To empower our patients, we:
- Teach them about the importance of hand hygiene and proper food handling
- Educate them on recognizing signs of infection, such as fever and chills
- Encourage them to ask questions and seek help when needed
| Educational Resource | Description | Benefit |
| Educational Brochures | Detailed guides on neutropenic precautions | Easy to understand and reference at home |
| Online Materials | Videos, FAQs, and interactive content | Accessible from anywhere, at any time |
| Counseling Sessions | One-on-one sessions with nursing staff | Personalized guidance and support |
Community Resources and Support Systems
Community support is key for Page during treatment that may cause neutropenia. We know that care goes beyond just medical treatment. It also includes support from the community.
Support Groups and Educational Workshops
Support groups offer a supportive space for patients to share and get emotional support. Educational workshops provide important info on managing neutropenia and improving care.
- Support groups help patients and their families feel connected and supported.
- Educational workshops give practical tips on nutrition and managing symptoms.
Navigating Healthcare Services for Additional Help
Navigating the healthcare system can be tough, but there are resources to help. Page can find services like home healthcare, nutritional counseling, and more medical support.
Page Page Pageble>
Using these community resources and support systems can improve care for neutropenic patients. We aim to provide full support that meets each patient’s unique needs.
| Resource | Description | Benefits |
| Home Healthcare Services | Professional medical care at home. | It’s convenient, personalized, and keeps care consistent. |
| Help with safe food handling and nutrition planning. | It improves health and lowers infection risk. | |
| Additional Medical Support | Access to specialists and more medical services. | It offers complete care and timely help. |
Conclusion: Essential Takeaways for Nurses
Neutropenic precautions are key for nurses caring for patients with chemotherapy-induced neutropenia. Understanding neutropenia’s causes and using effective nursing interventions can greatly improve patient outcomes.
A good neutropenia nursing care plan is vital for quality care. It involves assessing patient risks, educating patients and families, and keeping the environment clean and safe. Nursing interventions, like monitoring for infection signs and managing medications, are also critical.
It’s important for nurses to keep learning and stay updated on neutropenic care best practices. This ensures our patients get the support they need to successfully go through their treatment.
FAQ
What are neutropenic precautions, and why are they important for nurses caring for patients with chemotherapy-induced neutropenia?
Neutropenic precautions help prevent infections in patients with low neutrophil counts, often due to chemotherapy. Nurses must understand and follow these precautions to keep patients safe and prevent serious infections.
What is neutropenia, and how does it affect the immune system?
Neutropenia is when there are too few neutrophils, a key white blood cell. This weakens the immune system, making patients more likely to get infections.
What are the common causes of chemotherapy-induced neutropenia?
Neutropenia is a common side effect of cancer treatment. It happens when certain chemotherapy drugs slow down bone marrow, reducing neutrophil production.
How can nurses assess patient risks and needs for neutropenic care?
Nurses check a patient’s medical history, current health, and lab results like the absolute neutrophil count (ANC). This helps figure out the risk of infection.
What role does patient education play in neutropenic care, and how can nurses educate patients and their families on safety measures?
Teaching patients about neutropenia is key. Nurses teach them about hand hygiene, avoiding sick people, and recognizing infection signs. This helps prevent infections.
What are the key components of standard precautions for neutropenic patients, and how can they be implemented?
Standard precautions include washing hands often and using protective gear like gloves and masks. These steps help reduce infection risk.
How can healthcare providers maintain a clean and safe environment for neutropenic patients?
Keeping the environment clean involves regular disinfection of surfaces and equipment. Visitors and staff must also follow infection control rules.
What dietary considerations are important for neutropenic patients to prevent infections?
Patients should avoid raw foods and unpasteurized dairy. They should eat a balanced diet with fruits, veggies, and lean proteins.
What are the key signs and symptoms of infection that nurses should monitor in neutropenic patients?
Nurses watch for fever, chills, sore throat, cough, and shortness of breath. Any changes in wounds or catheter sites could mean an infection.
How does growth factor therapy play a role in managing neutropenia?
Growth factor therapy, like G-CSF, helps the bone marrow make more neutrophils. This lowers the risk of infection in neutropenic patients.
Why is communication among healthcare team members important for neutropenic patients?
Good communication ensures all aspects of care are coordinated. It helps address any changes in a patient’s condition quickly, improving safety and outcomes.
What community resources and support systems are available for neutropenic patients and their families?
There are support groups, educational workshops, and healthcare services. These offer help and guidance for managing neutropenia and its complications.
What is the role of antibiotic prophylaxis in neutropenic patients?
Antibiotic prophylaxis may be used for high-risk patients to prevent infections. It’s tailored to each patient’s needs and risk factors.
How can nurses empower patients to take charge of their health while undergoing neutropenic precautions?
Nurses give patients information and teach them self-care. They encourage patients to follow their treatment plans and report any concerns or symptoms.
References
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/cancer/preventinfections/neutropenia.htm









