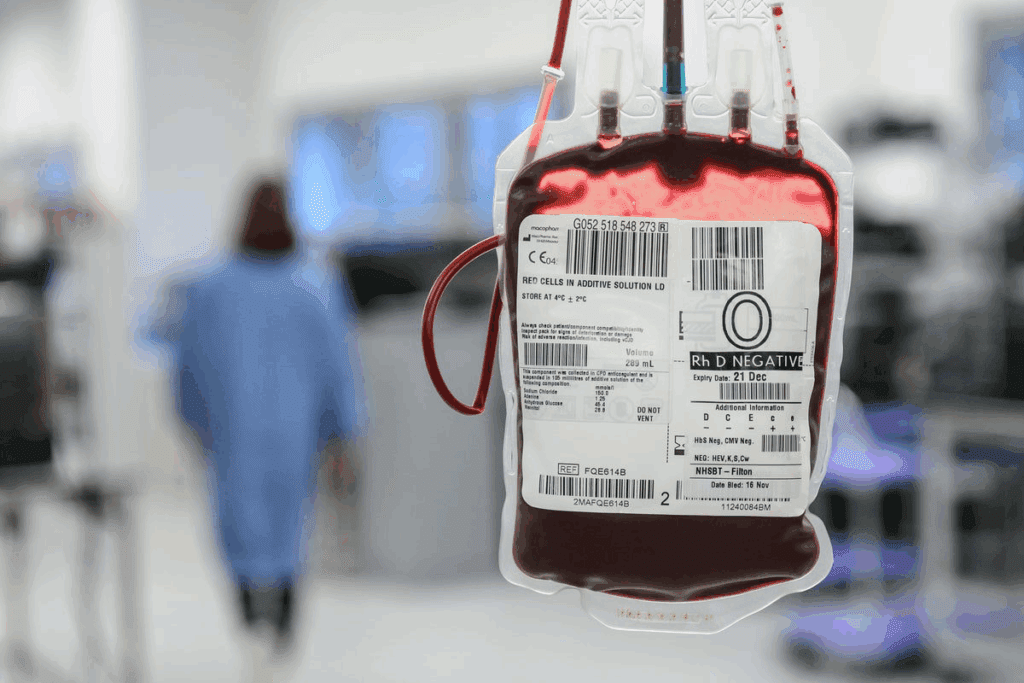
Did you know thousands of kids worldwide get blood transfusions every year? Safe transfusion practices are key for them, mainly those with blood disorders or going through surgery. A guide to calculating and adjusting the infusion Platelet transfusion rate based on patient condition and volume requirements.
We know how vital it is to follow guidelines to lower risks and better patient results. The World Health Organization (WHO) has comprehensive guidelines for safe blood transfusions, including pediatric blood transfusion guidelines.
It’s important for healthcare workers to understand these guidelines to give the best care to kids. By sticking to these guidelines, we can greatly improve care quality and lessen risks from platelet transfusions.
Key Takeaways
- Pediatric patients need special care with blood transfusions.
- The WHO offers guidelines for safe transfusions.
- Following these guidelines reduces risks and improves patient outcomes.
- Knowing platelet transfusion rates is key for healthcare providers.
- Safe transfusion practices are vital for better patient care.
What is a Platelet Transfusion?
A platelet transfusion is a medical procedure to help patients with low platelet counts or platelet problems. It’s very important for kids who need to manage their bleeding risks carefully.
Definition and Purpose
Platelet transfusions give platelets to patients with low platelet counts or platelet issues. The main goal is to stop or treat bleeding problems. We give platelet transfusions to patients with low platelets or platelet problems to prevent bleeding.
Indications for Use
Platelet transfusions are needed for thrombocytopenia caused by bone marrow failure, chemotherapy, or other reasons. Kids with platelet function disorders also need them to manage bleeding risks. The World Health Organization (WHO) guidelines help decide when to use platelet transfusions. They say to use them for severe thrombocytopenia or when there’s a high risk of bleeding.
Overview of the WHO Guidelines
The World Health Organization (WHO) has set up detailed guidelines for platelet transfusions. They focus on putting the patient first. These rules are key for making sure transfusions are safe and work well, mainly for kids.
Key Recommendations for Pediatric Patients
The WHO guidelines have special advice for kids. They talk about the right amount and how to give platelets. Kids need careful thought because they are different from adults. We must think about their health, lab results, and any other conditions when deciding on transfusions.
Application in Clinical Practice
Using the WHO guidelines in real life means working together. Doctors, nurses, and others must check on patients, watch how transfusions go, and change plans if needed. The guidelines stress the importance of keeping an eye on patients and being ready to adjust plans.
Factors Influencing Platelet Transfusion Rates
Platelet transfusions in kids are affected by many things. These include their age, weight, and health conditions. Knowing these helps doctors make better choices for blood transfusion in pediatrics and pediatric transfusion.
Age and Weight Considerations
Age and weight are key when it comes to platelet transfusions in kids. Smaller kids and those who weigh less might need smaller doses to avoid too much fluid. It’s important to think about these when deciding how much and how often to give platelet transfusions.
Doctors usually figure out the platelet dose based on the kid’s weight. They aim for a certain platelet count after the transfusion. For example, a dose of 10-20 mL/kg is common, but it can change based on the patient’s specific needs and health.
Disease States Impacting Platelet Levels
Different diseases can really affect platelet levels in kids, making them need more transfusions. Leukemia, lymphoma, and other cancers can cause low platelet counts because they affect the bone marrow or because of chemotherapy.
Other diseases like sepsis, DIC, and some genetic disorders can also lower platelet counts. We need to watch these patients closely and adjust their transfusions to help them the best we can.
Understanding how different factors affect platelet transfusions helps us give better care to kids. Tailoring care to each child is key to better outcomes and fewer risks with pediatric transfusion.
Pediatric Population: Unique Considerations
The pediatric population needs a special approach to platelet transfusions. This is because of their unique physiology and health issues. It’s important to know how development and specific conditions affect their platelet count and health.
Developmental Factors
Developmental factors are key in how pediatric patients respond to platelet transfusions. Children’s blood-making systems are not fully grown. This can affect their platelet production and function.
For example, newborns are more likely to have low platelet counts because their blood-making systems are immature. As kids get older, their platelet counts and functions change. This means they need age-specific guidelines for transfusions.
Key developmental considerations include:
- Age-related changes in platelet count and function
- Maturation of the hematopoietic system
- Weight and body size considerations for transfusion dosage
Common Conditions Requiring Transfusion
Some conditions are more common in kids and may need platelet transfusions. These include neonatal alloimmune thrombocytopenia, sepsis, and blood cancers. It’s important for healthcare providers to know about these conditions to make the right decisions about platelet transfusions.
Common conditions requiring platelet transfusion in pediatric patients:
- Neonatal alloimmune thrombocytopenia
- Sepsis or severe infection
- Hematological malignancies or bone marrow failure
- Congenital thrombocytopenia
Understanding these unique factors helps healthcare providers manage kids needing platelet transfusions. They can ensure these children get the best care possible, following the latest guidelines and research.
The Risks and Benefits of Platelet Transfusion
It’s important to know the risks and benefits of platelet transfusions for kids. These transfusions are lifesaving for many children. They help when treatments lower their platelet count. But, they also have risks and benefits.
Potential Complications
Platelet transfusions are mostly safe but can cause problems. Transfusion-related acute lung injury (TRALI) is a serious issue. It causes non-cardiogenic pulmonary edema. Another big risk is graft-versus-host disease (GVHD). This is when the transfused lymphocytes attack the recipient’s tissues.
We need to watch patients closely for these complications. This way, we can act fast if needed.
Clinical Benefits for Pediatric Patients
Despite the risks, platelet transfusions are very helpful for kids. They prevent bleeding in those with low platelets or before surgery. They also help in intensive care, managing serious conditions.
By understanding the risks and benefits, we can give our patients the best care.
Evaluating Platelet Count and Transfusion Needs
Keeping an eye on platelet counts is key in pediatric transfusions. Kids have special needs that require careful thought when checking platelet counts and deciding on transfusions.
The World Health Organization (WHO) suggests watching platelet counts closely. They also say to transfuse based on the situation. This way, kids get transfusions when they really need them, without getting too many.
Monitoring Platelet Levels
It’s important to check platelet levels often in kids, mainly those with low platelets or going through treatments that affect platelet counts. Frequent assessments help doctors decide if a platelet transfusion is needed.
We use different ways to check platelet levels, like complete blood counts (CBCs) and other tests. These tests tell us about the patient’s platelet count and overall blood health.
Thresholds for Transfusion
Setting the right threshold for platelet transfusions is important for kids. The decision to give platelets depends on the patient’s health, diagnosis, and risk of bleeding.
The WHO guidelines say the threshold for transfusion changes based on the situation. For example, kids with very low platelets or those having big surgeries might need different levels. We follow these guidelines to make sure our patients get the best care.
By carefully looking at platelet counts and transfusion needs, we can give our pediatric patients the care they need. This helps improve their outcomes and reduces risks.
Alternatives to Platelet Transfusion
Healthcare providers are looking for new ways to help kids, beyond just platelet transfusions. As science moves forward, we need more options for treating kids’ blood issues. This is because kids need special care when it comes to their blood.
Medications and Treatments
Researchers are working on medicines that help make more platelets. These could mean fewer transfusions for kids. For example, some drugs are being tested to see if they can increase platelet counts.
New medicines are also being made to help kids who need transfusions. These include:
- Growth Factors: These help the bone marrow make more platelets.
- Immunomodulatory Drugs: They help manage conditions that lower platelet counts.
Emerging Therapies
New treatments are also on the horizon. They could change how we treat platelet issues. Some of these include:
- Gene therapy to fix platelet problems at their source.
- Cell therapies that might fix platelet function.
These new options are not just about finding new treatments. They also aim to make care safer and more tailored to each child. This means less risk of bad reactions or infections from transfusions.
As we look into these new ways, following paediatric transfusion guidelines is key. This ensures kids get the best and safest care. It’s all about making sure they get the treatment they need.
The Role of Healthcare Providers
Healthcare providers are key in managing platelet transfusions for kids. We, as a team, know how complex these decisions are. We make sure to make the best choices for our young patients.
Interdisciplinary Team Approach
An interdisciplinary team is vital for kids needing platelet transfusions. This team includes hematologists, pediatricians, nurses, and more. They work together to check the patient’s health, decide if a transfusion is needed, and watch how the patient reacts.
Key components of an effective team approach include:
- Clear communication among team members
- Collaborative decision-making
- Continuous monitoring and assessment of the patient’s condition
A leading expert in pediatric hematology says, “A team-based approach ensures that all aspects of a patient’s care are considered, leading to better outcomes in pediatric patients undergoing platelet transfusion.”
“The complexity of managing platelet transfusions in children demands a multifaceted approach that only a diverse team of healthcare professionals can provide.”
A Pediatric Hematologist
Importance of Communication with Families
Talking clearly with families is key when it comes to platelet transfusions in kids. We need to make sure families know the risks, benefits, and options. They should also understand what the transfusion involves.
| Aspect of Communication | Description |
| Clear Explanation | Providing a straightforward explanation of the transfusion process and its rationale |
| Emotional Support | Offering emotional support to families dealing with the stress and uncertainty of transfusion |
| Informed Consent | Ensuring that families understand and agree to the transfusion process through informed consent |
By working together as a team and talking openly with families, we can give kids the best care. This includes following pediatric transfusion guidelines closely.
Patient Education and Consent
Informed consent is key when giving platelet transfusions, even more so for kids. It’s important to tell families all about the procedure, its risks, and benefits. This builds trust and helps them work together with us.
Ensuring Informed Consent
We need to give clear, simple info about platelet transfusions. We should explain why it’s needed, how it’s done, and any possible problems. Being open is vital so families can make good choices for their child.
A top ethicist says informed consent is more than a rule. It’s about respecting patients’ freedom and dignity. This is very important in kids’ care, where parents make decisions for them.
Addressing Family Concerns
Families often worry about platelet transfusions. They might be scared of bad reactions, getting sick, or how it will affect their child’s health. We need to answer these worries with honest, caring info.
“Good communication is the base of trust between doctors and families. By listening and sharing clear info, we can calm fears and work together better.”
A pediatric hematologist
To help families understand, we can use educational materials and tools. For example, a table with key points about platelet transfusions can be really helpful.
| Aspect | Description | Benefits/Risks |
| Procedure | Platelet transfusion involves giving platelets through a vein. | Benefits: Stops bleeding; Risks: Allergic reactions, infection. |
| Indications | Low platelet count due to many reasons. | Benefits: Lowers risk of bleeding; Risks: Possible bad reactions. |
| Monitoring | Watching the platelet count and the patient’s health closely. | Benefits: Makes sure it works and is safe; Risks: None if done right. |
By teaching patients and their families and making sure they understand, we offer care that’s not just good but also kind and respectful.
Future Directions in Transfusion Practices
Transfusion practices are evolving with new research and policy updates. It’s important to keep up with these changes in pediatric care. We’re moving towards more tailored and accurate transfusion methods.
Research Trends and Innovations
Research in pediatric transfusion is exploring new blood component therapies. Innovations in transfusion medicine are making transfusions safer and more effective. For example, studies are looking into pathogen-reduced platelet components to lower infection risks.
Another focus is on precision medicine in transfusions. This means tailoring treatments to each child’s genetic makeup and health needs. Such personalized care could greatly improve patient results.
Policy Changes and Recommendations
Policy updates and new clinical guidelines are also key in shaping transfusion practices. Professional organizations and regulatory groups are regularly updating their guidelines. These updates reflect the latest research and best practices in transfusion medicine.
For instance, new guidelines might suggest when to give platelet transfusions to kids or alternative treatments to reduce transfusion needs. These changes aim to improve patient safety and make better use of blood products.
We’re dedicated to keeping up with these advancements. This ensures our care for pediatric patients is top-notch. By following the latest research and guidelines, we can offer the best possible care.
Conclusion: Best Practices for Care
Managing platelet transfusions in kids is key for safe and good results. We talked about the need to know about platelet transfusion rates and guidelines. We also looked at what affects these rates.
The World Health Organization (WHO) guidelines help us follow best practices in transfusion care. This includes pediatric blood transfusion guidelines and pediatric transfusion guidelines. By sticking to these guidelines, healthcare providers can give kids the best care possible.
Key Takeaways
Following pediatric transfusion guidelines is vital to reduce risks and increase benefits of platelet transfusions. Healthcare providers need to think about the child’s age, weight, and health when deciding on transfusions.
Guideline Adherence
By following WHO guidelines and keeping up with new research, we can offer top-notch care to kids. This means knowing about new treatments and options instead of platelet transfusions.
FAQ
What are the guidelines for platelet transfusions in pediatric patients?
The World Health Organization (WHO) has guidelines for platelet transfusions in kids. They cover the right dose and how to give platelets. They also list when to use them, like when platelet counts are low.
What is thrombocytopenia, and how is it treated with platelet transfusions?
Thrombocytopenia means having too few platelets. Platelet transfusions help by adding more platelets. This can lower the risk of bleeding.
How do age and weight affect platelet transfusion requirements in pediatric patients?
A kid’s age and weight matter for platelet transfusions. The amount needed can change based on these factors. Doctors must think about these when deciding on transfusions.
What are the possible complications of platelet transfusions in pediatric patients?
Kids might face complications like TRALI and GVHD from platelet transfusions. Doctors must carefully consider the risks and watch for any signs of trouble.
What are the alternatives to platelet transfusion, and when are they used?
Instead of transfusions, there are medicines and new treatments. These might help some patients and reduce the need for transfusions, depending on their situation.
How do healthcare providers determine the need for platelet transfusions in pediatric patients?
Doctors check platelet counts and decide if transfusions are needed. They keep an eye on platelet levels and set clear rules for when to transfuse.
What is the role of patient education and consent in platelet transfusions?
Teaching patients and getting their consent is key. It’s important to tell families about the procedure, its risks, and benefits. Doctors should answer questions and explain the process.
What are the future directions in transfusion practices for pediatric patients?
The future looks bright with new research and treatments. There are also changes in policies to make transfusions safer and more effective for kids.
How do pediatric transfusion guidelines differ from adult guidelines?
Kids have their own guidelines because they are different from adults. These take into account their growth and common conditions like neonatal alloimmune thrombocytopenia.
What is the importance of adhering to guidelines for platelet transfusions in pediatric patients?
Following guidelines is vital for safe and effective care in kids. It helps reduce risks and improves outcomes by sticking to established best practices.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2764835