Last Updated on October 20, 2025 by
Being told you have a mass on the liver is scary, even more so for kids. Hepatoblastoma is a rare liver cancer that needs quick and accurate treatment to live.
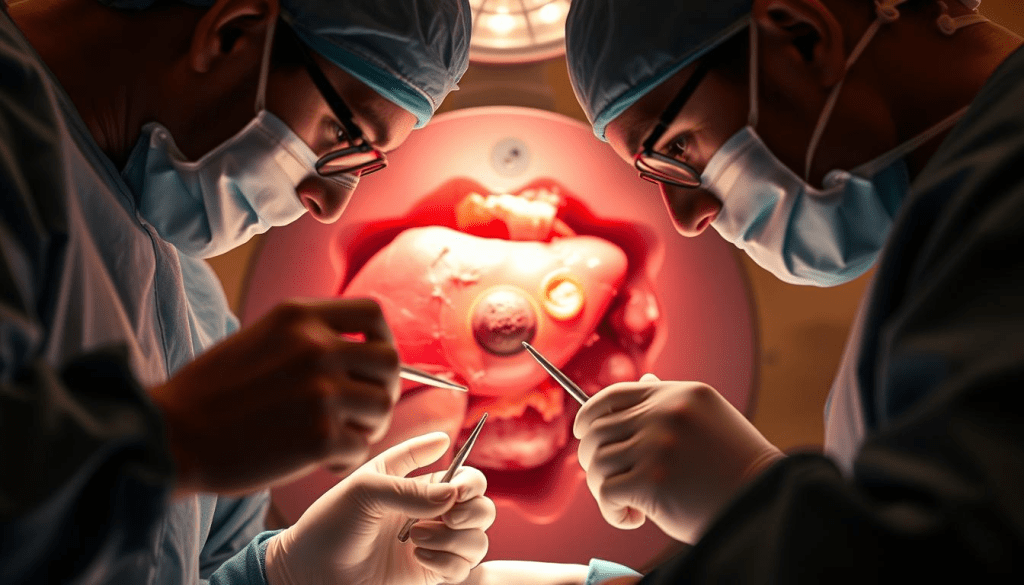
We offer top-notch healthcare and support for patients from around the world. We know that a tumor on the liver needs fast and effective care. The main treatment for hepatoblastoma is removing it all through surgery. This is the only way to possibly cure it.
New ways in chemotherapy and surgery have made treating hepatoblastoma much better. Now, more than 75% of people can survive. We’ll look into this treatment and other important details. We aim to give hope and clear answers to those facing this tough condition.
Hepatoblastoma is the most common liver cancer in kids. It needs a detailed approach for diagnosis and treatment. We will cover what this condition is, its symptoms, and how it’s diagnosed.
Hepatoblastoma is a rare hepatic tumor that mainly hits kids. It often shows up as an abdominal mass or pain. Spotting the tumor’s features and size is key to diagnosing it.
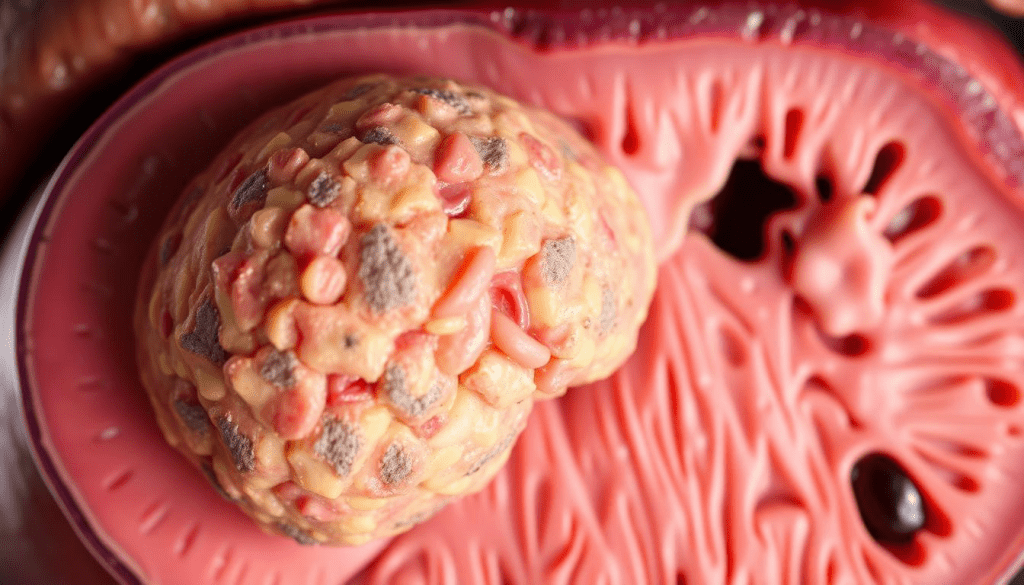
Doctors use imaging and lab tests, like alpha-fetoprotein (AFP) levels, to diagnose it. The National Cancer Institute says knowing the tumor’s stage and type is essential for treatment.
Thanks to advances, kids with hepatoblastoma have better chances of survival. The 3-year survival rate is about 79-81%, and the 5-year rate is nearly 70“76%. Factors like tumor stage, age, and AFP levels play a big role.
| Prognostic Factor | Impact on Survival |
| Tumor Stage | Advanced stages have poorer survival rates |
| Age | Younger children tend to have better outcomes |
| Alpha-fetoprotein (AFP) Levels | Abnormal AFP levels can indicate tumor presence and response to treatment |
Knowing these factors helps us create better treatment plans. We aim to give our patients the best chance of recovery. We use the latest in hepatoblastoma treatment to help them.
Finding out if someone has hepatoblastoma is very important. We use many tools and a team approach to make sure our patients get the right treatment.
Hepatoblastoma often shows up as a mass in the abdomen. You might feel it during a check-up or see it on scans. Symptoms can include a big belly, pain, or not wanting to eat.
Tests like ultrasound, CT scans, or MRI are key in finding the tumor. They help us see the tumor in the liver and how big it is. A biopsy, where we take a piece of the tumor, is needed to confirm the diagnosis.
Knowing the stage of hepatoblastoma is very important. It tells us how to treat it. We use systems like PRETEXT to figure out how big the tumor is and where it is.
The stage of the tumor helps us decide if surgery is needed or if other treatments like chemotherapy or a liver transplant are better. Knowing the stage helps us make a treatment plan that fits each patient’s needs.
By understanding the symptoms, stage, and how big the tumor is, we can give our patients the best care. Our team works together to make sure each patient gets a treatment plan that’s right for them.
Preoperative chemotherapy has changed how we treat hepatoblastoma. It makes liver tumors that were once too big to remove now operable. We use chemotherapy like cisplatin and doxorubicin (PLADO) to shrink tumors. This increases the chances of a successful surgery.
Chemotherapy before surgery is key in treating hepatoblastoma. It makes mass on the liver smaller, turning big tumors into ones we can remove. This method also helps us see how well the tumor responds to treatment.
It’s important to check how well the tumor responds to chemotherapy. We use scans and tumor markers to watch the patient’s progress. A big drop in tumor size means the treatment is working well. But, if the tumor doesn’t shrink or gets bigger, we might need to change the treatment plan.
The main advantages of preoperative chemotherapy are:
In summary, preoperative chemotherapy is a vital part of treating hepatoblastoma. By shrinking liver tumors and checking how they respond, we can customize treatment for each patient. This approach helps improve outcomes.
Surgical resection is the main treatment for hepatoblastoma, giving patients the best chance to live long. We use advanced techniques to remove the tumor and keep as much liver function as we can.
Partial hepatectomy means removing the liver part with the tumor. Our surgeons are skilled in finding and removing the tumor while keeping enough liver to function. The surgery is customized for each patient based on their liver and tumor size.

The success of this surgery depends on the tumor’s size, location, and the patient’s health. We work with our oncology team to decide the best surgery plan for each patient.
Removing all cancer cells is key to better outcomes for patients with hepatoblastoma. This means taking out not just the tumor but also any tiny cancer cells. Our surgeons use the latest imaging and techniques to ensure all cancer is gone.
Studies show that removing all cancer cells greatly improves survival rates. We follow strict protocols to give our patients the best care. For more on this, see studies in reputable journals, like the one here.
The tumor’s location in the liver affects the surgery plan. Tumors in some areas may need more complex surgeries. Our surgeons are skilled in these cases, using the latest tools for success.
| Tumor Location | Surgical Approach | Considerations |
| Left lobe | Left hepatectomy | Preservation of right liver lobe function |
| Right lobe | Right hepatectomy | Assessment of left liver lobe adequacy |
| Central | Central hepatectomy | Complex procedure requiring precise planning |
By customizing the surgery for each patient, we aim to improve outcomes and survival chances.
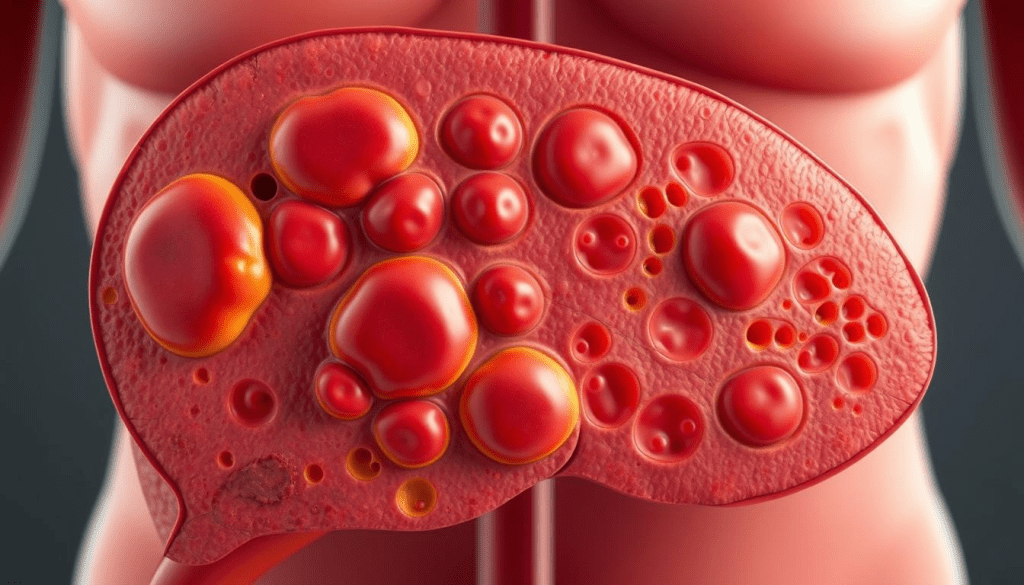
When hepatoblastoma is too big to remove, a liver transplant is often considered. This treatment has shown great promise for those facing this challenge.
We’ve seen great success with liver transplants, with survival rates up to 84%. This success shows how important it is to consider a transplant for unresectable hepatoblastoma. Our team helps patients and families decide if a transplant is right for them.
Key Considerations for Liver Transplantation
A leading medical expert says, “Liver transplantation has changed the game for unresectable hepatoblastoma, giving many patients a second chance at life.” This shows how vital liver transplants are for this condition.
When a tumor on liver can’t be removed, we carefully consider a transplant. We look at the patient’s health and the chances of success. Our team provides full care and support during treatment.
Knowing the liver cancer survival rate by age helps us plan treatment. While survival rates depend on many factors, transplants have greatly improved outcomes for unresectable hepatoblastoma patients.
By adding liver transplants to treatment plans, we offer hope to those with unresectable hepatoblastoma. Our dedication to top-notch healthcare and support for international patients shapes our approach to this complex condition.
Hepatoblastoma’s outcome depends on several factors. These include the tumor’s stage and the patient’s age. Thanks to advances, the 5-year survival rate for this cancer is now between 70% and 76%.
The tumor’s stage at diagnosis is very important. Patients with early-stage tumors usually do better than those with more advanced ones. Younger patients also tend to have a better chance of survival.
Factors Influencing Hepatoblastoma Prognosis
How well a patient responds to the first treatment is also key. Those who respond well to treatment often live longer.
| Stage | 5-Year Survival Rate |
| Early Stage | 80% |
| Advanced Stage | 50% |
The table shows how survival rates change with the tumor’s stage. Early detection and treatment are vital for better survival chances.
We aim to give the best care to hepatoblastoma patients. We use the latest treatments to improve their outcomes. By understanding what affects prognosis, we can create treatment plans that fit each patient’s needs.
Hepatoblastoma, a rare liver growth, has seen big improvements in treatment. New surgical methods, better chemotherapy, and liver transplants have made a big difference. Our hospital is dedicated to top-notch care for patients from around the world with liver masses.
Our team focuses on patient care, using the latest in medical science. We aim to improve life for those with hepatoblastoma. By using the newest treatments and working together, we aim for the best results for our patients.
Good care is key in fighting hepatoblastoma. We’re committed to keep pushing forward, making sure our patients get the best care possible.
Hepatoblastoma is a common liver cancer in kids. It shows up as a mass in the belly.
Doctors use imaging and check symptoms to find hepatoblastoma. They also stage it to plan treatment.
Chemotherapy before surgery makes tumors smaller. This makes them easier to remove. Cisplatin and doxorubicin are often used.
Surgery is the main treatment for hepatoblastoma. Doctors use partial hepatectomy to remove the tumor completely.
Kids with hepatoblastoma have a 70“76% chance of living 5 years. This depends on the tumor stage, age, and treatment response.
Liver transplant is an option for tumors that can’t be removed. It has a survival rate of up to 84%
Checking how tumors respond to treatment is key. Our team watches patient progress to adjust treatment plans.
Getting rid of all tumor cells is vital. It greatly improves survival chances for patients.
Centers for Disease Control and Prevention. (2024). Facts about birth defects. https://www.cdc.gov/ncbddd/birthdefects/facts.html
Hockenberry, M. J., Wilson, D., & Rodgers, C. C. (2019). Wong’s nursing care of infants and children (11th ed.). Mosby. https://www.elsevier.com/books/wongs-nursing-care-of-infants-and-children/hockenberry/978-0-323-54939-5
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). (2023). Patient information on hernia repair. https://www.sages.org/publications/patient-information/patient-information-for-hernia-repair-from-sages/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!