neurocritical care
Every year, over 700,000 Americans are admitted to ICUs with severe brain conditions. This shows the need for more neurocritical care experts. Doctors from internal medicine and other fields are looking into this career path.
We look into whether you can move into neurocritical care after an internal medicine residency. This includes talking about the extra training needed, like fellowship programs. We also discuss the chances in this demanding field.
Key Takeaways
- Doctors from different fields can become neurointensivists with more training.
- Internal medicine is a good base for moving into neurocritical care.
- Fellowship training is key for getting the right skills and knowledge.
- Neurocritical care deals with serious brain and brain surgery cases.
- A career in neurocritical care offers chances for growth and challenge.
Understanding Neurocritical Care
A modern, well-equipped neurocritical care unit bathed in bright, natural lighting that streams in through large windows. The foreground features a hospital bed with advanced medical equipment, monitors, and an array of life-support systems. In the middle ground, a team of dedicated healthcare professionals, including nurses and physicians, carefully tending to a critically ill patient. The background showcases the clean, sterile environment with state-of-the-art technology and infrastructure designed to provide the highest level of neurological care and support. The overall atmosphere conveys a sense of expertise, compassion, and the unwavering commitment to patient well-being.
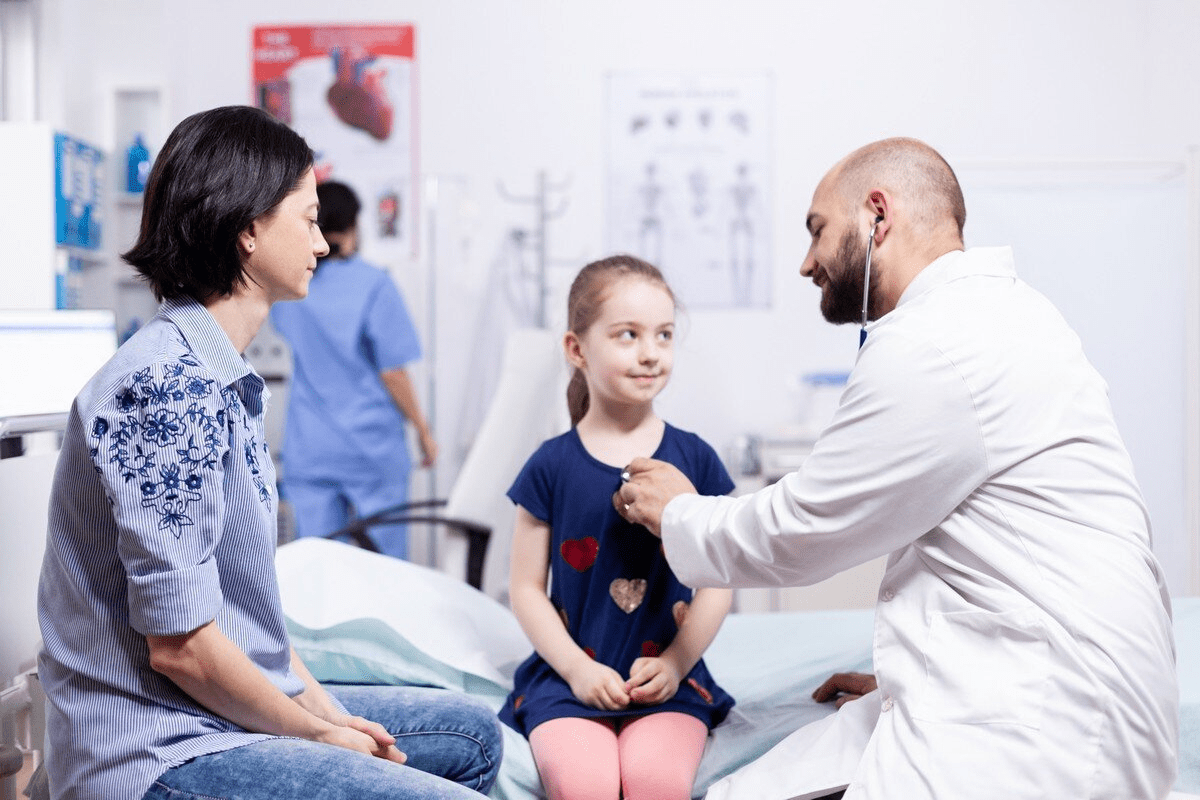
Neurocritical care is a key area in treating seriously ill brain and brain surgery patients. It connects the brain with other body systems when a patient is very sick.
Definition and Scope of Neurocritical Care
Neurocritical care deals with the intensive care of patients with severe brain and brain surgery illnesses. This includes acute stroke, traumatic brain injury, and status epilepticus. It covers a wide range, needing deep knowledge of brain and body problems in critical patients.
In a neurocritical care unit (NCCU), a team of experts works together. They focus on neurological assessment, neuromonitoring, and neuroimaging interpretation for patients.
Evolution of Neurocritical Care as a Subspecialty
Neurocritical care has grown a lot in recent years. This is thanks to new medical technology and better understanding of brain illnesses. Specialized NCCUs have been key, bringing together the needed skills and resources for these complex cases.
- Advances in neuromonitoring and neuroimaging techniques
- Increased understanding of the management of neurological emergencies
- Development of specialized training programs for neurointensivists
The Neurocritical Care Unit (NCCU) Environment
The NCCU is made for high-level care for brain and brain surgery patients. It has the latest monitoring tools and a team with neurocritical care expertise.
The NCCU environment supports detailed care, including managing other health issues. It’s where evidence-based practices are used and care is coordinated among different specialties.
Traditional Pathways to Neurocritical Care

A spacious hospital corridor with gleaming floors and walls in neutral tones. In the foreground, a team of medical professionals – a physician, a nurse, and a respiratory therapist – engaged in a tense consultation, their expressions serious as they review charts and exchange information. The middle ground features patients being transported on gurneys, their faces obscured by oxygen masks, surrounded by beeping monitors and IV stands. In the background, a bank of elevators and signs directing to the neurocritical care unit, highlighting the specialized nature of the care provided. Soft, directional lighting casts a warm, clinical glow, emphasizing the high-stakes, high-intensity environment. Captured with a wide-angle lens to convey the scale and gravity of the scene.
To become a neurointensivist, you often start in key medical fields. Neurology, neurosurgery, and anesthesiology are common starting points. These areas give a solid base for neurocritical care training.
Neurology as the Primary Route
Neurology is a main way to neurocritical care. Neurologists know how to handle neurological problems. Their training helps them understand and manage neurological emergencies well.
Many neurointensivists begin as neurologists. They then get more training in critical care. This helps them manage very sick neurological patients better.
Neurosurgery Connection
Neurosurgery is another key path to neurocritical care. Neurosurgeons deal with the most serious neurological issues. They need intensive care.
They use their surgical skills to help patients. This knowledge is crucial in neurocritical care. It helps them provide full care in intensive settings.
Anesthesiology Pathway
Anesthesiology is also a good way to neurocritical care. Anesthesiologists manage patients’ vital signs during surgery and in critical care. They know a lot about medicines and equipment.
They can use this knowledge in neurocritical care. Anesthesiologists can manage neurological emergencies well. They build on their patient monitoring and life support skills.
Neurology, neurosurgery, and anesthesiology are strong foundations for neurocritical care. Each specialty brings unique skills and knowledge. These are essential for caring for critically ill neurological patients.
As neurocritical care grows, knowing these paths helps future neurointensivists. They can choose the best path for their career goals.
Internal Medicine to Neurocritical Care: Is It Possible?
A group of IM-trained neurointensivists, clad in crisp white coats, intently examining advanced neuroimaging scans projected on a backlit display. The lighting is warm and focused, casting subtle shadows that accentuate their focused expressions. In the foreground, a seasoned clinician gestures toward a detailed CT scan, while their colleagues lean in, their brows furrowed in deep concentration. The background is a modern, high-tech intensive care unit, with sleek medical equipment and a sense of clinical efficiency. The overall atmosphere conveys the specialized knowledge and dedication of these physicians, bridging the gap between internal medicine and the critical care of neurological patients.
Internal medicine doctors might find neurocritical care a tempting but tough path. Can they really switch from internal medicine to neurocritical care?
Historical Perspective on IM-Trained Neurointensivists
Neurocritical care has long been the domain of neurologists and neurosurgeons. Yet, some internal medicine doctors have made the leap. The United Council of Neurological Subspecialties (UCNS) offers Neurocritical Care certification to doctors from various backgrounds, including internal medicine. This shows they can do well in this field.
Current Acceptance of Internal Medicine Background
More and more, internal medicine doctors are being welcomed into neurocritical care. Their broad medical knowledge is seen as a big plus. They’re great at handling complex medical issues and other health problems, which is crucial in the ICU.
Several things have led to this shift. The critical care skills internal medicine doctors learn are very useful in neurocritical care. Also, the UCNS certification has given internal medicine doctors a clear way to show their skills in neurocritical care.
Success Stories and Case Examples
There are many examples of internal medicine doctors thriving in neurocritical care. Some have done fellowships in critical care and then neurocritical care. Others use their internal medicine skills to manage complex cases in the neurocritical care unit, focusing on the overall health of patients.
These stories prove it’s possible for internal medicine doctors to move into neurocritical care. They bring a unique set of skills, like broad medical knowledge and the ability to handle multiple health issues. This makes them a big asset to the neurocritical care team.
Fellowship Training Requirements for IM Graduates
A modern, well-equipped neurocritical care unit with advanced medical equipment and technology. In the foreground, a team of dedicated healthcare professionals, including physicians, nurses, and respiratory therapists, collaborating closely around a critically ill patient’s bedside, closely monitoring vital signs and administering specialized treatments. The middle ground features state-of-the-art monitoring displays, ventilators, and other life-support systems, all carefully calibrated to provide the highest level of care. The background showcases a serene, dimly lit environment with muted tones, creating a soothing atmosphere conducive to patient recovery and healing. Soft, directional lighting illuminates the scene, capturing the technical expertise and attentive care provided in a neurocritical care fellowship training program.
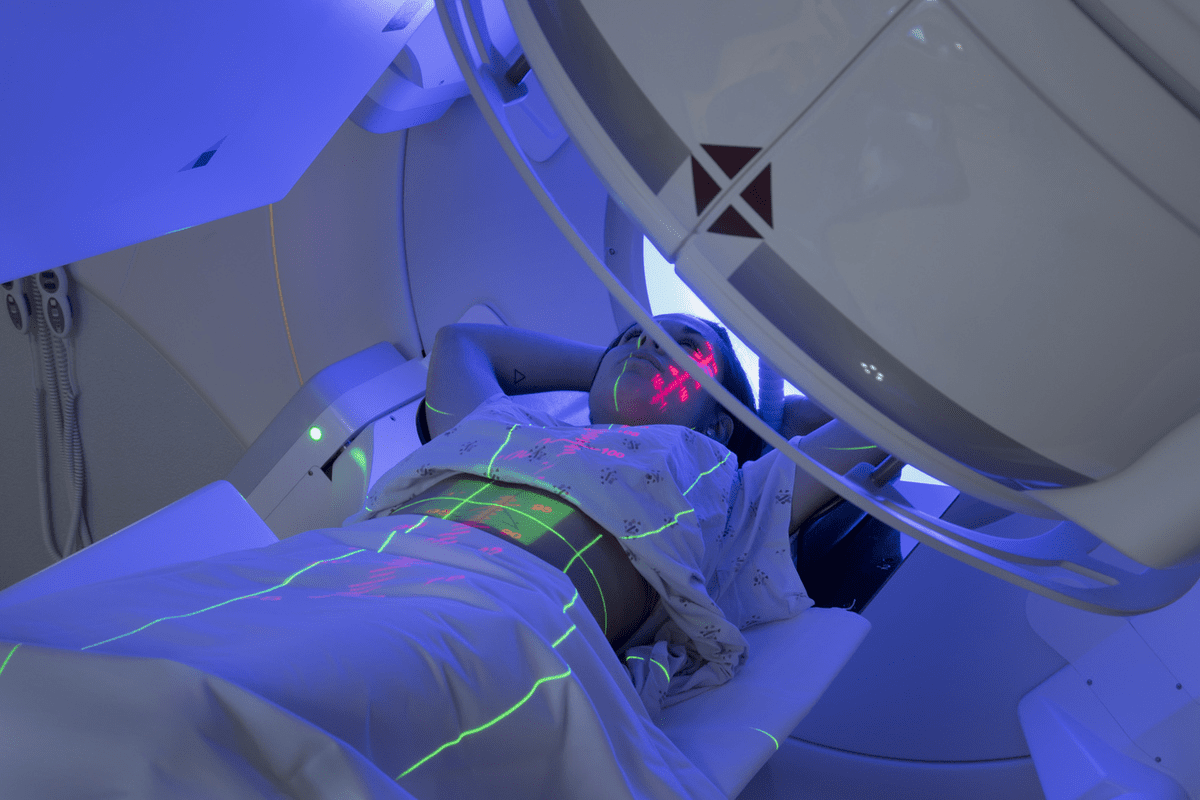
To become a neurointensivist, internal medicine graduates must complete a specialized fellowship. This training in neurocritical care gives them the skills to care for critically ill neurological patients.
ACGME-Accredited Programs vs. Non-Accredited Options
Neurocritical care fellowship programs can be ACGME-accredited or non-accredited. ACGME programs often combine neurocritical care with critical care medicine. For internal medicine graduates, these programs are seen as more prestigious.
However, non-accredited programs, like those from the United Council for Neurologic Subspecialties (UCNS), are also highly valued. They focus specifically on neurocritical care training.
Key differences between ACGME-accredited and non-accredited programs include:
- Curriculum structure and accreditation standards
- Availability of combined training options (e.g., critical care medicine)
- Program duration and flexibility
Application Prerequisites for Internal Medicine Physicians
Internal medicine physicians need to have completed a residency in internal medicine to apply. They may also need training in critical care medicine or neurology. Specific requirements vary by program but usually include:
- Completion of an internal medicine residency program
- Clinical experience in critical care or a related field
- Strong letters of recommendation
- A personal statement outlining career goals and motivation
Typical Fellowship Duration and Structure
Neurocritical care fellowship programs for internal medicine graduates last two years. They include:
- Clinical rotations in neurocritical care and related disciplines
- Didactic sessions and workshops on neurocritical care topics
- Research opportunities to develop academic skills
- Procedural training in neurocritical care techniques
Understanding fellowship training requirements helps internal medicine graduates prepare for a career in neurocritical care.
The Critical Care Medicine Pathway
A high-resolution, photorealistic illustration of the critical care medicine pathway. A detailed diagram depicting the different stages and specializations within the field, showcased in a clean and organized layout. The foreground highlights the key milestones, such as residency, fellowships, and board certifications, using clear icons and concise labels. The middle ground features medical professionals in scrubs and lab coats, engaged in various critical care activities, creating a sense of the clinical environment. The background subtly incorporates hospital architecture, advanced medical equipment, and a soft, warm lighting that enhances the overall professional and authoritative tone.
Internal medicine doctors wanting to focus on neurocritical care have a good option. They can take the critical care medicine pathway. This path includes a CCM fellowship, giving a solid base in critical care. Then, they can specialize in neurocritical care.
Completing CCM Fellowship First
Starting a CCM fellowship is a big step towards neurocritical care. These fellowships offer intensive training in caring for very sick patients, including those with brain issues. Doctors learn to manage complex cases in an ICU.
In a CCM fellowship, doctors learn about hemodynamic monitoring, mechanical ventilation, and managing organ failure. These skills are crucial for neurocritical care. Here, patients often have complex brain and body problems.
Adding Neurocritical Care Training
After a CCM fellowship, doctors can get more training in neurocritical care. They might do a neurocritical care fellowship or join special training programs. This training focuses on neuromonitoring and managing acute brain conditions.
Training in neurocritical care after CCM builds on what doctors already know. It tailors their skills to meet the needs of neurocritical care patients.
Combined Training Programs
Some places offer combined training programs in critical care medicine and neurocritical care. These programs let doctors train in both areas at the same time. This might shorten their training time.
Combined programs are great because they give a complete training experience. They cover critical care basics and the special knowledge needed for neurocritical care. This is good for those wanting to train efficiently and effectively.
UCNS Certification in Neurocritical Care
A neatly organized examination paper with a prominent "UCNS Certification in Neurocritical Care" title on the front page. The pages are crisp and white, with a clean, professional layout. Subtle, warm lighting casts a soft glow over the exam content, which features a mix of multiple-choice questions, short-answer prompts, and clinical case studies relevant to neurocritical care. The paper is set against a slightly blurred background, hinting at the academic environment where this important certification exam would be taken.
For doctors aiming to be top in neurocritical care, getting UCNS certification is key. The United Council for Neurologic Subspecialties (UCNS) offers this. It shows a doctor’s skill in neurocritical care.
Eligibility Requirements for IM Graduates
Internal medicine (IM) doctors wanting UCNS certification in neurocritical care have to meet certain rules. They need to finish a fellowship in neurocritical care or a similar field. They also need a certain amount of clinical experience and to meet specific training needs.
The path to getting certified can differ based on a doctor’s past and training. So, IM doctors should carefully check the UCNS eligibility criteria. This ensures they meet all the needed requirements.
| Eligibility Criteria | Description |
| Fellowship Training | Completion of a neurocritical care or related fellowship program |
| Clinical Experience | A minimum number of years of clinical experience in neurocritical care |
| Training Requirements | Specific training in neurocritical care procedures and management |
Examination Process and Content
The UCNS certification exam in neurocritical care tests a doctor’s knowledge and skills. It covers managing critically ill neurological patients. Topics include neurological assessment, neuromonitoring techniques, and neuropharmacology.
Exam Content: The exam has multiple-choice questions, case studies, and other formats. It checks a candidate’s skill in neurocritical care.
Maintaining Certification
To keep UCNS certification in neurocritical care, doctors must keep learning. They need to do continuing medical education (CME) courses and follow UCNS rules. This keeps their certification active.
Staying Current: Neurocritical care is always changing. Doctors must keep up with new discoveries and best practices.
We advise certified doctors to keep learning and growing. This helps them not only keep their certification but also give the best care to their patients.
Core Competencies in Neurocritical Care
A well-lit surgical suite, with a team of skilled medical professionals intently focused on a patient’s brain. Delicate instruments gently probe neural pathways, monitoring electrical activity and blood flow. Colorful displays provide real-time data, guiding the team’s decisions. Precision and care are paramount, as they work to ensure the patient’s optimal neurological function. The atmosphere is one of quiet intensity, where every detail is meticulously attended to, reflecting the core competencies required in neurocritical care.
In neurocritical care, some skills are crucial for top-notch patient care. Neurointensivists need a wide range of skills to handle critically ill neurological patients well.
Neurological Assessment Skills
Getting a patient’s neurological status right is key in neurocritical care. It’s about checking their consciousness, nerve function, and reflexes. Neurointensivists must know how to do and understand these checks to make the best care choices.
Neuromonitoring Techniques
Neuromonitoring is vital for spotting changes in a patient’s brain and guiding treatment. It includes checking intracranial pressure and using EEG. It’s important to know how these tools work to use them right.
Neuroimaging Interpretation
Imaging is key for diagnosing and managing brain issues. Neurointensivists need to read scans like CTs and MRIs well. Getting these images right is key to spotting serious problems and treating them.
Neuropharmacology Knowledge
Neurocritical care uses medicines to treat brain conditions. Knowing how these medicines work is crucial for the best treatment and to avoid side effects. This includes sedatives and drugs for seizures and blood pressure.
| Core Competency | Description | Clinical Application |
| Neurological Assessment | Evaluating level of consciousness, cranial nerve function, motor and sensory function, and reflexes. | Guiding initial management and ongoing care decisions. |
| Neuromonitoring Techniques | Using ICP monitoring, cerebral blood flow monitoring, and EEG to detect neurological changes. | Detecting and responding to changes in neurological status. |
| Neuroimaging Interpretation | Interpreting CT scans, MRI, and angiography to diagnose neurological conditions. | Identifying life-threatening conditions and guiding treatment. |
| Neuropharmacology Knowledge | Understanding the use of sedatives, anticonvulsants, and vasoactive medications. | Optimizing treatment regimens and minimizing adverse effects. |
Clinical Conditions Managed in Neurocritical Care
Neurointensivists are key in handling critical brain and nervous system issues. We diagnose and treat serious conditions that need quick action.
Acute Stroke Management
Managing acute stroke is a big part of our job. Quick action is vital to lessen brain damage and better patient results. We use treatments like thrombolysis and mechanical thrombectomy to get blood flowing again.
“The timely management of acute stroke is crucial in reducing morbidity and mortality,” as emphasized by leading neurologists in the field.
Traumatic Brain Injury
Traumatic brain injury (TBI) is common in our units. We handle TBI by watching intracranial pressure, keeping blood flow right, and supporting the brain to avoid more damage.
Handling TBI well needs a team effort. This includes neurosurgeons, neurologists, and critical care experts working together.
Status Epilepticus
Status epilepticus is a serious condition with long or repeated seizures. We treat it with a step-by-step plan, starting with benzodiazepines and moving to other drugs if needed.
- Initial treatment with benzodiazepines
- Second-line treatment with antiepileptic drugs
- Third-line treatment with anesthetic agents for refractory cases
Neuromuscular Emergencies
Neuromuscular emergencies, like Guillain-Barré Syndrome and myasthenic crisis, need fast action. We offer support, like breathing help and treatments like plasmapheresis or immunoglobulin, to manage these issues.
Dealing with neuromuscular emergencies requires knowing the disease well and being able to give life-saving care.
Day-to-Day Responsibilities in Neurocritical Care
Being a neurointensivist means a busy day of patient rounds, procedures, and leading a team. This field is tough, needing many skills and quick, smart decisions.
Patient Rounds and Assessment
Patient rounds are key in neurocritical care. Neurointensivists lead these daily sessions. They check on patients, manage their care, and decide on tests or treatments. They look over charts, scans, and lab results to plan treatment.
Good patient care in this field means knowing how to check patients, understand complex data, and use the latest treatments.
Procedural Skills Required
Neurointensivists must know how to do many procedures. This includes lumbar punctures, central line placements, and managing external ventricular drains. These steps are crucial for treating serious brain conditions.
They also need to know how to use advanced tools like transcranial Doppler ultrasonography and EEG for monitoring.
Interdisciplinary Team Leadership
Leading a team is a big part of being a neurointensivist. They work with neurosurgeons, neurologists, nurses, and others to care for very sick brain patients.
Good leadership means clear communication, making quick decisions, and understanding how all parts of care work together.
Teaching and Supervision Roles
Neurointensivists also teach and supervise trainees. They guide, supervise procedures, and promote safe, top-notch care.
By teaching the next generation, they help the field grow and ensure patients get the best care for their brain illnesses.
The Neurocritical Care Society and Professional Resources
The Neurocritical Care Society is key for neurointensivists. It offers many benefits and chances to grow. It has a wide range of resources to help specialists in neurocritical care.
Membership Benefits and Opportunities
Being a member of the Neurocritical Care Society has many perks. You get special educational resources, chances to network, and join special groups. You can also help shape the field by joining committees.
Some main benefits include:
- Discounts on conference registrations
- Access to the Neurocritical Care Journal
- Opportunities for leadership within the society
- Participation in special interest groups
Annual Conferences and Continuing Education
The Neurocritical Care Society holds big conferences every year. These events are where experts share new research and discuss tough cases. You can also learn about the latest in neurocritical care through online courses and webinars.
Neurocritical Care Journal and Publications
The Neurocritical Care Journal is a top publication of the society. It has peer-reviewed articles on the newest research and practices. Members get to read this journal as part of their benefits. The society also publishes guidelines and statements to help professionals.
| Publication | Description | Frequency |
| Neurocritical Care Journal | Peer-reviewed articles on research and clinical practices | Bimonthly |
| Guidelines and Position Statements | Official statements on best practices in neurocritical care | As needed |
The Neurocritical Care Society is crucial for neurointensivists’ growth. It supports their development and moves the field forward.
Strengths Internal Medicine Physicians Bring to Neurocritical Care
Internal medicine physicians have skills that are very useful in neurocritical care. They know a lot about medicine, can handle complex health issues, and focus on the whole body. These skills make them great for this tough field.
Broad Medical Knowledge Base
Internal medicine doctors are trained to deal with many health problems. This broad knowledge is key in neurocritical care. Here, patients often have many complex issues.
Key aspects of their broad medical knowledge include:
- Understanding of various organ systems and their interrelations
- Familiarity with a wide range of medications and their interactions
- Ability to diagnose and manage complex medical conditions
Management of Comorbidities
In neurocritical care, patients often have many health problems. Internal medicine doctors are good at managing these complex cases. They make sure to take care of all parts of a patient’s health.
| Comorbidity | Management Strategy | Importance in Neurocritical Care |
| Hypertension | Careful blood pressure monitoring and management | Critical to prevent further brain injury |
| Diabetes | Tight glucose control | Important for preventing infection and promoting healing |
| Chronic kidney disease | Adjusting medication dosages and monitoring renal function | Essential for avoiding nephrotoxicity and managing fluid balance |
Systems-Based Approach to Care
Internal medicine physicians focus on the whole body when caring for patients. This is very helpful in neurocritical care. Here, the nervous system works closely with other parts of the body.
The systems-based approach involves:
- Coordinating care with multiple specialties
- Understanding the impact of neurological conditions on other organ systems
- Managing the complex interplay between different medical conditions
Challenges for IM-Trained Neurointensivists
IM-trained neurointensivists face a tough path. They must deal with knowledge gaps and competition. Their internal medicine background is strong, but neurocritical care needs more training.
Overcoming Knowledge Gaps in Neurology
One big challenge is filling knowledge gaps in neurology. They need to understand conditions like stroke and brain injuries well. To get better, they often take extra courses or fellowships in neurology.
Here’s a table showing areas where they need to focus:
| Area of Knowledge | Description | Relevance to Neurocritical Care |
| Neurological Assessment | Skills in assessing neurological function and identifying critical conditions | High |
| Neuroimaging Interpretation | Understanding of imaging modalities like CT and MRI in neurological contexts | High |
| Neuropharmacology | Knowledge of medications used in neurological critical care | Medium |
Competing with Traditionally Trained Specialists
IM-trained neurointensivists compete with specialists in neurology or neurosurgery. They must show their strengths, like managing complex health issues and a systems-based care approach.
Establishing Credibility in the Field
Establishing credibility is key for IM-trained neurointensivists. They can do this through education, experience, and joining professional groups like the Neurocritical Care Society. By doing research, presenting at conferences, and publishing, they can earn respect in the field.
Competitive Landscape and Fellowship Application Strategies
Applying for neurocritical care fellowships is getting tougher. As internal medicine residents think about specializing, it’s key to know the competition and prepare well.
Fellowship Application Timeline
The application for neurocritical care fellowships starts a year before you want to start. It’s smart to plan ahead. Mark important dates like when ERAS opens and when applications are due.
| Milestone | Timeline |
| ERAS Registration Opens | June |
| Application Submission Deadline | September |
| Interview Season | October – January |
| Match Day | February |
Strengthening Your Application as an IM Resident
To get noticed, focus on critical care and neurology. Take electives, do research, and go to conferences.
Key areas to focus on:
- Clinical experience in critical care and neurology
- Research and publications related to neurocritical care
- Leadership roles in medical school or residency
- Presentations at national conferences
Interview Preparation and Questions
Getting ready for the interview is crucial. Review common questions, practice your answers, and prepare questions for the panel.
“The best way to predict your future is to create it.” – Abraham Lincoln. This quote fits well with the effort needed for a good interview.
Some common interview questions are:
- Why are you interested in neurocritical care?
- How do you stay current with the latest developments in the field?
- Can you describe a challenging case you managed and how you handled it?
Letters of Recommendation and Personal Statements
Getting strong letters of recommendation and writing a good personal statement are key. Choose recommenders who know you well. They should talk about your skills and achievements.
Your personal statement should show your passion for neurocritical care. It should highlight your experiences and career goals. Make sure to customize it for each program you apply to.
Career Opportunities in Neurocritical Care
Career paths in neurocritical care are wide-ranging and suited to various interests and skills. Neurointensivists can find rewarding roles in many settings. These include academic medical centers, community hospitals, and roles in research and education.
Academic Medical Centers
Academic medical centers combine clinical work, research, and teaching. Neurointensivists here often lead clinical trials, publish studies, and train future doctors. For example, they might work on new stroke treatments and mentor young intensivists.
Community Hospital Settings
Community hospitals are key for local healthcare. Neurointensivists in these places manage urgent neurological cases and lead critical care teams. They work with other healthcare teams to give full care to patients.
Research and Education Roles
Neurointensivists can also focus on research and teaching. They might work in research centers or universities, pushing the field forward with their studies and teaching. These roles are crucial for creating new treatments and training neurointensivists.
Balancing General Critical Care and Neurocritical Care Practice
Neurocritical care often overlaps with general critical care. This creates both chances and hurdles. Many neurointensivists handle both, balancing complex neurological cases with general ICU duties.
Dual Practice Models
Dual practice models let neurointensivists work in both areas. This broadens their skills and variety in work. For example, they might care for stroke patients in a neurocritical unit and general ICU cases the rest of the time.
Maintaining Competency in Both Areas
It’s key to stay skilled in both general and neurocritical care. This means constant learning and updates. Neurointensivists need to know the latest in critical care and neurocritical care.
To keep up, many neurointensivists:
- Go to conferences and workshops in both fields
- Join continuous professional development programs
- Read peer-reviewed journals and publish
Schedule and Lifestyle Considerations
Managing both areas is tough. The hours are long, and the decisions are critical. Work-life balance is crucial.
A comparison of the two practices is shown in the table below:
| Aspect | General Critical Care | Neurocritical Care |
| Patient Profile | Diverse critical care conditions | Complex neurological conditions |
| Skill Set | Broad critical care skills | Specialized neurological assessment and management |
| Workload | Variable, often high volume | Can be high acuity, with complex cases |
Understanding the differences and similarities helps neurointensivists manage dual practice. This way, they can have a rewarding career.
Conclusion: Is Neurocritical Care Right for You After Internal Medicine?
Thinking about neurocritical care after internal medicine? It’s a big decision. You need to think about your career goals, the challenges, and the chances you’ll find. We’ve looked at how to get into this field, like through fellowship training and getting certified.
Internal medicine doctors have a wide range of medical knowledge. This is great for neurocritical care. But, they also need to learn more about neurology and prove themselves in this field.
When deciding, think about what neurointensivists do every day. They handle serious cases and work in different places. We talked about the mix of general and neurocritical care, and the chance to teach and do research.
Neurocritical care can be very rewarding for those who love caring for critically ill patients. Knowing what it takes and what’s available helps you decide if it’s the right path for you.
FAQ
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3117518/
What is neurocritical care, and how does it differ from other critical care specialties?
Neurocritical care focuses on patients with serious brain conditions. It uses a team effort to handle complex cases. It’s different because it focuses on brain and brain surgery patients.
Can internal medicine physicians pursue a career in neurocritical care?
Yes, doctors from internal medicine can move into neurocritical care. They need more training and fellowship programs. Their wide medical knowledge helps them fit well in this field.
What are the traditional pathways to becoming a neurointensivist?
To become a neurointensivist, you can start with neurology, neurosurgery, or anesthesiology. These paths give a strong base in brain and critical care.
What are the fellowship training requirements for internal medicine graduates?
Internal medicine doctors can get fellowship training in neurocritical care. They can choose from ACGME-accredited or non-accredited programs. Training lasts one to two years, with both clinical and research parts.
How can internal medicine physicians obtain UCNS certification in neurocritical care?
Internal medicine doctors need to finish a neurocritical care fellowship. They must also meet certain training needs. Then, they pass the UCNS certification test to show their skills.
What are the core competencies required in neurocritical care?
Key skills in neurocritical care include brain checks, monitoring, reading brain scans, and knowing about brain medicines. These skills are crucial for top-notch care of brain patients.
What clinical conditions are typically managed in neurocritical care?
Neurointensivists handle many conditions, like sudden stroke, brain injury, ongoing seizures, and muscle emergencies. Quick and right action is key for good patient results.
What are the day-to-day responsibilities of neurointensivists?
Neurointensivists do patient checks, perform procedures, lead teams, and teach. They need a lot of skill and leadership to manage tough cases.
What resources are available to neurointensivists through the Neurocritical Care Society?
The Neurocritical Care Society offers many benefits. Members get access to conferences, learning chances, and the Neurocritical Care Journal. These help with growth and networking.
What are the strengths that internal medicine physicians bring to neurocritical care?
Internal medicine doctors have a wide medical knowledge, handle other health issues, and focus on the whole system. These are big pluses for caring for patients with many health problems.
What challenges do internal medicine-trained neurointensivists face?
Internal medicine-trained neurointensivists might face challenges like catching up on neurology, competing with others, and proving themselves. Overcoming these is important for success.
How can internal medicine residents strengthen their fellowship applications?
Internal medicine residents can boost their fellowship chances by getting research experience, getting a strong letter of recommendation, and writing a compelling personal statement. A good application is key to getting a fellowship.
What career opportunities are available to neurointensivists?
Neurointensivists can work in many places, like big hospitals, community hospitals, research, and teaching. They can also lead or manage, based on their interests and skills.
How can neurointensivists balance general critical care and neurocritical care practice?
Neurointensivists can manage both general and brain-focused critical care by using dual practice models. They need to stay skilled in both, considering their schedule and lifestyle. This balance needs careful planning and ongoing learning.