Last Updated on October 22, 2025 by mcelik
Over 32.5 million adults in the United States have osteoarthritis. This is a degenerative joint disease that can really affect how well you live.
Medical imaging is key in finding and tracking this condition. X-rays can spot joint space narrowing and bone spurs. These are signs of osteoarthritis.
Doctors use these images to see how much damage there is in the joints. This helps them create good treatment plans. Knowing how osteoarthritis looks on a scan is important for both diagnosing and managing it.

To understand osteoarthritis, it’s key to see how medical imaging helps in diagnosing it. Osteoarthritis is a complex condition that affects joints. Accurate diagnosis is vital for managing it well.
Osteoarthritis is a degenerative joint disease. It involves the breakdown of cartilage, joint inflammation, and bone spur formation. It can affect any joint but is common in hands, knees, hips, and spine.
The condition causes pain, stiffness, and reduced mobility. This significantly impacts one’s quality of life.
The degeneration of cartilage is a key feature of osteoarthritis. It happens due to joint wear and tear over time. As cartilage wears out, the bone underneath gets affected, leading to bone spurs and cysts. This causes pain and limits joint mobility.
Medical imaging is vital in diagnosing and monitoring osteoarthritis. Techniques like X-rays, MRI, and CT scans give detailed images of joints. These images help healthcare professionals assess joint damage and degeneration.
Imaging tests are essential for seeing the joint structure. They include cartilage, bone, and soft tissues. By analyzing these images, healthcare providers can determine osteoarthritis severity and plan treatment.
Common symptoms that lead to imaging tests for osteoarthritis include joint pain, stiffness, and limited mobility. Swelling and joint deformity also suggest osteoarthritis. When these symptoms appear, healthcare providers often recommend imaging tests to confirm the diagnosis.
The choice to use imaging depends on symptom severity and medical history. By combining clinical evaluation with imaging, healthcare professionals can accurately diagnose osteoarthritis. They can also monitor its progression over time.
X-ray imaging is key in spotting osteoarthritis by showing joint damage. It’s a top choice because it clearly shows bone and joint spaces.
X-rays are great at showing joint damage from osteoarthritis. They capture images of bones and the spaces between them. This lets doctors see how much damage there is. Joint space narrowing and bone spurs are signs of osteoarthritis seen on X-rays.
One key sign of osteoarthritis is joint space narrowing. This can be seen on X-rays. When cartilage wears down, the space between bones gets smaller. X-rays help doctors measure how much narrowing there is, helping with diagnosis and treatment.
Bone spurs, or osteophytes, are abnormal bone growths from osteoarthritis. X-rays can spot these growths, showing how much damage there is. The size and number of bone spurs tell doctors about the osteoarthritis’s stage and severity.
| Osteoarthritis Feature | X-Ray Finding | Clinical Significance |
| Joint Space Narrowing | Reduced space between bones | Indicates cartilage loss and osteoarthritis progression |
| Bone Spurs/Osteophytes | Abnormal bone growths | Signifies joint damage and osteoarthritis severity |
| Sclerosis | Increased bone density | Reflects chronic osteoarthritis and bone remodeling |
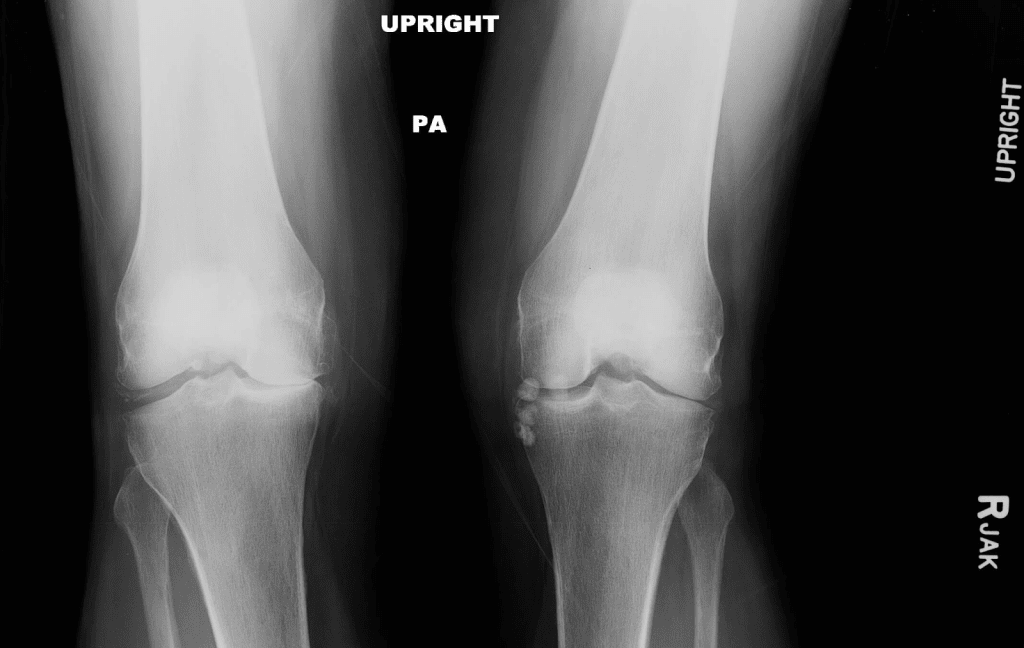
X-ray imaging is key in diagnosing osteoarthritis. But, it needs expert eyes to understand the results. Getting X-ray findings right is vital for knowing how severe osteoarthritis is and what treatment to use.
The Kellgren-Lawrence grading system is a common way to check osteoarthritis on X-rays. It rates osteoarthritis from 0 to 4. A 0 means no osteoarthritis, and a 4 means it’s very severe.
| Grade | Description |
| 0 | No osteoarthritis |
| 1 | Doubtful narrowing of joint space and possible osteophytic lipping |
| 2 | Definite osteophytes and possible narrowing of joint space |
| 3 | Moderate multiple osteophytes, definite narrowing of joints space, some sclerosis and possible deformity of bone contour |
| 4 | Large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone contour |
Kellgren and Lawrence said, “The radiological assessment of osteoarthritis is based on the presence of osteophytes, narrowing of joint space, and other changes such as sclerosis and deformity of bone contour” (
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494-502.
).
X-rays show different things in different joints with osteoarthritis. For example, knee osteoarthritis often shows joint space narrowing, osteophyte formation, and subchondral sclerosis. Hand osteoarthritis might show joint space narrowing, osteophytes, and bony erosions.
In hip osteoarthritis, X-rays usually show joint space narrowing, osteophyte formation, and cyst formation. The Kellgren-Lawrence grading system is used differently for each joint.
X-rays are great for diagnosing osteoarthritis, but they have limits, mainly in the early stages. Early osteoarthritis might not show up on X-rays because it takes a lot of damage to be seen.
“X-ray is not sensitive to early changes in osteoarthritis, as it mainly shows bone changes, not soft tissue changes.” This shows why we need a full diagnostic approach, including other imaging like MRI.
MRI scans are key in checking osteoarthritis, focusing on soft tissues. This advanced imaging shows the joint in detail. It helps doctors see how damaged the joint is and plan the best treatment.
MRI is great for seeing soft tissues like cartilage, ligaments, and tendons. Soft tissue visualization is important for tracking osteoarthritis. MRI’s clear images spot small changes early, helping to act fast.
Cartilage thinning and defects show osteoarthritis. MRI scans spot these changes well. Cartilage thinning MRI shows how much cartilage is lost. This helps doctors decide if surgery or other treatments are needed.
Bone marrow lesions are abnormal spots in the bone marrow, linked to osteoarthritis. These spots can mean inflammation or other issues. Bone marrow lesion detection on MRI is key. It helps in planning treatment and understanding the disease’s progress.
MRI scans give a full view of osteoarthritis. They show soft tissues, cartilage thinning, and bone marrow lesions. This helps doctors make a precise diagnosis and a treatment plan that fits each patient.
CT scans give a detailed look at bone health. They help doctors accurately diagnose osteoarthritis. These scans show the extent of joint damage, helping doctors plan the best treatment.
CT scans are great for catching small changes in bone density. They can spot bone spurs or cysts, common in osteoarthritis. This helps doctors see the bone’s condition clearly.
Bone detail imaging is key for checking the joint’s health. It shows where bones touch each other, a sign of advanced osteoarthritis.
CT scans can create 3D reconstructions. This lets doctors see the joint in three dimensions. It’s very helpful for understanding the joint’s complex anatomy.
3D reconstructions reveal joint damage not seen in 2D images. This gives a fuller picture of the joint’s health.
CT arthrography involves injecting contrast into the joint before scanning. It makes soft tissues like cartilage and ligaments more visible.
This method is great for checking the joint space and finding cartilage defects. It helps spot soft tissue issues linked to osteoarthritis.
| Diagnostic Feature | Description | Clinical Significance |
| Bone Spurs | Abnormal bone growths that can occur in response to joint damage | Indicate advanced osteoarthritis |
| Joint Space Narrowing | Reduction in the space between bones due to cartilage loss | A hallmark of osteoarthritis |
| Cartilage Defects | Damage to the cartilage lining the joints | Can lead to bone-on-bone contact and pain |
Ultrasound technology is key in checking arthritis. It gives real-time views of joint health. Doctors can see how joints move and if they’re inflamed.
Ultrasound is great for checking joints in real-time. Doctors can see how joints move and find any problems.
It’s very helpful for checking hands and feet. These areas often get arthritis. Doctors can see how the disease affects patients’ lives.
Ultrasound is good at finding joint fluid buildup. This is common in arthritis. It shows if there’s inflammation or infection.
| Condition | Ultrasound Findings | Clinical Implication |
| Osteoarthritis | Joint space narrowing, bone spurs | Degenerative changes, possible pain and mobility issues |
| Rheumatoid Arthritis | Joint effusion, synovial thickening | Active inflammation, risk of joint damage |
| Gout | Joint effusion, tophi deposition | Acute inflammation, risk of chronic damage |
Ultrasound has many benefits, like being non-invasive and not using radiation. But, it has downsides. The quality of images and diagnosis depends on the operator’s skill.
Despite these, ultrasound is very useful for arthritis checks. It gives clear images and spots joint fluid buildup. It’s a key tool in rheumatology.
Nuclear medicine imaging, like SPECT and bone scans, gives us a close look at bone activity. This is key for seeing how osteoarthritis is progressing. These methods are great for checking how bones are working, which can show signs of osteoarthritis.
Seeing bone activity through SPECT and bone scans is vital for understanding osteoarthritis. These scans spot changes in bone metabolism early on. They show where bone activity is up or down, giving a clear picture of the disease.
Key Features of Bone Activity Visualization:
Nuclear medicine scans are used when other tests don’t give clear answers. They’re helpful when it’s hard to tell if it’s osteoarthritis or something else. They’re also used when symptoms don’t match what’s expected.
| Condition | Typical Use of Nuclear Medicine Scans |
| Osteoarthritis | Checks disease activity and how it’s changing |
| Inflammatory Arthritis | Helps tell it apart from osteoarthritis by looking at bone activity |
| Bone Metastasis | Finds and tracks bone lesions |
Nuclear medicine scans help tell osteoarthritis apart from other conditions. For example, inflammatory arthritis shows different bone activity patterns. This helps doctors make better diagnoses.
Using nuclear medicine imaging, like SPECT and bone scans, is a big help in fighting osteoarthritis. These scans give detailed info on bone activity. This helps doctors understand the disease better and make the right treatment plans.
Learning about the osteoarthritis scan can help ease worries. This scan helps doctors see how much damage is in your joints. It also helps track how the disease is changing.
Getting ready for an osteoarthritis scan depends on the test type. For X-rays, you don’t need to do anything special. But, for MRI or CT scans, you might need to take off jewelry and wear loose clothes. You might also get a contrast agent to make the images clearer.
| Imaging Test | Preparation Required |
| X-ray | No special preparation needed |
| MRI | Remove jewelry, wear loose clothing, possible contrast agent |
| CT Scan | Remove jewelry, wear loose clothing, possible contrast agent |
When you’re in the scan, you’ll lie on a table that moves into the machine. For MRI scans, it’s important to stay very quiet and not move. The time it takes can vary, with X-rays being the fastest and MRI or CT scans taking longer.
After the scan, you can usually go back to your normal activities unless your doctor says not to. A radiologist will look at the images and send them to your doctor. Then, your doctor will talk to you about what they found and what treatment you might need.
Accurate diagnosis through imaging is key for a good treatment plan for osteoarthritis.
You might need to come back for more tests to check how the disease is doing or if treatment is working. Knowing what to expect can help you feel more ready and less anxious about the scan.
Imaging is key in diagnosing osteoarthritis. Different methods are used for different joints. Each joint needs its own imaging approach for accurate diagnosis and treatment.
X-rays are often used to check knee osteoarthritis. They show joint space narrowing and bone spurs. MRI is also valuable for assessing soft tissue damage and cartilage loss.
A study in a Journal found MRI is very good at spotting early knee osteoarthritis changes.
X-rays are used to check hip osteoarthritis. They look at joint space narrowing and bone spurs. CT scans can provide more detailed images of bone structures.
MRI can check the soft tissues around the hip.Spine and Facet Joint Visualization
X-rays, CT scans, and MRI are used for spine and facet joint osteoarthritis. CT scans are useful for bone structures and detecting osteophytes.
A study in the CT scans have greatly helped in diagnosing and managing spinal osteoarthritis.
X-rays are often used for hand and finger osteoarthritis. They show joint space narrowing and erosions. Ultrasound can also be used to evaluate joint inflammation and soft tissue changes.
In conclusion, different imaging methods are vital for diagnosing osteoarthritis in various joints. The choice of method depends on the joint and the disease’s extent.
Finding osteoarthritis early is vital for effective management. Advanced imaging techniques are key in this early detection. They help in timely intervention and can slow disease progression.
Scans can show early signs of osteoarthritis before symptoms appear. These signs include cartilage loss and bone marrow lesions. Advanced imaging modalities like MRI can spot these changes early.
Seeing these changes early is key for early arthritis detection. It lets healthcare providers act early. This can help delay or lessen the impact of symptoms.
The use of biomarkers and advanced imaging has changed osteoarthritis diagnosis. Biomarkers give insights into the disease’s state and how it might progress. Advanced imaging, like compositional MRI, offers detailed views of joint health.
These advanced imaging techniques help in early detection and monitoring treatment success. They also help understand disease progression at a molecular level.
Imaging is vital for risk assessment in osteoarthritis. It helps identify those at higher risk or with faster disease progression. This info is key for personalized management plans.
Using imaging for risk assessment leads to a proactive approach. It aims to improve outcomes by focusing interventions on those who need them most.
Imaging findings are key in making effective osteoarthritis treatment plans. By linking imaging results with symptoms, doctors can tailor treatments for each patient.
Matching imaging results with symptoms is vital for understanding osteoarthritis. Imaging tools like X-rays, MRI, and CT scans show joint damage. This helps doctors match patient symptoms with the right treatment.
For example, a patient with severe joint damage and pain might need stronger treatment. This is different from someone with less damage and fewer symptoms.
Scan results are essential for planning surgeries, like joint replacements. Imaging shows the extent of joint damage. This helps surgeons choose the best surgery.
| Surgical Procedure | Imaging Modality | Information Provided |
| Joint Replacement | X-ray, CT | Extent of joint damage, bone density |
| Arthroscopy | MRI | Cartilage condition, ligament integrity |
Regular scans help track osteoarthritis progress. Changes in joint damage or bone spurs show if treatment needs to change.
Imaging also checks how well treatments work. For instance, less joint inflammation on MRI means treatment is effective.
Using imaging to guide treatment helps doctors give better care to osteoarthritis patients.
Imaging is key in diagnosing osteoarthritis, but it’s not perfect. Tools like X-rays, MRI, and CT scans give insights into joint health. Yet, they have their flaws.
One big issue is the gap between what imaging shows and how patients feel. Some might have serious joint damage but little pain. Others might be in a lot of pain with only slight damage seen on scans.
“The disconnect between imaging findings and symptoms highlights the complexity of osteoarthritis and the need for a complete diagnostic approach.”
Many things can cause this gap. It includes how people feel pain, other joint issues, and the limits of current imaging tech.
Imaging tests can also be wrong. A wrong positive result might wrongly say someone has osteoarthritis or think it’s worse than it is. A wrong negative result could mean missing the diagnosis.
If imaging doesn’t match symptoms, more tests might be needed. This could include more imaging, arthroscopy, or lab tests to check for other causes.
For example, if X-rays look normal but symptoms suggest osteoarthritis, an MRI might be used. It can spot soft tissue and early cartilage changes not seen on X-rays.
In summary, imaging is vital for osteoarthritis diagnosis, but knowing its limits is key. By understanding the gaps between what imaging shows and symptoms, and the chance of errors, doctors can give better care. This means more accurate and tailored treatment for patients with osteoarthritis.
New methods are being used to look at osteoarthritis in a more detailed way. These methods, like dynamic and functional imaging, give us insights into how joints work and how osteoarthritis progresses. They help doctors see how different parts of the joint work together under different conditions.
Weight-bearing imaging takes pictures of joints when they’re under stress, like when you’re standing. It’s great for checking the space between joints and the thickness of cartilage in places like knees and hips. This way, doctors can see how osteoarthritis affects joints in real life.
The benefits of weight-bearing imaging include:
Motion analysis and stress views show how joints move and how stable they are. For example, stress X-rays can show if a joint is loose or unstable, even if it looks fine in regular pictures.
Key applications of motion analysis include:
Functional MRI (fMRI) looks at how joints function, including inflammation and blood flow. It shows what’s happening inside the joint, helping doctors understand the disease better.
Some of the benefits of fMRI in osteoarthritis assessment include:
In conclusion, new imaging methods are changing how we look at osteoarthritis. They give us a deeper understanding of joint function and disease progression. These methods are set to be key in managing osteoarthritis in the future.
Osteoarthritis imaging is on the verge of a big change. New technologies are coming that will make diagnosing and treating the disease better. These new tools will give us a deeper look into joint health and how the disease progresses.
New MRI methods are being made to check cartilage health. They can spot early signs of cartilage problems. Compositional MRI looks at cartilage thickness, structure, and what it’s made of.
Artificial intelligence (AI) is helping doctors understand medical images better. AI can look through lots of data, find patterns, and see small changes. This means doctors can make more accurate diagnoses and help patients more.
Molecular imaging is being looked at for its ability to find specific signs of osteoarthritis. It can show what’s happening inside the body at a molecular level. This could lead to treatments that are more focused and effective.
New imaging tech is small and can be used in many places, like clinics. This makes it easier to get images taken and get a diagnosis sooner. It’s great for people in areas that don’t have easy access to medical care.
These new technologies are going to change how we deal with osteoarthritis. They will help doctors diagnose and treat the disease better. As these tools get better, they will play a bigger role in helping patients.
New imaging technologies are changing how we diagnose and manage osteoarthritis. Tools like compositional MRI and artificial intelligence help doctors spot the disease early and accurately. This means better care for those affected.
The future of treating osteoarthritis will be more team-based. Doctors will use imaging, clinical checks, and other tools together. This approach will help tailor treatments to each patient’s needs.
Getting osteoarthritis right means accurate diagnosis and regular checks. With new imaging and tech, doctors can offer better care. This will improve life for those with osteoarthritis, shaping the future of their care.
Osteoarthritis is a disease where the cartilage in joints wears down. This leads to inflammation and bone spurs. X-rays, MRI, and CT scans help doctors diagnose and track this condition.
X-rays show joint damage like narrowed spaces and bone spurs. These signs are common in osteoarthritis. Doctors use the Kellgren-Lawrence system to grade the severity seen on X-rays.
MRI scans are great because they show soft tissues like cartilage and ligaments. They can spot cartilage thinning and defects. This gives doctors a clear picture of joint damage.
Yes, CT scans are good at showing bone details. They can spot bone spurs and cysts. Plus, they can create 3D images of the joint.
Ultrasound lets doctors see joints in real-time. They can check for inflammation and fluid buildup. This helps in diagnosing arthritis.
SPECT and bone scans show bone activity. They help detect osteoarthritis, even when other tests are unclear. This is useful for diagnosing the condition.
Scan results help match symptoms with imaging findings. This guides treatment plans. Imaging also helps plan surgeries and track disease progress.
Sometimes, scans don’t match symptoms. False positives and negatives can happen. More tests might be needed to confirm a diagnosis.
New tech includes compositional MRI, AI in image analysis, and molecular imaging. Portable and point-of-care imaging are also being developed. These advancements improve diagnosis and make it more accessible.
Yes, scans can show early signs like cartilage loss and bone marrow lesions. Biomarkers and advanced imaging help catch osteoarthritis early.
Each imaging method has its own strengths and weaknesses. The choice depends on the joint and the osteoarthritis stage. X-rays, MRI, CT scans, and ultrasound are all used for different needs.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!