Last Updated on December 1, 2025 by Bilal Hasdemir

Did you know brain tumors affect thousands in the U.S. each year? A specialized medical facility offers care for patients with these complex conditions.
A neuro-oncology clinic has a multidisciplinary team of experts. They include specialists in cancer treatment options and patient education. Their main aim is to create personalized treatment plans to better patient outcomes and life quality.
Key Takeaways
- Neuro-oncology clinics provide complete care for brain tumor patients.
- A team of specialists staffs these clinics.
- Personalized treatment plans are made for each patient.
- Cancer treatment options are carefully chosen for each patient.
- Patient education is a key part of neuro-oncology care.
Neuro-oncology clinics play a crucial role in the management of brain tumors.
Neuro-oncology clinics play a crucial role in the management of brain tumors. They use a team approach for patient care. These clinics help from the start of diagnosis to after treatment.
Definition and Purpose
A neuro-oncology clinic focuses on brain and spinal cord tumors. Their main goal is to give personalized care to each patient. This ensures the best results for each person.
These clinics have the latest technology and a team of experts. The team includes neurologists, neurosurgeons, and more. They work together to create comprehensive treatment plans for brain tumor patients.
Evolution of Specialized Brain Tumor Care
Neuro-oncology clinics have changed a lot over time. New medical tech, surgery methods, and treatments have improved care. Today, patients get the latest in glioma management and other treatments.
Aspect of Care | Traditional Approach | Neuro-oncology clinics play a crucial role in the management of brain tumors. |
Diagnosis | Limited imaging techniques | Advanced imaging techniques like MRI and PET scans |
Treatment Planning | Less personalized, more generalized treatment plans | Highly personalized treatment plans based on tumor genetics and patient health |
Surgical Techniques | Invasive surgeries with longer recovery times | Minimally invasive surgical techniques and awake brain surgery for better outcomes |
Neuro-oncology clinics now offer specialized treatment thanks to new advancements. This leads to better patient outcomes and quality of life. The growth of these clinics shows a dedication to top-notch, patient-focused care in brain tumor management.
The Multidisciplinary Neuro-oncology Team
A neuro-oncology clinic’s strength comes from its team. This team has many specialists working together. They make sure patients get care that fits their needs.
Key Specialists and Their Roles
The team has several key players. Each one is important for patient care. Here are some of them:
- Neuro-oncologists: These doctors focus on brain tumors. They use treatments like chemotherapy and targeted therapy.
- Neurosurgeons: These surgeons work on the brain and nervous system. They might do biopsies or remove tumors.
- Radiation Oncologists: They use radiation to treat cancer. This includes things like stereotactic radiosurgery.
- Nurses and Nurse Practitioners: These healthcare workers give direct care. They also educate patients and their families.
Support Professionals
Neuro-oncology clinics also have support staff. They are key to patient care. Some of these include:
- Social Workers: They help patients and families deal with the emotional and practical sides of cancer.
- Rehabilitation Specialists: These experts help patients get back their physical and mental abilities after brain tumors or treatment.
- Psychologists and Psychiatrists: They offer mental health support. They help patients with the emotional side of their condition.
These professionals work together. They make sure patients get comprehensive care. This care covers medical, emotional, and practical needs. By teaming up, they create personalized treatment plans. These plans help patients live better lives.
Conditions Treated at Neuro-oncology Clinics
Neuro-oncology clinics offer care for many brain and spinal tumors. They use the latest technology and have teams of experts. This helps meet the complex needs of patients with brain and central nervous system tumors.
Primary Brain Tumors
Primary brain tumors start in the brain and can be either benign or malignant. Gliomas, meningiomas, and medulloblastomas are examples. Treatment plans vary based on the tumor type, grade, and location, and the patient’s health.
Metastatic Brain Tumors
Metastatic brain tumors come from cancer spreading to the brain. They are more common than primary brain tumors. Often, they start from cancers like lung, breast, or melanoma. Treatment includes surgery, radiation, and chemotherapy.
Spinal Cord Tumors
Spinal cord tumors can be inside the spinal cord or in the membranes around it. They can cause pain, weakness, and numbness. Treatment depends on the tumor’s location, type, and the patient’s condition.
Neuro-oncology clinics tailor care to each patient’s needs. This ensures they get the best treatment for their condition.
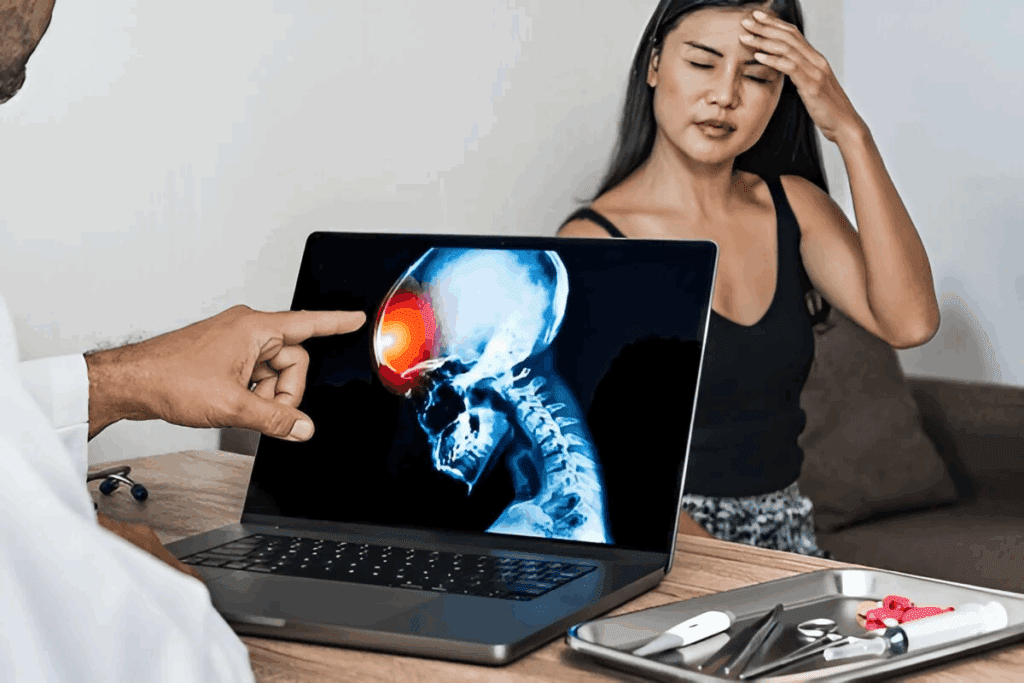
The Diagnostic Process in Neuro-oncology
Getting a correct diagnosis is key in neuro-oncology. It helps doctors create treatment plans that fit each patient. Finding out what kind of brain tumor someone has involves many steps. These include different tests and procedures.
Advanced Imaging Techniques
Advanced imaging is very important in finding brain tumors. MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans are used a lot. MRI is great for seeing soft tissues, while CT scans are quicker and better for bones and calcifications.
“Advanced imaging has changed neuro-oncology a lot,” says a top neuro-oncologist. “It helps doctors diagnose and plan treatments more accurately.”
Biopsy Procedures
Sometimes, a biopsy is needed to confirm a diagnosis. This means taking a piece of tumor tissue for lab tests. There are different biopsies, like stereotactic biopsy and open biopsy. Each has its own reasons and benefits.
- Stereotactic biopsy uses a frame and imaging to find the tumor precisely.
- Open biopsy means opening the skull to get to the tumor.
Molecular and Genetic Testing
Molecular and genetic tests give important details about the tumor. They show things like genetic mutations and markers. This info helps doctors choose the best treatments and predict how well a patient will do. Genetic counseling might also be offered to talk about what these findings mean.
Test Type | Purpose | Benefits |
MRI | Soft tissue characterization | Detailed visualization of tumor extent |
Biopsy | Tissue diagnosis | Confirms tumor type and grade |
Molecular Testing | Genetic mutation analysis | Guides targeted therapy |
Comprehensive Neuro-oncology Care Approaches
Comprehensive neuro-oncology care is a detailed approach for brain tumor patients. It combines many medical specialties. This creates personalized treatment plans for each patient’s unique needs.
Personalized Treatment Planning
Personalized treatment planning is key in neuro-oncology care. It starts with a thorough look at the patient’s tumor and health. This helps create a treatment plan that might include surgery, radiation, or chemotherapy.
- Genetic profiling of tumors to identify targeted therapy options
- Advanced imaging techniques for precise tumor localization
- Consideration of patient comorbidities and preferences
Tumor Board Reviews
Tumor board reviews are vital in neuro-oncology care. These meetings bring together experts from different fields. They discuss complex cases and create collaborative treatment plans.
- Presentation of patient cases by the primary treating physician
- Discussion among specialists to determine the best treatment approach
- Recommendations for additional diagnostic tests or treatments as needed
Integrated Care Coordination
Integrated care coordination ensures patients get complete care. It involves teamwork among healthcare providers. They focus on the patient’s physical, emotional, and social needs.
Key aspects of integrated care coordination include:
- Appointment scheduling and reminders
- Communication between healthcare providers
- Access to support services, such as counseling and rehabilitation
By using a multidisciplinary care approach, neuro-oncology clinics offer top-notch care. This improves outcomes and enhances life quality for brain tumor patients.
Surgical Interventions for Brain Tumors
Neurosurgeons use many surgical interventions to treat brain tumors. Each method has its own benefits and things to consider. The right surgery depends on the tumor’s size, location, and type.
Traditional Neurosurgical Approaches
Traditional surgery involves making a big cut to reach the tumor. This method is good for big or hard-to-reach tumors.
Craniotomy is a key traditional surgery. It involves removing part of the skull to get to the brain. This method has improved a lot and is very important in treating brain tumors.
Minimally Invasive Techniques
Minimally invasive surgery has changed brain tumor treatment. It uses small cuts, causes less damage, and helps patients recover faster. It uses special tools and advanced imaging.
Examples of these techniques include:
- Endoscopic surgery, where tiny cameras and tools are used through small cuts.
- Laser interstitial thermal therapy (LITT), which uses a laser to kill tumor cells.
Awake Brain Surgery
Awake brain surgery keeps the patient awake during parts of the surgery. This lets the team watch brain function live. It helps protect important areas like those for speech and movement.
Surgical Technique | Key Benefits | Typical Applications |
Traditional Neurosurgery | Direct access to tumor, suitable for large or complex tumors | Large or deep-seated brain tumors |
Minimally Invasive Techniques | Smaller incisions, less tissue damage, quicker recovery | Smaller tumors, tumors in sensitive areas |
Awake Brain Surgery | Real-time monitoring of brain function, preservation of critical areas | Tumors near critical brain areas, such as speech or motor centers |
The right surgical intervention depends on the tumor and the patient’s health. Neurosurgery keeps getting better, helping more patients with brain tumors.
Radiation Therapy in Neuro-oncology
Radiation therapy is key in fighting brain tumors. It offers several options for both patients and doctors. It’s often used alone or with surgery and chemotherapy to treat brain tumors well.
External Beam Radiation
External beam radiation therapy (EBRT) is a common treatment for brain tumors. It sends radiation from outside the body to the tumor. EBRT includes techniques like 3D conformal radiation therapy, intensity-modulated radiation therapy (IMRT), and volumetric modulated arc therapy (VMAT).
Benefits of EBRT include precise targeting of tumors and less harm to healthy tissues. This precision helps protect important brain areas.
Stereotactic Radiosurgery
Stereotactic radiosurgery (SRS) is a precise radiation therapy. It delivers a high dose of radiation to a specific area. SRS is not surgery but a non-invasive treatment using multiple beams of radiation.
SRS is very effective for small to medium-sized tumors. It’s great for tumors that are hard to reach surgically or have come back after treatment.
Proton Therapy
Proton therapy uses protons instead of X-rays to kill cancer cells. It’s good for tumors near important structures. This is because it delivers a high dose of radiation to the tumor while protecting healthy tissue.
Radiation Therapy Type | Description | Benefits |
External Beam Radiation | Delivers radiation from outside the body | Precise targeting, minimizes damage to healthy tissues |
Stereotactic Radiosurgery | High dose of radiation to a specific area | Effective for small, well-defined tumors; non-invasive |
Proton Therapy | Uses protons to kill cancer cells | Spares surrounding healthy tissue; ideal for tumors near critical structures |
Guidance in radiation therapy is vital in neuro-oncology. It involves careful planning and execution for the best patient outcomes. The choice of technique depends on the tumor’s type, size, location, and the patient’s health.
Chemotherapy and Drug Treatments
Drug treatments, including chemotherapy, are key in caring for brain tumor patients. They help control tumor growth, ease symptoms, and improve life quality.
Standard Chemotherapy Protocols
Chemotherapy for brain tumors often uses drugs that can get past the blood-brain barrier. Temozolomide is a common drug for glioblastoma.
The right chemotherapy depends on the tumor type, grade, and patient health. Combination chemotherapy may be used to boost treatment results.
Chemotherapy Drug | Tumor Type | Administration Method |
Temozolomide | Glioblastoma | Oral |
Carmustine | Various brain tumors | Intravenous |
Lomustine | Brain tumors, lymphoma | Oral |
Targeted Therapies
Targeted therapies are a new way to fight brain tumors. They aim at specific tumor growth mechanisms. Bevacizumab is used for glioblastoma.
Targeted therapies offer a more focused treatment. This can mean fewer side effects than traditional chemotherapy.
Blood-Brain Barrier Considerations
The blood-brain barrier is a big challenge in treating brain tumors. It blocks many chemotherapy drugs from reaching the tumor.
Scientists are working on new drugs and methods to get around this barrier. They aim to improve drug delivery to the tumor site.
Clinical Trials and Research Opportunities
The field of neuro-oncology is growing fast. This is thanks to many clinical trials and research projects. These efforts help find new treatments for brain tumors.
Current Neuro-oncology Research
Research in neuro-oncology aims to understand brain tumors better. Clinical trials play a big role in this. They test new treatments to see if they work.
Neuro-oncology clinics join big clinical trials. This gives patients access to new treatments. These trials might test new chemotherapy agents, targeted therapies, or other new methods.
Patient Eligibility for Clinical Trials
Who can join clinical trials depends on the study. Researchers help patients and their families understand the process.
Criteria for joining trials include the tumor type and stage, past treatments, and health. Eligible patients might get new treatments that could save their lives.
Accessing Experimental Treatments
Patients can get into clinical trials by talking to their doctor. Neuro-oncology clinics have staff to guide patients through the process.
It’s key for patients to know the risks and benefits of trials. By joining, patients help advance research. They might also get new treatments.
Patient Support Services in Neuro-oncology Clinics
Patient support services are key in neuro-oncology clinics. They meet the emotional, physical, and educational needs of patients and their families. These services aim to improve life quality and offer support during treatment.
Psychological Support
Getting a brain tumor diagnosis is tough emotionally. There are counseling and therapy services to help with anxiety, depression, and other feelings. Professional counselors help patients find ways to cope and offer emotional support.
Rehabilitation Services
Rehabilitation is important for recovery. It helps patients get stronger and more independent. Neuro-oncology clinics offer physical therapy, occupational therapy, and speech therapy to meet each patient’s needs.
Rehabilitation Service | Description | Benefits |
Physical Therapy | Helps improve mobility and strength | Enhances physical function and reduces disability |
Occupational Therapy | Assists with daily living activities | Increases independence and confidence |
Speech Therapy | Addresses communication and swallowing issues | Improves communication skills and reduces risk of aspiration |
Family Resources and Education
It’s important for families to understand the diagnosis and treatment. Neuro-oncology clinics offer family resources and education. This includes workshops, support groups, and materials to help families deal with brain tumor care.
Neuro-oncology clinics provide a wide range of support services. This ensures patients and their families get the care and support they need during treatment.
Managing Neurological Symptoms and Side Effects
Neuro-oncology clinics play a crucial role in the management of brain tumors.
Seizure Management
Seizures are common in brain tumor patients. Anticonvulsant medications are used to manage them. The right medication depends on the tumor type and patient health. It’s important to monitor and adjust the medication to prevent seizures.
Cognitive Changes
Cognitive changes, like memory loss and trouble concentrating, can greatly affect daily life. Cognitive rehabilitation helps patients regain function and adapt to changes.
Physical Limitations
Brain tumors or treatments can cause physical limitations. Physical therapy is key to improve strength and function. Occupational therapy helps with daily activities, keeping patients independent.
Neuro-oncology clinics play a vital role in managing symptoms. They enhance patient care and improve outcomes.
Follow-up Care and Surveillance
Effective follow-up care and surveillance are key for brain tumor patients. They help ensure long-term health and well-being. After treatment, patients need ongoing monitoring and support.
Monitoring for Recurrence
Regular checks for recurrence are vital. This includes MRI or CT scans to spot tumor growth early.
The scan frequency varies based on the tumor type, treatment, and patient risk. For example, those with high-grade gliomas might need scans more often than those with low-grade tumors.
Long-term Survivorship Care
Long-term care focuses on treatment’s late effects. This includes cognitive, physical, and emotional changes. Survivor stories show the journey continues after treatment.
Neuro-oncology clinics offer full care. This includes rehab, psychological support, and education. The aim is to help survivors live their best lives.
Quality of Life Assessments
Quality of life checks are a big part of follow-up care. They help doctors understand treatment’s effects on patients. These assessments guide care plans to meet each patient’s needs.
As
“The care received after treatment is just as important as the treatment itself,”
patient advocates say. This highlights the need for a holistic approach to care. It’s not just about watching for recurrence but also supporting patients’ overall well-being.
Telemedicine is becoming key in neuro-oncology, making it easier for patients to get the care they need. It uses technology to offer healthcare services from a distance. This change is helping neuro-oncology clinics reach more patients.
Virtual Consultations
Virtual consultations let patients talk to doctors from home. This is great for those who can’t easily get to the clinic. It also means fewer hospital visits, which helps avoid infections and reduces stress.
A study found virtual consultations work well for brain tumor patients. They help doctors make quick changes to treatment plans. “
Remote Monitoring Options
Remote monitoring lets doctors keep an eye on patients’ symptoms and side effects as they happen. This helps doctors make quick changes to treatment plans. It also helps patients feel more involved in their care.
Tools like wearable devices and mobile apps help track patients’ health. These tools give doctors important information to make better decisions.
Benefits and Limitations
Telemedicine in neuro-oncology offers many benefits, like easier access to care and happier patients. But, there are challenges too, like technical problems and security worries. Despite these, telemedicine is set to be a big part of neuro-oncology care in the future.
Emerging Trends in Neuro-oncology Treatment
Medical research is leading to new treatments in neuro-oncology. The field is changing fast. New methods are being tested to help patients more.
Immunotherapy Approaches
Immunotherapy uses the body’s immune system to fight cancer. Checkpoint inhibitors and CAR T-cell therapy are being studied for brain tumors. They might offer new hope.
- Checkpoint inhibitors: Drugs that help the immune system fight cancer better.
- CAR T-cell therapy: T-cells are changed to find and kill cancer cells.
Precision Medicine Advancements
Precision medicine means treatments are made just for each patient. Molecular profiling and genetic testing help doctors plan better. This makes treatments more accurate.
- Molecular profiling finds genetic changes that make tumors grow.
- Genetic testing shows inherited traits that affect treatment.
Novel Delivery Methods
New ways to get treatments to brain tumors are being looked into. Convection-enhanced delivery is one. It involves putting drugs right into the tumor or nearby brain.
These new trends in neuro-oncology bring hope to patients with brain tumors. As research keeps going, we’ll likely see even better treatments.
Conclusion
Neuro-oncology clinics are changing how we treat brain tumors. They offer complete cancer care that meets patients’ complex needs. These clinics use a team approach, combining specialists to create personalized treatment plans.
Patient support is key in neuro-oncology care. It helps patients with emotional, psychological, and rehabilitative needs during treatment. This support improves patient outcomes and quality of life.
These clinics stay ahead in neuro-oncology, using new treatments and technology. They provide the best care possible, leading to better treatment results and improved patient care.
FAQ
What is a neuro-oncology clinic, and what services does it provide?
A neuro-oncology clinic offers care for brain tumor patients. It includes diagnosis, treatment, and support. A team of experts, like neuro-oncologists and neurosurgeons, work together here.
What types of brain tumors are treated at neuro-oncology clinics?
These clinics treat many brain and central nervous system tumors. This includes primary and metastatic brain tumors, and spinal cord tumors.
How are brain tumors diagnosed?
Diagnosing brain tumors involves several tests. These include MRI and CT scans, biopsies, and genetic testing.
What is the role of a multidisciplinary team in neuro-oncology care?
The team is key in treating brain tumors. They work together to create personalized treatment plans. This ensures patients get the best care from start to finish.
What are the different treatment options available for brain tumors?
There are many treatments for brain tumors. These include surgery, radiation, chemotherapy, and more. The right treatment depends on the tumor and the patient’s health.
What is the significance of tumor board reviews in neuro-oncology care?
Tumor boards review complex cases. This approach ensures patients get well-rounded care. Treatment plans are made to fit each patient’s needs.
How do neuro-oncology clinics support patients and their families beyond medical treatment?
These clinics offer many support services. They include psychological support, rehabilitation, and education for families. This helps patients and families deal with the emotional and practical challenges of a brain tumor diagnosis.
What is the role of clinical trials in neuro-oncology research?
Clinical trials offer new treatments to patients. They also help researchers find better treatments for brain tumors.
How can patients access clinical trials for brain tumors?
Patients can find clinical trials through neuro-oncology clinics. Each trial has its own rules for who can join.
What are some emerging trends in neuro-oncology treatment?
New trends include immunotherapy and precision medicine. These aim to improve treatment results and patient quality of life.
How can telemedicine be used in neuro-oncology care?
Telemedicine offers remote healthcare services. This includes virtual consultations and monitoring. It makes care more accessible and convenient.
What is the importance of follow-up care and surveillance for patients with brain tumors?
Follow-up care is vital. It helps monitor for recurrence and manage side effects. This improves patients’ quality of life.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10366931/