The hypothalamus is a small but vital part of the brain. It helps keep the body balanced by controlling things like temperature, hunger, and sleep. It also helps the pituitary gland release hormones for growth and reproduction.
When the hypothalamus gets damaged, it can cause many health problems. These can affect growth, fertility, and even how we feel. Knowing about the different types of hypothalamic disorders is key to getting help early.
We will look at the eight main types of hypothalamic disorders. We’ll learn about how they affect this important brain area.
Key Takeaways
- The hypothalamus regulates vital bodily functions, including temperature, hunger, and emotions.
- Damage to the hypothalamus can lead to various health issues, including growth and fertility problems.
- Understanding hypothalamic disorders is critical for early recognition and effective treatment.
- There are eight main types of disorders that can affect the hypothalamus.
- Recognizing the symptoms of hypothalamic dysfunction is essential for timely medical intervention.
The Hypothalamus: Function and Importance

The hypothalamus is key to controlling many body functions. It’s a vital part of our endocrine system. Knowing about hypothalamic diseases and dysfunction helps us grasp its role.
Anatomical Location and Structure
The hypothalamus sits at the brain’s base, below the thalamus. It’s connected to the pituitary gland by a stalk. This area is complex, with different nuclei each having its own job. It’s well-placed to gather and act on information from the brain and body.
Key Regulatory Functions
The hypothalamus makes hormones that control many body functions. These include:
- Body temperature
- Hunger and thirst
- Sleep-wake cycle
- Emotional responses
It also manages the hormonal system by guiding the pituitary gland. This gland releases hormones for growth, reproduction, and thyroid function.
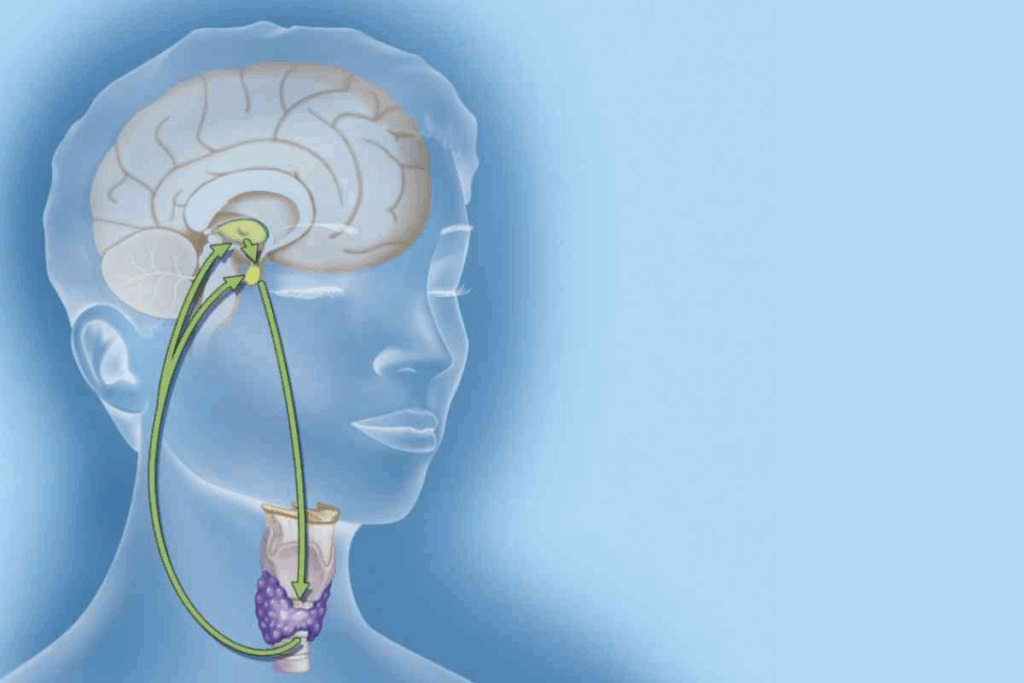
Connection to the Pituitary Gland
The hypothalamus controls the pituitary gland, known as the “master gland.” It does this by making hormones that either help or stop the pituitary gland’s hormone release. This affects many body processes.
| Hypothalamic Hormone | Pituitary Hormone | Function |
|---|---|---|
| TRH | TSH | Regulates thyroid function |
| CRH | ACTH | Regulates adrenal function |
| GnRH | LH, FSH | Regulates reproductive functions |
A study on the hypothalamus found, “The hypothalamus is a critical regulator of the endocrine system, and its dysfunction can lead to a range of health problems” (
This statement highlights the importance of understanding the hypothalamus and its health impact.
Understanding Hypothalamic Disease

Hypothalamic diseases are complex disorders that affect the hypothalamus, a key part of the brain. They regulate various bodily functions. These disorders can cause a wide range of health issues. It’s important to know their definition, classification, prevalence, and how they affect quality of life.
Definition and Classification
Hypothalamic diseases include many disorders, such as hypopituitarism and Prader-Willi syndrome. These conditions disrupt the hypothalamus’s normal function. This leads to hormonal imbalances and metabolic issues. As Medical Expert, “The classification of hypothalamic diseases is based on the underlying causes and the specific functions affected.”
Prevalence and Demographics
The prevalence of hypothalamic diseases varies. For example, hypopituitarism affects about 45.5 people per 100,000. Prader-Willi syndrome occurs in 1 in 15,000 to 1 in 30,000 births. Knowing who is at risk helps in developing targeted treatments.
Impact on Quality of Life
Hypothalamic diseases can greatly affect a patient’s quality of life. Symptoms include excessive thirst, low body temperature, and sleep problems. A study found that patients with these conditions often have a lower quality of life. Effective management is key to improving their well-being.
Understanding these disorders is essential for better patient care. By knowing their definition, classification, prevalence, and impact, healthcare providers can develop effective strategies. This helps improve patient outcomes and overall well-being.
Common Causes of Hypothalamic Dysfunction
It’s important to know what causes hypothalamic dysfunction to manage and treat it well. The hypothalamus controls many body functions and can get damaged in several ways.
Tumors and Space-Occupying Lesions
Tumors, whether they are benign or cancerous, can harm the hypothalamus. Craniopharyngiomas and pituitary adenomas are tumors that can affect it. Surgery or radiation for these tumors can also cause problems.
Traumatic Brain Injury
Traumatic brain injury (TBI) can seriously damage the hypothalamus. Studies show that 27–32% of TBI cases harm the pituitary gland. This can lead to long-term hormonal issues.
Inflammatory and Infectious Processes
Infections and inflammation, like meningitis or sarcoidosis, can harm the hypothalamus. These conditions cause inflammation that can damage the hypothalamus or disrupt its connections.
Genetic and Congenital Factors
Genetic disorders, such as Prader-Willi syndrome, often include hypothalamic dysfunction. Congenital issues can also affect the hypothalamus’s structure and function.
Understanding the many causes of hypothalamic dysfunction is key. It helps healthcare providers create effective treatment plans for each patient. This way, they can address the specific needs of each person.
Hypopituitarism: When the Master Gland Fails
When the pituitary gland doesn’t work right, it can cause hypopituitarism. This condition affects health a lot. It happens when the gland can’t make enough hormones. These hormones help control our body’s functions.
Pathophysiology of Hypopituitarism
Hypopituitarism is when the pituitary gland doesn’t make enough hormones. This can happen for many reasons like tumors or brain injuries. It can also be caused by inflammation or genetic problems.
This problem can make other hormones in the body go out of balance. It’s important to understand why this happens to treat it well.
Clinical Presentation
The symptoms of hypopituitarism can vary a lot. People might feel very tired, gain or lose weight, or have less sex drive. Women might have irregular periods. In serious cases, it can even be life-threatening.
It’s key to notice these symptoms early. This way, doctors can treat it quickly and effectively.
Diagnostic Approach
To diagnose hypopituitarism, doctors check the hormone levels in the body. They use tests and scans to see if the pituitary gland is okay.
We’ll talk about how doctors figure out if someone has hypopituitarism. A table will show the tests used and what they mean.
| Diagnostic Test | Purpose | Interpretation |
|---|---|---|
| Hormone Level Assays | Measure the levels of pituitary hormones | Low levels indicate deficiency |
| MRI of the Pituitary | Identify structural abnormalities | Tumors or damage may be visible |
| Stimulation Tests | Assess the pituitary gland’s response to stimuli | Impaired response indicates dysfunction |
Treatment Strategies
Treating hypopituitarism means giving the body the hormones it needs. This is done through hormone replacement therapy. It’s customized for each person.
We’ll look at the different ways to treat hypopituitarism. It’s important to keep an eye on how well the treatment is working. This can really improve someone’s life.
Neurogenic Diabetes Insipidus
When the hypothalamus fails to make antidiuretic hormone (ADH), it leads to neurogenic diabetes insipidus. This condition makes it hard to control fluids in the body.
Disruption of Antidiuretic Hormone Production
The hypothalamus makes ADH. It then goes to and is released from the posterior pituitary gland. Neurogenic diabetes insipidus happens when ADH production or release is disrupted. This is often due to damage to the hypothalamus or pituitary gland.
This damage can come from many things, like tumors, brain injuries, or inflammation. As a result, the kidneys can’t pull water back into the body. This causes a lot of thirst and urination.
Symptoms and Clinical Features
The main symptoms of neurogenic diabetes insipidus are:
- Excessive thirst
- Frequent urination
- Large volumes of diluted urine
- Dehydration if not managed well
These symptoms can really affect a person’s life. They need careful management to keep fluids balanced.
Differential Diagnosis
To diagnose neurogenic diabetes insipidus, it’s important to tell it apart from other types. A water deprivation test and desmopressin stimulation test can help figure out the cause.
As noted by
“The diagnosis of diabetes insipidus requires a thorough evaluation, including clinical assessment and lab tests.”
Management Options
Managing neurogenic diabetes insipidus usually means using desmopressin, a synthetic ADH. This medicine helps cut down urine production and eases symptoms.
| Treatment | Description | Benefits |
|---|---|---|
| Desmopressin | Synthetic ADH analogue | Reduces urine production, alleviates symptoms |
| Fluid management | Monitoring and adjusting fluid intake | Maintains hydration, prevents dehydration |
Understanding neurogenic diabetes insipidus helps healthcare providers create good treatment plans. This way, they can manage the condition effectively.
Tertiary Hypothyroidism and Adrenal Insufficiency
Understanding how the hypothalamus, pituitary gland, and their target organs work together is key. This knowledge helps in diagnosing and treating tertiary hypothyroidism and adrenal insufficiency. The hypothalamus controls the pituitary gland, which then affects the thyroid and adrenal glands.
Hypothalamic-Pituitary-Thyroid Axis Dysfunction
Tertiary hypothyroidism happens when the hypothalamus doesn’t make enough TRH. This leads to less TSH from the pituitary gland and less thyroid hormone. Causes include tumors, trauma, or inflammation in the hypothalamus.
Hypothalamic-Pituitary-Adrenal Axis Disruption
Adrenal insufficiency due to hypothalamic issues, or tertiary adrenal insufficiency, occurs when the hypothalamus doesn’t make enough CRH. This results in less ACTH from the pituitary gland and less cortisol from the adrenal glands.
Clinical Manifestations
The symptoms of tertiary hypothyroidism and adrenal insufficiency can be hard to spot. They include fatigue, weight changes, and hormonal imbalances. A detailed diagnostic process is needed to identify these conditions.
Treatment Approaches
Treatment for tertiary hypothyroidism and adrenal insufficiency involves hormone replacement. For tertiary hypothyroidism, thyroid hormone is needed. For adrenal insufficiency, glucocorticoids are used. It’s important to monitor and adjust the treatment to manage the conditions well.
| Condition | Cause | Symptoms | Treatment |
|---|---|---|---|
| Tertiary Hypothyroidism | Hypothalamic dysfunction leading to decreased TRH and TSH production | Fatigue, weight gain, cold intolerance | Thyroid hormone replacement |
| Adrenal Insufficiency | Hypothalamic dysfunction leading to decreased CRH and ACTH production | Fatigue, weight loss, hypotension | Glucocorticoid replacement |
Reproductive Disorders: Functional Hypothalamic Amenorrhea and Kallmann Syndrome
The hypothalamus plays a key role in reproductive health. It can lead to conditions like functional hypothalamic amenorrhea and Kallmann syndrome. These issues show how closely the hypothalamus and reproductive system are linked.
Disruption of GnRH Secretion
The hypothalamus controls reproductive functions by releasing Gonadotropin-Releasing Hormone (GnRH). Problems with GnRH can cause reproductive issues. GnRH is important for the pituitary gland to make gonadotropins, which control sex hormones. Any issue here can lead to reproductive problems.
Functional Hypothalamic Amenorrhea
Functional hypothalamic amenorrhea (FHA) is when menstrual cycles stop due to hypothalamic issues. It’s often caused by stress, weight loss, or too much exercise. FHA shows how sensitive the hypothalamic-pituitary-gonadal axis is to stress. It’s diagnosed after other causes of amenorrhea are ruled out.
Kallmann Syndrome Characteristics
Kallmann syndrome is a rare genetic disorder. It causes delayed or no puberty and a poor sense of smell. This happens because of genes that affect GnRH secretion and neuron migration during development. People with Kallmann syndrome need hormone therapy to start puberty and keep their secondary sex traits.
Diagnostic Workup and Management
Diagnosing reproductive issues linked to the hypothalamus involves a detailed check-up, hormone tests, and imaging. Treatment plans are based on the diagnosis and may include hormone therapy, lifestyle changes, and counseling. For FHA, fixing the cause is key. Kallmann syndrome needs ongoing hormone treatment.
Prader-Willi Syndrome: A Complex Genetic Disorder
Prader-Willi syndrome is a genetic disorder that affects the hypothalamus. It requires a detailed management plan. This condition has physical, mental, and behavioral symptoms, mainly because of hypothalamic dysfunction.
Genetic Basis and Hypothalamic Involvement
The genetic cause of Prader-Willi syndrome is the loss of paternal chromosome 15 genes. This loss impacts the hypothalamus’s development and function. The hypothalamus is key in controlling hunger, thirst, and body temperature.
Clinical Features Throughout Life
Prader-Willi syndrome’s symptoms change as people grow. Babies may have low muscle tone and trouble eating. Older kids and adults might eat too much, leading to obesity if not controlled.
Other signs include being short, having low sex hormone levels, and developmental delays. A leading researcher says, “Prader-Willi syndrome is complex. It needs a team effort to manage its many aspects.”
“The management of Prader-Willi syndrome involves a combination of dietary restrictions, behavioral therapy, and hormone replacement therapy to address the various endocrine disturbances.”
Multidisciplinary Management Approach
Managing Prader-Willi syndrome requires a team of experts. This team includes doctors, dietitians, and psychologists. They create a treatment plan tailored to each person’s needs, like diet and hormone therapy.
Long-term Outcomes and Challenges
Outcomes for Prader-Willi syndrome vary based on management. Challenges include fighting obesity, dealing with behavioral issues, and getting the right medical care. Yet, with the right care and support, people with Prader-Willi syndrome can have a good life.
Hypothalamic Obesity and Appetite Dysregulation
Hypothalamic obesity is a complex condition that affects weight regulation. It happens when the hypothalamus, which controls appetite and metabolism, is damaged. This damage can lead to severe obesity.
Mechanisms of Weight Regulation Disruption
The hypothalamus controls weight by balancing hormones like leptin and ghrelin. These hormones tell us when we’re full or hungry. When this balance is off, we might eat more and burn less energy.
Clinical Presentation and Diagnosis
People with hypothalamic obesity often gain weight quickly and feel very hungry. Doctors diagnose it by looking at the patient’s history, doing a physical exam, and using imaging to check for damage to the hypothalamus.
“The diagnosis of hypothalamic obesity requires a high index of suspicion, particular in patients with a history of hypothalamic damage or dysfunction.”
Treatment Challenges
It’s hard to treat hypothalamic obesity because of its complex nature. Traditional weight loss methods often don’t work. So, doctors need to find new ways to help.
| Treatment Approach | Challenges | Potential Solutions |
|---|---|---|
| Dietary Modifications | Poor adherence, increased hunger | Personalized nutrition plans, appetite suppressants |
| Pharmacological Interventions | Limited efficacy, side effects | Novel therapeutic agents, combination therapy |
| Lifestyle Changes | Low motivation, physical limitations | Behavioral therapy, adaptive exercise programs |
Emerging Therapeutic Approaches
Scientists are working hard to find new treatments for hypothalamic obesity. They’re looking at new medicines that target specific parts of appetite and energy balance.
As we learn more about hypothalamic obesity, we can create better treatments. This will help improve the lives of those affected.
Hypothalamic Hamartoma: Rare but Significant
Some people have hypothalamic hamartomas, which are non-cancerous growths. They can cause big problems with the brain and hormones. These growths are found in the hypothalamus, a key part of the brain.
Characteristics and Classification
Hypothalamic hamartomas are known for where they are and what cells they have. They can be attached to the hypothalamus in different ways. Knowing about these hamartomas helps doctors figure out how to treat them.
Neurological and Endocrine Manifestations
Having a hypothalamic hamartoma can cause many symptoms. These include:
- Seizures that don’t respond to medicine
- Hormonal problems because of the hamartoma’s effect on the brain
- Delays in development or problems with thinking in kids
- Behavior issues, like being too aggressive or irritable
Diagnostic Imaging
Imaging tests are key in finding hypothalamic hamartomas. MRI is the best choice because it shows the brain’s soft tissues well.
Treatment Options
Treatment for hypothalamic hamartomas depends on several factors. These include the size, location, and symptoms of the growth. Possible treatments are:
- Medicine to manage seizures and hormone issues
- Surgery, like stereotactic radiosurgery or endoscopic surgery
- Other treatments, like laser ablation or Gamma Knife radiosurgery
Managing hypothalamic hamartomas needs a team effort. This team includes neurologists, endocrinologists, and neurosurgeons. They work together to give care that fits each person’s needs.
Diagnosis and Evaluation of Hypothalamic Diseases
Identifying and treating hypothalamic disorders starts with a detailed diagnostic evaluation. This process uses many tools and techniques. It’s key to finding the right treatment plan.
Clinical Assessment
The first step is a thorough clinical assessment. This involves looking at your medical history and doing a physical exam. Doctors look for signs like changes in appetite, sleep, and hormone levels.
Laboratory Testing
Laboratory tests are vital for diagnosing these disorders. They check hormone levels, like TSH, ACTH, and GH. These tests also look for metabolic issues linked to hypothalamic problems.
Imaging Studies
Imaging, like MRI, is key for seeing the hypothalamus. It helps find tumors, cysts, or inflammation that might be causing problems.
Specialized Endocrine Testing
Special tests are needed to check the hypothalamic-pituitary axes. These tests help diagnose issues like central diabetes insipidus or hypothalamic amenorrhea.
| Diagnostic Tool | Purpose |
|---|---|
| Clinical Assessment | Identify symptoms and signs of hypothalamic dysfunction |
| Laboratory Testing | Assess hormonal levels and metabolic disturbances |
| Imaging Studies (MRI) | Visualize structural abnormalities in the hypothalamus |
| Specialized Endocrine Testing | Assess the integrity of hypothalamic-pituitary axes |
Using these methods, doctors can accurately diagnose and treat hypothalamic diseases. This leads to better health outcomes for patients.
Conclusion: Advances in Management and Future Directions
New hope is on the horizon for those with hypothalamic diseases. Research and new treatments are making a big difference. This is true for both hypothalamic disease and disorders of the hypothalamus.
As we learn more about these diseases, we’re finding new ways to treat them. These new strategies are key to helping patients with hypothalamic dysfunction. They aim to improve patient outcomes.
More research and investment will lead to even better care for patients. This progress is essential for providing top-notch care to those with these disorders.
FAQ
What is the role of the hypothalamus in the body?
The hypothalamus is key to keeping the body balanced. It controls body temperature, hunger, thirst, and hormone levels.
What are hypothalamic diseases?
Hypothalamic diseases are disorders that harm the hypothalamus. This can lead to health problems because of its role in the body.
What causes hypothalamic dysfunction?
Many things can cause problems with the hypothalamus. These include tumors, brain injuries, inflammation, genetics, and birth defects.
What is hypopituitarism, and how is it related to hypothalamic disease?
Hypopituitarism is when the pituitary gland doesn’t make enough hormones. This often happens because of hypothalamic issues. It can cause many health problems.
What is neurogenic diabetes insipidus?
Neurogenic diabetes insipidus is when the body can’t make enough ADH hormone. This is often due to damage to the hypothalamus or pituitary gland. It makes you very thirsty and need to urinate a lot.
How do hypothalamic diseases affect reproductive health?
Diseases of the hypothalamus can mess with hormones that control reproduction. This can lead to problems with menstrual cycles and fertility.
What is Prader-Willi syndrome?
Prader-Willi syndrome is a rare genetic disorder. It affects the hypothalamus and causes problems with appetite, growth, and development. It also affects physical and mental health.
How is hypothalamic obesity diagnosed and treated?
Doctors diagnose hypothalamic obesity by looking at symptoms and testing the hypothalamus. Treatment is hard and needs a team effort. It includes diet, lifestyle changes, and sometimes medicine.
What is a hypothalamic hamartoma?
A hypothalamic hamartoma is a rare, non-cancerous tumor in the hypothalamus. It can cause seizures, hormonal problems, and developmental issues.
How are hypothalamic diseases diagnosed?
Doctors use many tests to find hypothalamic diseases. These include clinical exams, lab tests, imaging, and endocrine tests. They help find the cause and check how the hypothalamus is working.
What are the treatment options for hypothalamic disorders?
Treatment for hypothalamic disorders varies based on the cause. It might include hormone therapy, managing symptoms, surgery, or other specific treatments.
What is the impact of hypothalamic disease on quality of life?
Hypothalamic diseases can greatly affect your life. They can harm your health, mood, and ability to interact with others. Getting the right care and support is very important.
References:
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560743/








