Diabetes affects millions worldwide, with Type 1 and Type 2 being the most prevalent forms. We are facing a global health crisis, with 1 in 9 adults living with this condition. Despite their similarities, these two types of diabetes have distinct physiological mechanisms and require different management approaches.difference diabetes type 1 and type 2Is Back Surgery Dangerous? 12 Major Risks and Complications Explained
Type 1 diabetes is an autoimmune condition where the body’s immune system attacks the insulin-producing beta cells in the pancreas. In contrast, Type 2 diabetes is characterized by insulin resistance, where the body’s cells become less responsive to insulin. Understanding these differences is key for effective management and treatment.
Key Takeaways
- Type 1 diabetes is an autoimmune condition requiring daily insulin administration.
- Type 2 diabetes is mainly caused by insulin resistance.
- Both types need unique management strategies.
- Knowing the differences between Type 1 and Type 2 diabetes is vital for effective treatment.
- The global impact of diabetes calls for awareness and education on its various forms.
Understanding Diabetes: A Global Health Challenge

Diabetes is a growing health crisis worldwide. It affects many people, communities, and healthcare systems. We must understand its impact and how to manage it.
The Growing Prevalence of Diabetes Worldwide
More adults are living with diabetes than ever before. Today, 589 million adults have diabetes. By 2050, this number is expected to reach 853 million. This shows diabetes is becoming more common worldwide.
The rise in diabetes puts a big strain on healthcare. The International Diabetes Federation says,
“The global diabetes epidemic is one of the most significant challenges facing healthcare systems today.”
This challenge affects healthcare costs and quality of life. It’s not just about money; it’s about living well.
Economic and Social Impact of Diabetes
Diabetes has big economic and social effects. It costs a lot to manage diabetes, including medicines and hospital stays. It also affects work and life expectancy.
Diabetes also has a social side. It affects families and caregivers. It can cause stigma and make people feel isolated. We need to tackle diabetes’s social side with education and support.
In summary, diabetes is a big problem worldwide. It affects our economy and society. We must understand its impact to find ways to manage and prevent it.
The Difference Between Type 1 and Type 2 Diabetes Explained
Diabetes is not just one disease. It’s actually two different conditions: Type 1 and Type 2. Knowing the difference is key to managing and treating them well.
Insulin Production vs. Insulin Resistance
Type 1 diabetes happens when the body’s immune system attacks and destroys the insulin-making cells in the pancreas. This leads to a complete lack of insulin production. On the other hand, Type 2 diabetes is caused by insulin resistance. This means the body’s cells don’t respond well to insulin, and the pancreas may not make enough insulin over time.
Understanding the difference between insulin production and insulin resistance is vital. People with Type 1 diabetes need insulin to live, while those with Type 2 may start with lifestyle changes and medications. Insulin therapy might be added later for Type 2 diabetes.
Autoimmune vs. Metabolic Disorder
Type 1 diabetes is an autoimmune disease. The body’s immune system attacks its own cells. Type 2 diabetes, on the other hand, is a metabolic disorder. It’s caused by insulin resistance and poor insulin secretion.
Type 1 diabetes is not preventable with today’s medicine. But Type 2 diabetes can be prevented or delayed with diet and exercise.
Onset and Progression Patterns
Type 1 diabetes can start quickly, with symptoms appearing in weeks. It often shows up in kids or teens, but can happen at any age. Type 2 diabetes, though, develops slowly over years. Many people don’t show symptoms until the disease is far along. It’s more common in adults, but is also rising in kids and teens, linked to obesity.
It’s important for doctors to know how Type 1 and Type 2 diabetes start and progress. Early diagnosis and the right treatment can greatly improve life for those with diabetes.
Type 1 Diabetes: The Autoimmune Condition
Type 1 diabetes is an autoimmune disease. It happens when your body’s immune system attacks the insulin-making cells in your pancreas. This is due to a mix of genetic and environmental factors.
How Type 1 Diabetes Develops
Getting type 1 diabetes involves genetics and environmental factors. Genetic factors increase your risk, but they’re not the only cause. Environmental triggers, like viruses, also play a part.
When someone with a genetic risk meets an environmental trigger, it can start an autoimmune attack. This attack damages the pancreas, leading to a lack of insulin.
Genetic and Environmental Factors
Research is ongoing to understand how genetics and environment interact in type 1 diabetes. Some genes are linked to a higher risk. Viral infections, like coxsackievirus B, might start the autoimmune process.
- Genetic Markers: Certain HLA genotypes are associated with an increased risk.
- Environmental Triggers: Viral infections may trigger the autoimmune response.
Who Is Most at Risk for Type 1 Diabetes
Anyone can get type 1 diabetes, but some are at higher risk. If your family has it, you’re more likely to get it. People of European descent also face a higher risk.
Knowing who’s at risk helps us catch type 1 diabetes early. We can then manage it better and improve outcomes.
Type 2 Diabetes: The Progressive Metabolic Disorder
Type 2 diabetes is a metabolic disorder linked to lifestyle and genetics. It’s marked by insulin resistance and poor insulin production, causing high blood sugar.
The Development of Insulin Resistance
Insulin resistance is key in Type 2 diabetes. It happens when cells don’t respond well to insulin, making it hard for glucose to get in. The pancreas then makes more insulin, but can’t keep up, leading to high blood sugar.
Insulin resistance is linked to obesity, physical inactivity, and an unhealthy diet. It’s also influenced by genetics, with some genes making it more likely.
Risk Factors for Type 2 Diabetes
Several factors increase the risk of Type 2 diabetes. These include:
- Family history: Having a relative with Type 2 diabetes raises your risk.
- Obesity: Being overweight, with belly fat, is a big risk factor.
- Physical inactivity: A sedentary lifestyle leads to insulin resistance.
- Unhealthy diet: Eating too much fat, sugar, and salt increases risk.
- Age: Risk grows with age, after 45.
- Ethnicity: Some groups, like African Americans and Hispanics/Latinos, face higher risks.
Preventable Aspects of Type 2 Diabetes
While some factors can’t be changed, many can be through lifestyle changes. These include:
- Lifestyle changes: Regular exercise, a healthy weight, and balanced diet can lower risk.
- Dietary modifications: Eating more fruits, veggies, whole grains, and lean proteins helps manage blood sugar.
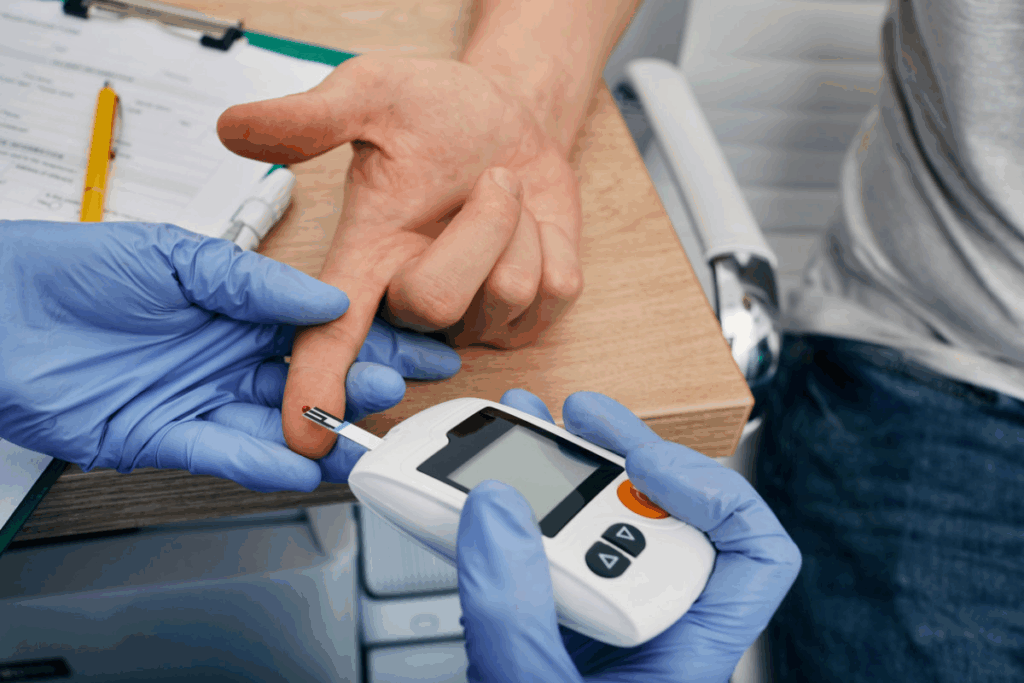
- Monitoring and management: Regular health checks and blood sugar monitoring can catch problems early.
Understanding Type 2 diabetes can help us prevent or manage it. This improves life quality for those affected.
Comparing Symptoms: How Each Type Manifests
It’s key to know the different symptoms of Type 1 and Type 2 diabetes to get help fast. Both types have some symptoms in common, but they also have big differences. These differences can affect how you’re diagnosed and treated.
Common Symptoms in Both Types
Both types show symptoms like increased thirst and urination because of high blood sugar. Other common signs are fatigue, blurred vision, and slow healing of cuts and wounds. These happen because high blood sugar makes it hard for the body to work right.
Unique Symptom Patterns in Type 1 vs. Type 2
Type 1 diabetes comes on fast, with symptoms appearing quickly. This is because the body suddenly stops making insulin. You might see rapid weight loss and flu-like symptoms.
Type 2 diabetes might not show symptoms for years, with them coming on slowly. Signs of Type 2 include tingling or numbness in hands and feet and recurring skin, gum, or bladder infections.
When to Seek Medical Attention
If you notice any diabetes symptoms, see a doctor right away. Early treatment can greatly improve your health. If you have a family history of diabetes or are at risk, watch your health closely.
See a healthcare professional if you notice any unusual changes in your body, and you’re at risk for diabetes. Getting help quickly can really help manage your condition.
Age of Onset: When Each Type Typically Appears
Type 1 and Type 2 diabetes can start at different ages, changing how we see these diseases. While some ages are more common for each type, the truth is more complex.
Beyond the “Juvenile Diabetes” Label
Type 1 diabetes used to be called “juvenile diabetes” because it often started in kids. But now, we know it can start at any age. Many adults are getting Type 1 diabetes, a condition called LADA.
Studies show Type 1 diabetes is happening more often in all ages, not just kids. Doctors need to think about Type 1 diabetes for adults with diabetes symptoms too.
The Shifting Demographics of Type 2 Diabetes
Type 2 diabetes used to mainly affect adults. But now, it’s being seen in kids and teens more often. This is because of more childhood obesity and less exercise.
This is worrying because Type 2 diabetes in young people can last longer. It can cause more serious problems later in life. So, it’s key to prevent it and treat it early.
Late-onset Type 1 and Early-onset Type 2: A Changing Landscape
The line between Type 1 and Type 2 diabetes based on age is getting fuzzy. We see late Type 1 diabetes and early Type 2 diabetes more often.
“The changing epidemiology of diabetes requires a nuanced understanding of the disease beyond traditional age-related categorizations.” – Medical Expert, Diabetes Researcher
A study looked at when Type 1 and Type 2 diabetes start. It found big differences. Here’s a summary:
Type of Diabetes | Typical Age of Onset | Possible Age Range |
Type 1 | Childhood to early adolescence | Any age |
Type 2 | Adulthood | Children to elderly |
It’s important to understand these changes for better diagnosis and treatment. As diabetes demographics change, so must our approach to it.
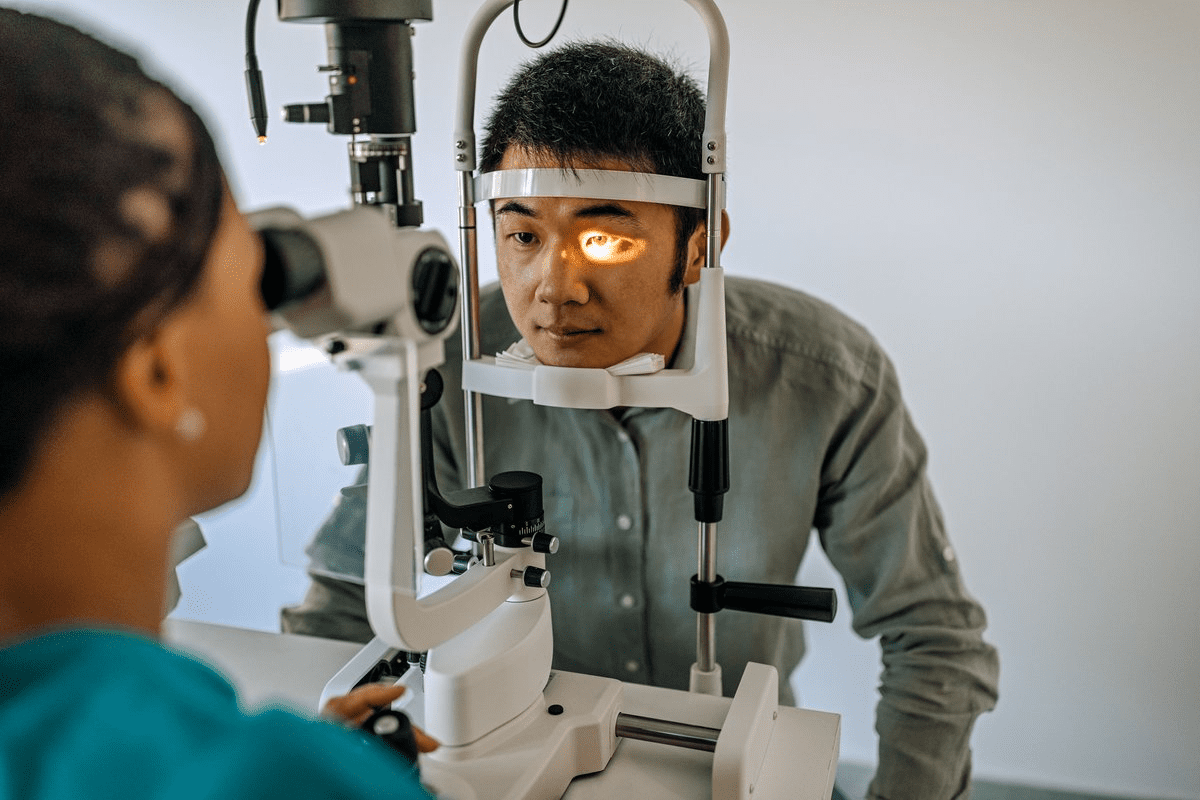
Diagnostic Approaches for Type 1 and Type 2 Diabetes
Diagnosing diabetes requires both clinical checks and lab tests. We’ll look at how to tell Type 1 from Type 2 diabetes.
Blood Tests and Biomarkers
Blood tests are key in finding diabetes. They check blood sugar levels, important for both types. Main tests include:
- Fasting Plasma Glucose (FPG): Checks blood sugar after not eating overnight.
- Oral Glucose Tolerance Test (OGTT): Sees how well the body handles sugar after drinking a sweet drink.
- Hemoglobin A1c (HbA1c): Shows average blood sugar levels over 2-3 months.
Tests for biomarkers like autoimmune antibodies also help tell Type 1 from Type 2 diabetes.
Distinguishing Between Types During Diagnosis
Telling Type 1 from Type 2 diabetes can be hard because symptoms are similar. But, some tests and signs can help:
Diagnostic Feature | Type 1 Diabetes | Type 2 Diabetes |
Autoimmune Antibodies | Often present (e.g., GAD, IA-2) | Typically absent |
Age of Onset | Usually in children and young adults | More common in adults, but increasingly seen in younger individuals |
Insulin Levels | Low or absent | Variable, often with insulin resistance |
Doctors use these clues to make a correct diagnosis.
Challenges in Accurate Diagnosis
Even with better tests, it’s hard to tell Type 1 from Type 2 diabetes. Challenges include:
- Overlapping Symptoms: Symptoms of both types can be similar, making it hard to tell them apart.
- Age and Presentation: Type 1 is now seen in adults, and Type 2 in the young, making age less of a clue.
- Co-existing Conditions: Other health issues can make diagnosis harder.
Treatment Strategies: Managing Each Type Effectively
It’s important to know how to treat Type 1 and Type 2 diabetes differently. Both types need careful management, but the methods can vary a lot.
Insulin Therapy: Essential for Type 1, Sometimes for Type 2
People with Type 1 diabetes need insulin therapy because their bodies can’t make insulin. They use injections or an insulin pump to help glucose get into cells. Those with Type 2 diabetes might start with lifestyle changes and pills, but could need insulin as their disease gets worse.
We’ll look at the different types of insulin, like rapid-acting and long-acting. The right insulin plan depends on your lifestyle, blood sugar checks, and health issues.
Medication Options for Type 2 Diabetes
Type 2 diabetes treatment often starts with lifestyle changes. But if these don’t work, medicines are needed. There are many oral and injectable medicines for Type 2 diabetes, each lowering blood sugar in its own way.
- Metformin is often the first choice, as it lowers liver glucose production.
- Sulfonylureas make the pancreas release more insulin.
- DPP-4 inhibitors help keep insulin production going and lower liver glucose.
- SGLT2 inhibitors stop the kidneys from taking glucose back into the blood, helping it get into urine instead.
The Role of Lifestyle Modifications
Lifestyle changes are key for managing both Type 1 and Type 2 diabetes. Dietary changes, physical activity, and weight management can greatly affect blood sugar and health.
For Type 2 diabetes, lifestyle changes are often the first step. Even if you’re on medication or insulin, a healthy lifestyle can help you need less medicine and control your diabetes better. It’s best to work with a healthcare provider to create a plan that includes diet advice and exercise tailored to you.
Special Populations and Diabetes Management
Managing diabetes in special groups like children, teens, pregnant women, and the elderly is complex. Each group has unique needs that require a tailored approach to care.
Children and Adolescents with Diabetes
Diabetes in kids and teens needs a plan that fits their growth and lifestyle. Insulin therapy is key, and it must be flexible for diet and activity changes. It’s also important to support their mental health to help them manage diabetes well.
“Diagnosing diabetes in kids is a big change that needs constant education for the child and their family,” experts say. This education is critical for managing diabetes effectively.
Diabetes in Pregnancy: Gestational and Pre-existing
Diabetes in pregnancy is risky for both mom and baby if not managed well. Gestational diabetes mellitus (GDM) is when blood sugar levels are high during pregnancy in women without diabetes before. Keeping blood sugar in check is key to avoid problems.
- Regular monitoring of blood glucose levels
- Dietary adjustments to manage carbohydrate intake
- Insulin therapy when necessary
For women with diabetes before pregnancy, managing blood sugar is even more critical. This helps protect the baby and mom from complications.
Elderly Patients with Diabetes
Elderly people with diabetes often face more health issues and take many medications. This makes managing diabetes harder. We aim to simplify treatment and teach self-care to improve health.
Research shows, “Older adults with diabetes are at higher risk for losing function, memory problems, and frailty.” So, a detailed diabetes care plan is vital for this group.
Complications: Long-term Health Risks in Both Types
Diabetes can lead to serious health problems over time. Both Type 1 and Type 2 diabetes can cause big issues if not managed well.
Cardiovascular Complications
Heart disease is a big risk for people with diabetes. It can cause heart attacks, strokes, and problems with blood flow. High blood glucose levels can harm blood vessels and heart nerves.
People with diabetes face a higher risk of heart problems. This is because of high blood pressure and bad cholesterol. It’s important to manage these with lifestyle changes and medicine.
Microvascular Complications
Diabetes can damage small blood vessels. This leads to problems like kidney damage, nerve damage, and eye damage.
Kidney damage from diabetes can lead to kidney failure. Early detection and management are key to stopping it from getting worse.
Risk Profiles: Similarities and Differences
Both types of diabetes have common complications. But, their risk levels are different. Type 1 diabetes often starts earlier and lasts longer.
Type 2 diabetes is often linked with obesity and high blood pressure. Knowing these differences helps doctors create better treatment plans. This can lower the risk of long-term problems.
Is One Type “Worse” Than the Other? Addressing Common Misconceptions
Diabetes affects millions globally, coming in two main types. Each type has its own set of challenges. The debate between Type 1 and Type 2 diabetes often leads to misunderstandings about their severity and how they affect people’s lives.
Comparing Severity and Prognosis
Looking at the severity of Type 1 and Type 2 diabetes, we must consider their prognosis. Type 1 diabetes is an autoimmune disease where the body attacks insulin-producing cells. This requires a lifetime of insulin therapy.
Type 2 diabetes is linked to insulin resistance and impaired insulin secretion. It’s often caused by lifestyle and genetics. Both types need careful management, but their effects and progression can differ greatly.
Quality of Life Considerations
The quality of life for those with diabetes depends on several factors. These include the type of diabetes, how well it’s managed, and overall health. For Type 1 diabetes, managing insulin and glucose levels can be tough.
Type 2 diabetes requires lifestyle changes and, sometimes, medication. But, if not managed well, it can lead to serious complications.
The Individualized Nature of Diabetes Impact
The impact of diabetes varies from person to person. Factors like health, treatment adherence, and healthcare access greatly affect quality of life and prognosis.
Both Type 1 and Type 2 diabetes need tailored care and management. By understanding the unique aspects of each type and the experiences of those with diabetes, we can improve outcomes and quality of life for all.
Conclusion: Living Well With Either Type of Diabetes
We’ve looked into the unique traits of Type 1 and Type 2 diabetes. We’ve seen how they differ in causes, symptoms, and how to manage them. Good diabetes care is key for those with either type, helping them live fully and actively.
Managing diabetes needs a full plan, including the right treatment and lifestyle changes. Knowing what your diabetes needs helps you take better care of yourself. This way, you can make smart choices for your health.
Living with diabetes means being proactive about your health. With the right care and support, you can lower the risk of serious problems. We urge those with diabetes to team up with doctors to create a care plan that fits them.
FAQ
What is the main difference between Type 1 and Type 2 diabetes?
Type 1 diabetes is when the body attacks its own insulin-making cells. Type 2 diabetes is when the body doesn’t use insulin well and makes less of it over time.
Is Type 1 diabetes worse than Type 2 diabetes?
Both types of diabetes have their own challenges. The impact of diabetes varies based on health, lifestyle, and how well it’s managed.
What are the common symptoms of Type 1 and Type 2 diabetes?
Common symptoms include thirst, urination, fatigue, blurred vision, and slow healing. Type 1 diabetes often has more severe symptoms like rapid weight loss and ketoacidosis.
Can Type 2 diabetes be prevented?
While some risk factors can’t be changed, many can be managed. This includes eating well, staying active, and keeping a healthy weight.
How is diabetes diagnosed?
Diabetes is diagnosed with blood tests like fasting plasma glucose and hemoglobin A1c (HbA1c). Doctors also look at symptoms and medical history.
What are the treatment options for Type 1 diabetes?
Insulin therapy is key for Type 1 diabetes. Treatment plans include insulin injections or pumps, along with monitoring blood sugar levels.
Can lifestyle changes help manage Type 2 diabetes?
Yes, lifestyle changes are vital for Type 2 diabetes. Eating well, staying active, and managing weight can improve insulin sensitivity and glucose control.
Are there any differences in the complications associated with Type 1 and Type 2 diabetes?
Both types face similar risks like heart disease, kidney damage, and nerve damage. But, the risk and rate of these complications can differ.
How does diabetes affect different age groups?
Diabetes management changes with age. Children, teens, pregnant women, and the elderly face unique challenges and considerations.
Is it possible to live well with diabetes?
Yes, with the right care and management, people with diabetes can live active and fulfilling lives. Education and support are key to good health outcomes.
References
World Health Organization. Type 1 vs. Type 2 Diabetes: Key Differences. Retrieved from
https://www.who.int/news-room/fact-sheets/detail/diabetes