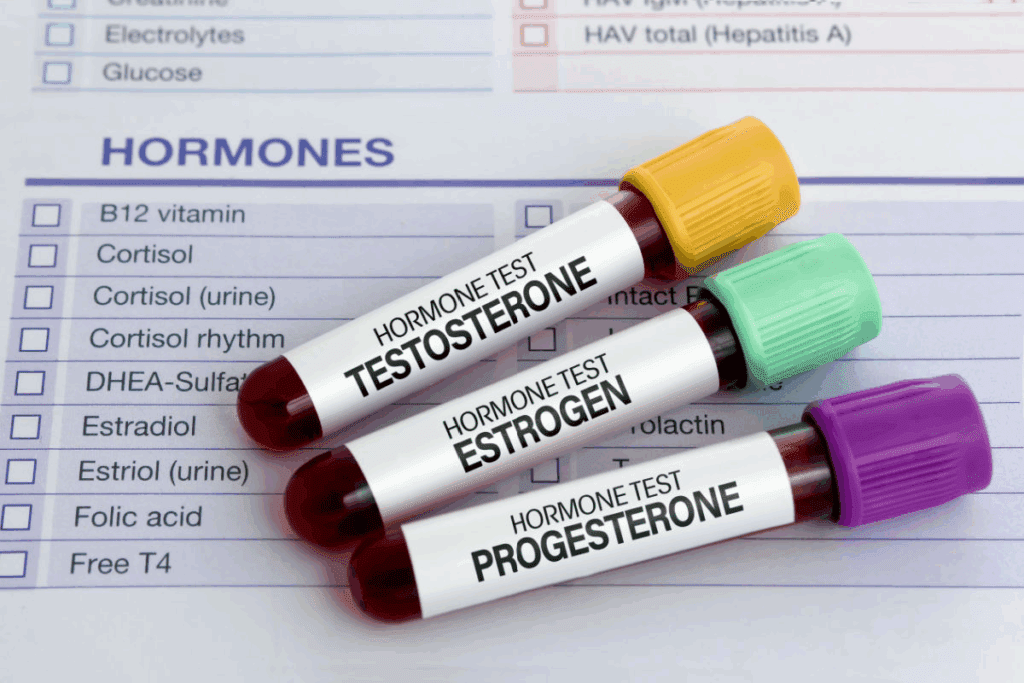
Hormone Replacement Therapy (HRT) helps manage menopause symptoms by adding hormones that decrease with age. At Liv Hospital, we focus on choosing the right patients and tailoring hormone doses for each one.
Find the key lowest dose of progesterone for hrt (Hormone Replacement Therapy). Learn about dosage guidelines and contraindications immediately.
Menopausal hormone therapy (MHT) is key for treating hot flashes and vaginal dryness. It’s also used to prevent and treat bone loss in younger postmenopausal women.
Knowing how progesterone works in HRT is important. It helps balance the risks of estrogen therapy. We’ll look at the key contraindications to HRT and the lowest effective dose of progesterone for HRT.
Key Takeaways
- HRT is a critical treatment for managing menopausal symptoms.
- Progesterone plays a key role in HRT by reducing risks from estrogen therapy.
- Choosing the right patients is vital for safe HRT use.
- Customizing hormone doses is necessary for the best results.
- Knowing the HRT contraindications is important to avoid risks.
Understanding Hormone Replacement Therapy (HRT)

Hormone Replacement Therapy (HRT) is a big help for many women during menopause. It’s key to know what HRT is, how it works, and the hormones it uses.
What is HRT and How Does it Work?
HRT is a treatment that helps with menopause symptoms. It adds hormones that the body doesn’t make enough of anymore. The main goal is to balance hormones and lessen symptoms like hot flashes and vaginal dryness.
Guidelines say to start with the lowest dose of progesterone. This helps avoid side effects while managing symptoms well.
“Menopausal Hormone Therapy (MHT), which includes HRT, is the most effective treatment for hot flushes and night sweats, and it also effectively treats vaginal dryness.”
Types of Hormones Used in HRT
HRT uses estrogen and progesterone. Estrogen helps with vaginal dryness and hot flashes. Progesterone protects the uterus from estrogen’s effects, for women with a uterus.
The choice of hormones depends on a woman’s health and history. Customizing HRT is important for the best results and safety.
Knowing about the hormones in HRT helps women choose their treatment. It’s a detailed process, but with the right advice, women can handle menopause better.
The Role of Progesterone in HRT
For women on HRT, progesterone is key to avoiding estrogen’s risks. It balances estrogen’s effects on the uterus.
Protective Function for Women with Intact Uterus
Women with a uterus need progesterone in their HRT. It stops estrogen from making the endometrium grow too much. Without progesterone, estrogen can cause endometrial hyperplasia and cancer. Progesterone stops this by making the endometrium grow normally and preventing bad cell growth.
Balancing Estrogen Effects on Endometrium
Adding progesterone to HRT balances estrogen’s effects on the endometrium. This balance is key to stop endometrial hyperplasia. It includes:
- Regulating endometrial growth
- Encouraging endometrial differentiation
- Lowering estrogen’s growth effect
Reducing Risk of Endometrial Hyperplasia
Progesterone’s main role in HRT is to lower endometrial hyperplasia risk. It stops estrogen’s growth effects, keeping the endometrium healthy. The benefits are:
- Less chance of endometrial cancer
- Stopping abnormal bleeding
- Keeping the endometrium healthy
Understanding progesterone’s role in HRT helps doctors tailor treatments. This is important for women with an intact uterus.
The Lowest Dose of Progesterone for HRT: Clinical Guidelines
When starting hormone replacement therapy (HRT), finding the right amount of progesterone is key. It helps avoid unwanted side effects. Clinical guidelines help doctors choose the best dose for each patient.
The aim is to use the least amount needed to work well. This lowers the chance of bad reactions. It’s very important for women on HRT to avoid risks.
Standard Starting Doses (100-200mg)
Most women start with 100 to 200 milligrams of oral micronized progesterone daily. This dose works well for many.
The estrogen dose depends on how a woman feels and her health. It’s not just about blood tests. This shows the need for personalized care in HRT.
Individualized Dosing Considerations
While starting doses are a guide, each woman’s needs are different. Her medical history, age, and symptoms play a big role in finding the right dose.
Women with certain health issues might need different doses. Doctors must look at each case carefully to find the best plan.
Bioavailability Factors
Bioavailability is also key when picking the lowest effective progesterone dose. It changes based on how the progesterone is made and given.
Oral micronized progesterone works well and is often chosen for HRT. Knowing about bioavailability helps doctors make better choices for dosing.
Progesterone Administration Methods and Dosing Protocols
Choosing the right way to give progesterone is key for Hormone Replacement Therapy (HRT). How you give progesterone can really affect how well it works.
Oral Micronized Progesterone Dosing
Oral micronized progesterone is a popular choice. It usually comes in doses of 100 to 200 milligrams a day. It’s often given in a cycle.
When using this type of progesterone, think about how well it’s absorbed and what each patient needs.
Cyclic Regimens (12-14 Days Monthly)
Cyclic regimens give progesterone for 12 to 14 days each month. This helps to mimic the natural cycle and lower the risk of endometrial hyperplasia.
- Progesterone doses in cyclic regimens usually range from 200 milligrams daily.
- This is good for women in the early stages of menopause.
- It helps manage symptoms and regulate menstrual bleeding.
Continuous Combined Therapy Options
Continuous combined therapy gives both estrogen and progesterone every day. It’s often suggested for postmenopausal women.
The benefits include:
- Lower risk of endometrial cancer
- Good management of menopausal symptoms
- No menstrual bleeding over time
Healthcare providers weigh many factors when deciding between cyclic regimens and continuous combined therapy. They look at the patient’s menopausal status, medical history, and what they prefer.
7 Critical Contraindications to Hormone Replacement Therapy
Before starting Hormone Replacement Therapy (HRT), it’s key to know the serious reasons why it might not be safe. HRT helps with menopause symptoms by adding hormones. But, there are certain situations where it’s not recommended.
Current or History of Breast Cancer
Having breast cancer now or in the past is a big reason to avoid HRT. The estrogen in HRT can make some breast cancers worse. So, women with breast cancer history should talk to their doctor before starting HRT.
History of Cardiovascular Disease
Heart disease is another reason to think twice about HRT. HRT, mainly estrogen, can raise the risk of heart problems. Doctors should be very careful when considering HRT for women with heart disease.
Unexplained Vaginal Bleeding
Unexplained vaginal bleeding is a warning sign against HRT. It could mean there’s a serious issue that needs to be checked. Starting HRT without finding out why you’re bleeding could hide a bigger problem, like cancer.
History of Venous Thromboembolism
Having had a blood clot in the veins or lungs is a big no for HRT. HRT, mainly estrogen, can make blood clots more likely. Women who’ve had blood clots should look into other options instead of HRT.
In short, HRT can help with menopause symptoms, but it’s not for everyone. Doctors need to check if HRT is safe for each patient. They must look at the patient’s health history and risks before starting HRT.
Relative Contraindications and Cautions for HRT
When thinking about Hormone Replacement Therapy (HRT), knowing the relative contraindications is key. These are conditions that need careful thought and watchful eye when deciding if HRT is right for someone.
Migraine Headaches with Aura
Migraine headaches, and those with aura, are a caution when it comes to HRT. Estrogen therapy might make migraines worse. It’s important to watch closely to see if HRT is safe to start or keep up.
Uncontrolled Hypertension
Uncontrolled high blood pressure is something to think about with HRT. Estrogen can affect blood pressure differently in everyone. It’s important to keep a close eye on blood pressure to manage risks.
| Condition | HRT Consideration | Monitoring Requirement |
|---|---|---|
| Migraine with Aura | Caution advised | Frequent headache monitoring |
| Uncontrolled Hypertension | Careful consideration | Regular blood pressure checks |
| Diabetes with Vascular Complications | Monitor closely | Regular vascular assessment |
Diabetes with Vascular Complications
For those with diabetes, HRT needs careful thought. The benefits must be weighed against the risks. It’s important to watch vascular health closely.
Gallbladder Disease
Gallbladder disease is also something to consider with HRT. Estrogen therapy might raise the risk of gallbladder problems. Patients with gallbladder issues should be watched closely for any worsening.
In summary, HRT has relative contraindications like migraine headaches with aura, uncontrolled hypertension, diabetes with vascular complications, and gallbladder disease. Creating personalized treatment plans that consider these factors is key for safe and effective HRT.
Monitoring and Adjusting Progesterone Therapy
Monitoring and adjusting progesterone therapy is key for the best results in hormone replacement. We must watch how patients react to treatment and tweak it as needed. This ensures the best outcomes.
Initial Assessment Timeline
Doctors usually check how well HRT is working after 4 to 6 weeks. This time lets us see how patients are doing and make changes if needed. Women over 50 should get regular breast checks and mammograms, with or without MHT.
Signs of Inadequate Dosing
Not enough progesterone can cause ongoing menopause symptoms like hot flashes and night sweats. We must watch for these signs and up the dosage if needed to help symptoms.
When and How to Increase Dosage
If symptoms don’t go away, we might need to up the progesterone dose. Deciding to do this depends on how the patient is doing and the doctor’s judgment. It’s important to weigh the benefits against the risks.
Managing Side Effects
Dealing with side effects is a big part of progesterone therapy. Common ones include feeling tired, dizzy, and tender breasts. We can lessen these by adjusting the dosage or how it’s given. For example, taking it at night can reduce daytime sleepiness.
By closely watching how patients respond and adjusting treatment as needed, we can make progesterone therapy work better. This way, we can get the most benefits while keeping risks low.
Special Considerations for Different Patient Populations
When it comes to HRT, each woman’s needs are unique. Hormone replacement therapy isn’t a one-size-fits-all solution. It’s important to consider a woman’s menopausal status, medical history, and health goals.
Perimenopausal Women
Women going through perimenopause may have irregular periods and changing hormone levels. HRT can help with symptoms like hot flashes and mood swings. We start with a low dose and adjust as needed.
Early Postmenopausal Women
Women in early menopause may benefit from HRT to ease symptoms and prevent osteoporosis. We focus on the timing and duration of HRT. Women with an intact uterus often get continuous combined therapy.
Women Over 60
For women over 60, starting HRT is a bigger decision. It depends on symptoms, osteoporosis risk, and heart health. We use a lower dose and watch for side effects, mainly for those with heart disease.
Women with Hysterectomy
Women who’ve had a hysterectomy don’t need progesterone. They often get estrogen-alone therapy. We stress the importance of watching for side effects and adjusting therapy as needed.
To show the different needs for these groups, let’s look at a table:
| Patient Population | HRT Considerations | Typical HRT Regimen |
|---|---|---|
| Perimenopausal Women | Symptom management, irregular periods | Low-dose, cyclic regimen |
| Early Postmenopausal Women | Symptom relief, osteoporosis prevention | Continuous combined therapy |
| Women Over 60 | Symptom management, cardiovascular health | Lower dose, careful monitoring |
| Women with Hysterectomy | Estrogen-alone therapy, simplified regimen | Estrogen-alone, adjusted as needed |
In conclusion, tailoring HRT to each woman’s needs is key. Understanding the unique needs of perimenopausal, early postmenopausal, women over 60, and those with hysterectomy helps us provide better care.
Discussing HRT Options with Healthcare Providers
Talking to your healthcare provider about HRT is a big step. It helps find the best treatment for you. A detailed conversation ensures you get care that fits your health history and needs.
Important Health History to Disclose
Before talking about HRT, gather all your health history. This includes any past medical issues, surgeries, allergies, and family health.
Make a list of your health history. Include:
- Any current or past medical conditions (like diabetes or high blood pressure)
- Surgeries or times you’ve been in the hospital
- Allergies to medicines
- Family history of diseases (like breast cancer or osteoporosis)
Questions to Ask About Progesterone Dosing
It’s important to understand progesterone dosing for HRT. Ask your healthcare provider about:
- The right dosage and how to take it (oral, vaginal, etc.)
- Possible side effects and how to handle them
- If the dosage might change based on how you react to treatment
Creating a Personalized Treatment Plan
A treatment plan made just for you is key to successful HRT. We work with your healthcare provider to make sure the treatment fits your needs perfectly.
What makes a treatment plan personal includes:
| Element | Description |
|---|---|
| Customized Dosage | The dosage of progesterone is tailored to your individual needs. |
| Monitoring Schedule | A schedule for regular check-ups to monitor your response to HRT. |
| Lifestyle Adjustments | Recommendations for diet, exercise, and other lifestyle changes to complement HRT. |
Follow-up Schedule Recommendations
Regular check-ups with your healthcare provider are key. They help adjust your treatment as needed. Schedule follow-ups as your healthcare provider suggests, usually:
- First follow-up: 4-6 weeks after starting HRT
- Future follow-ups: Every 3-6 months to check progress and adjust treatment
Conclusion: Balancing Benefits and Risks of HRT
Menopausal hormone therapy (MHT) is the best way to ease symptoms and improve life quality. We’ve talked about how HRT guidelines focus on weighing the good and bad sides.
Healthcare providers need to think about each patient’s needs and health history. Creating a treatment plan that fits each person and keeping an eye on how they’re doing is key. This way, we can reduce risks and increase benefits of HRT.
Knowing how progesterone works in HRT helps doctors make better choices. This knowledge lets them design treatments that really meet each patient’s needs.
The main aim of HRT is to make life better for women going through menopause. By carefully looking at the pros and cons, we can offer safe and effective treatments. This way, we can help our patients live better lives.
FAQ
What is Hormone Replacement Therapy (HRT) and how does it work?
Hormone Replacement Therapy (HRT) helps with menopause symptoms. It adds hormones that the body doesn’t make enough of. This usually means estrogen and progesterone to fight hot flashes and dryness.
What are the contraindications to Hormone Replacement Therapy?
You shouldn’t take HRT if you have breast cancer, heart disease, or bleeding issues. Also, if you’ve had blood clots or certain headaches, it’s not safe.
Why is progesterone important in HRT for women with an intact uterus?
Progesterone is key for women with a uterus. It balances estrogen’s effects on the uterus. This helps prevent problems like too much growth.
What is the lowest effective dose of progesterone for HRT?
The starting dose of progesterone is usually 100-200mg. But, the right dose can vary. It depends on each person’s needs.
How is progesterone administered in HRT?
Progesterone is often taken by mouth as micronized progesterone. The treatment can be daily or follow a cycle, based on what’s best for you.
What are the signs of inadequate progesterone dosing in HRT?
If you’re not getting enough progesterone, you might bleed too much or not feel better from menopause. These are signs you might need more.
How often should progesterone therapy be monitored?
Keep an eye on progesterone therapy closely. You’ll need a check-up in 4-6 weeks at the start. Then, watch for any side effects and adjust as needed.
Are there special considerations for different patient populations when using HRT?
Yes, HRT needs to be tailored for each group. This includes women in perimenopause, early postmenopause, over 60, or with a hysterectomy. It’s all about what’s best for you.
What health history should be disclosed when discussing HRT options with healthcare providers?
Share your health history fully. This includes any past or current conditions like breast cancer or heart disease. It helps make a treatment plan just for you.
How can a personalized treatment plan be created for HRT?
To get a treatment plan that fits you, talk to your doctor. Discuss your symptoms, health, and lifestyle. This way, you get the right HRT for you.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK493191/