Immunotherapy is a new hope for those with leukemia whose treatments don’t work well. It uses the body’s immune system to find and kill cancer cells. This makes it a powerful tool in the fight against leukemia.
Discoveries in immunotherapy are showing great promise. For example, immunotherapy for leukemia can be used alone or with other treatments. This depends on the type of leukemia and the patient’s health.
Explore the promise of immunotherapy in oncology. Find out if this advanced approach is becoming a definitive leukemia treatment and cure for patients.
Even though curing leukemia is a complex issue, immunotherapy is making a big difference. We will look at different types of immunotherapy and how they help in treating leukemia.
Key Takeaways
- Immunotherapy uses the immune system to fight leukemia.
- Types like CAR T cell therapy and monoclonal antibodies are showing great results.
- Studies have shown better remission and survival rates with immunotherapy.
- How well it works depends on the leukemia type and the patient’s health.
- Immunotherapy might have fewer side effects than traditional treatments.
The Landscape of Leukemia and Its Impact
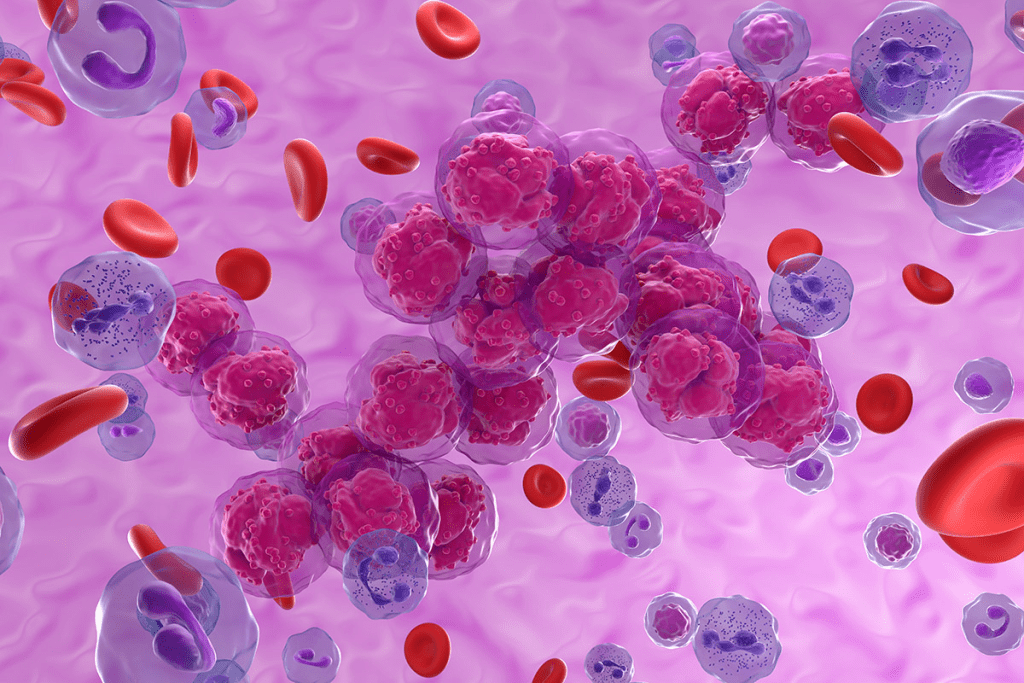
Leukemia is a complex disease that affects millions worldwide. It’s important to know its different forms and impacts. Leukemia is not just one disease but a group of disorders that affect the blood and bone marrow.
Leukemia cells often look normal, making them hard to fight. This is why it’s tough to diagnose and treat. To combat leukemia, doctors use Chimeric antigen receptor T-cell therapy (CAR T-cell therapy), Donor lymphocyte infusion, Monoclonal antibodies, and Immune checkpoint inhibitors.
Types of Leukemia and Their Prevalence
There are several types of leukemia, each with its own characteristics and level of commonality. The main types include:
- Acute Lymphoblastic Leukemia (ALL): A fast-progressing leukemia that affects the lymphoid cells.
- Acute Myeloid Leukemia (AML): A rapidly progressing leukemia that affects the myeloid cells.
- Chronic Lymphocytic Leukemia (CLL): A slow-progressing leukemia that affects the lymphoid cells.
- Chronic Myeloid Leukemia (CML): A slow-progressing leukemia that affects the myeloid cells.
Recent statistics show that the incidence of leukemia varies across different areas. Knowing these differences helps us develop better treatments.

Picture background
The Burden of Leukemia in the United States
In the United States, leukemia is a big health issue, with thousands of new cases every year. It affects not just the patients but also their families and caregivers. This puts a big strain on the healthcare system.
As we learn more about leukemia, it’s key to think about how it affects different people. We also need to consider the role of immunotherapy in treatment. By understanding leukemia’s types and impacts, we can see why we need more research and better treatments.
Traditional Leukemia Treatment Approaches
For decades, treating leukemia has mainly involved chemotherapy, radiation, and stem cell transplants. These methods have been key in fighting the disease. They offer different choices based on the patient’s diagnosis and health.
Chemotherapy Protocols
Chemotherapy is a mainstay in leukemia treatment. It uses drugs to kill cancer cells. The treatment plan varies based on the leukemia type, stage, and the patient’s health.
“Chemotherapy has been a cornerstone in treating leukemia for years,” said a leading oncologist. “But the treatment plan can vary a lot from one patient to another.”
Chemotherapy for leukemia often uses a mix of drugs in cycles. This helps treat the disease while protecting healthy cells. The goal is to reach remission, where the disease is no longer found.
Radiation Therapy Applications
Radiation therapy is also key in treating leukemia, mainly for certain types or before stem cell transplants. It uses high-energy rays to kill leukemia cells.
Picture background
Radiation therapy can target specific areas where leukemia cells may be. It’s often paired with chemotherapy to boost treatment results.
Stem Cell Transplantation
Stem cell transplantation, from a donor or the patient, can be a cure for some with leukemia. It replaces the patient’s sick bone marrow with healthy stem cells.
The success of stem cell transplantation depends on several factors. These include the patient’s age, health, and leukemia type. “Stem cell transplantation has changed leukemia treatment, giving hope to those with advanced disease,” said a hematologic malignancies specialist.
In summary, traditional treatments like chemotherapy, radiation, and stem cell transplants are vital in managing leukemia. Patients and doctors need to understand these options as they face the challenges of leukemia treatment.
Defining “Cure” in the Context of Leukemia
In leukemia, ‘cure’ means more than just getting better. It means being in complete remission, living a long time, and feeling well. Knowing these parts is key to judging treatment success and setting realistic hopes for patients.
Complete Remission vs. Functional Cure
Complete remission means no cancer cells are found in the body after treatment. Doctors check this with bone marrow biopsies and blood tests. But, a ‘functional cure’ is more than that. It means living a normal life without needing constant treatment.
“The goal of leukemia treatment is not just to achieve remission, but to ensure that patients can lead normal, healthy lives,” as emphasized by leading oncologists. Achieving a functional cure is very important. It lets patients stop treatment and live their lives freely.
Long-term Survival Metrics
Long-term survival is key to judging leukemia treatment success. We look at 5-year and 10-year survival rates. These rates show how many patients live for these times after being diagnosed.
For example, new treatments like immunotherapy have greatly improved survival rates. In Acute Lymphoblastic Leukemia (ALL), cure rates for relapsed patients have jumped from under 10% to up to 40% in some trials. This shows why we must look at long-term results when judging treatments.
Quality of Life Considerations
Quality of life is very important in leukemia treatment. Treatments can have big side effects that affect daily life. We focus on treatments that work well but don’t harm patients too much.
As we keep finding new treatments like immunotherapy, we must balance finding a ‘cure’ with keeping patients’ quality of life good. This way, we help leukemia patients not just survive but also thrive.
The Emergence of Immunotherapy as a Leukemia Treatment
Immunotherapy is a new hope for leukemia patients worldwide. It boosts the body’s defenses to fight leukemia cells better.
Principles of Cancer Immunotherapy
Cancer immunotherapy makes the immune system fight cancer cells. For leukemia, it helps the immune system find and kill cancer cells. This leads to better treatment results.
Immunotherapy is special because it specifically targets cancer cells. This reduces damage to healthy cells, unlike traditional treatments.
How Immunotherapy Targets Leukemia Cells
Immunotherapy fights leukemia cells in different ways. It boosts the immune system’s attack on these cells. This is done through various immunotherapies, such as:
- CAR T-cell therapy, which changes T-cells to attack leukemia cells.
- Monoclonal antibodies, which mark leukemia cells for the immune system to destroy.
- Immune checkpoint inhibitors, which let the immune system attack leukemia cells more freely.
Types of Immunotherapeutic Approaches
There are many ways to use immunotherapy for leukemia. Each approach is tailored to the patient’s needs. Some notable ones include:
- CAR T-cell therapy has shown great promise in treating some leukemias.
- Monoclonal antibody therapy targets specific leukemia cells.
- Cancer vaccines, which help the immune system fight leukemia cells.
A leading oncologist says, “Immunotherapy has changed how we treat leukemia. It offers a targeted and possibly less harmful option than traditional treatments.”
“The future of leukemia treatment is in improving immunotherapy. It has a lot of promise for better patient outcomes.”
, Oncologist
Understanding immunotherapy helps us see its promise in treating leukemia. It can greatly improve the lives of those with this disease.
CAR T-Cell Therapy: Revolutionizing Blood Cancer Treatment
CAR T-cell therapy is a major leap in fighting leukemia. It offers a more precise way to treat cancer. This method changes a patient’s T-cells to better target and destroy cancer cells.
Engineering T-Cells to Fight Leukemia
The therapy starts by taking T-cells from the patient’s blood. These T-cells are then changed to recognize and attack leukemia cells. After growing in number, they are given back to the patient to fight cancer.
This targeted approach helps CAR T-cells focus on cancer cells. This reduces harm to healthy cells and lowers side effects compared to old treatments.
FDA-Approved CAR T-Cell Therapies
Several CAR T-cell therapies have been approved by the FDA. tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta) are two. They work well for certain types of leukemia and lymphoma.
These approvals bring new hope to those who have tried other treatments without success.
Success Rates in Clinical Trials and Practice
Clinical trials show CAR T-cell therapy is effective. For example, tisagenlecleucel led to a complete remission in 81% of young patients with B-cell ALL.
Ongoing research aims to make CAR T-cell therapy even better. It’s looking at using it for more cancers and finding ways to lessen side effects.
Bispecific Antibodies: Bridging Immune Cells and Cancer
Bispecific antibodies are a new way to fight leukemia. They connect immune cells with leukemia cells, starting an immune attack. This method is showing great promise in treating different types of leukemia.
Mechanism of Action in Leukemia
Bispecific antibodies work by binding to two targets at once. One part targets leukemia cells, and the other part activates immune cells like T cells. This brings the immune cells close to the cancer, helping them attack it. The mechanism of action of bispecific antibodies in leukemia involves:
- Targeting specific antigens on leukemia cells
- Activating and engaging T cells or other immune effector cells
- Enhancing the immune response against leukemia cells
Approved Bispecific Antibody Treatments
Several bispecific antibodies have been approved for leukemia treatment. Blinatumomab is approved for relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL). It binds to CD19 on B cells and CD3 on T cells, helping T cells kill leukemia cells.
Efficacy Data and Patient Responses
Clinical trials show bispecific antibodies work well against leukemia. Patients on blinatumomab have seen big improvements, including complete remissions. This data shows bispecific antibodies can greatly help leukemia patients, even those with hard-to-treat disease.
We keep watching how bispecific antibodies are changing, with new research and targets. As the field grows, these antibodies will become more key in fighting leukemia.
Immunotherapy Outcomes in Acute Lymphoblastic Leukemia (ALL)
Immunotherapy has changed how we treat Acute Lymphoblastic Leukemia (ALL). It brings hope to patients all over the world. This new method has greatly improved results for both kids and adults with ALL.
Childhood ALL Treatment Success Stories
In kids, immunotherapy works really well. It has greatly increased leukemia remission rates. Studies show that targeted immunotherapies can lead to complete remission in many children with ALL.
For example, CAR T-cell therapy is a game-changer for childhood ALL. It has much better results than old treatments. This means many young patients now live longer and have a better quality of life.
Adult ALL Response to Immunotherapy
Adults with ALL also benefit from immunotherapy, but results can differ. Factors like age, genetic changes, and past treatments play a role. Yet, immunotherapy offers hope for lasting remissions in adults.
Research shows that bispecific antibodies and other immunotherapies are promising for adult ALL. They offer new ways to treat this tough group of patients.
Relapsed/Refractory ALL Management
For those with relapsed or refractory ALL, immunotherapy is key. Clinical trials show it can increase cure rates from less than 10% to up to 40% in some cases.
Managing relapsed/refractory ALL involves a mix of treatments. CAR T-cell therapy, bispecific antibodies, and other immunotherapies are used. They are often combined with other treatments to get the best results.
As research keeps improving, we’ll see even better treatments for ALL. Immunotherapy will play a bigger role in helping patients.
Acute Myeloid Leukemia (AML): Immunotherapy Challenges and Breakthroughs
Acute Myeloid Leukemia (AML) is a tough blood cancer to fight. But new hope comes from immunotherapy. AML causes abnormal white blood cells to grow fast, crowding out normal cells in the bone marrow.
The Unique Complexity of AML
AML is complex because it has many genetic mutations. This makes finding one treatment hard. Now, we know that each patient’s genes and molecules affect how aggressive the disease is and how well it responds to treatment.
Current Immunotherapeutic Approaches
Immunotherapy is a promising way to treat AML. The few methods are being used:
- CAR T-Cell Therapy: This method is mostly used for other leukemias but is being tested for AML, too.
- Checkpoint Inhibitors: These drugs help the immune system fight cancer cells better.
- Monoclonal Antibodies: These target specific cancer cells, marking them for destruction.
These treatments are being tested in clinical trials, alone or with traditional treatments like chemotherapy.
Survival Rates and Ongoing Clinical Trials
For AML, high-risk patients have a five-year survival rate of under 25%. But new immunotherapies might change this. Clinical trials are key to finding out if these treatments work and are safe. Research focuses on:
- Combining immunotherapy with other treatments to make them better.
- Creating new treatments that target specific AML types.
- Choosing the right patients for immunotherapy based on their genes and molecules.
As research keeps moving forward, we hope immunotherapy will help more with AML. This could lead to better survival rates and quality of life for patients.
Patient Factors Influencing Immunotherapy Success
Many factors can affect how well immunotherapy works for leukemia. Knowing these factors helps doctors tailor treatments for each patient. This makes treatments more effective.
Age and Comorbidity Considerations
Age is a big factor in how well immunotherapy works. Older patients might not respond as well because their immune systems are weaker. Also, health problems like heart disease or diabetes can make it hard for patients to handle immunotherapy.
When deciding if immunotherapy is right for a patient, age and health issues are key. For example, older patients or those with serious health problems might need their treatments adjusted or watched more closely.
Key considerations include:
- Checking the patient’s overall health for immunotherapy
- Changing treatment plans based on age and health
- Keeping a close eye on patients for side effects
Genetic and Molecular Profiles
The type of leukemia a patient has can greatly affect how well they do with immunotherapy. Some genetic changes or molecular profiles might mean a patient will respond better or worse to certain treatments.
For example, some genetic changes might make a patient more likely to benefit from certain immunotherapies. We’re learning more about how genetics affects how well immunotherapy works.
Important genetic factors include:
- Mutations in genes like FLT3 or NPM1
- Presence of specific surface antigens like CD19 or CD22
- Certain genetic changes that affect how well treatments work
Prior Treatment History
A patient’s past treatments can also change how well they do with immunotherapy. Patients who have had many treatments might not respond the same way as those who haven’t had any.
When choosing an immunotherapy, a patient’s past treatments are important. For example, patients who have had treatments before might need more aggressive or new approaches.
- Previous treatments like chemotherapy or targeted therapy
- How well patients responded to past treatments
- Any history of resistance or relapse
The Bone Marrow Microenvironment: A Key Battleground
The bone marrow microenvironment is a key area where leukemia cells meet the immune system. This complex system is vital for leukemia’s growth and spread.
How Leukemia Hijacks the Bone Marrow
Leukemia cells change the bone marrow to hide from the immune system and grow. They do this by messing with the normal bone marrow cells. This creates a space where they can live and multiply without being attacked.
Studies have found that leukemia cells can make the bone marrow less able to fight cancer. They do this by working with immune cells and the bone marrow stroma in complex ways.
Immunotherapy’s Role in Reprogramming the Microenvironment
Immunotherapy is a new way to fight leukemia by changing the bone marrow. It helps the immune system fight leukemia better, leading to better treatment results.
One effective method is CAR T-cell therapy. It makes T-cells attack leukemia cells. This helps the bone marrow to see and fight leukemia cells.
Measuring Minimal Residual Disease
Checking for minimal residual disease (MRD) is important in leukemia treatment. MRD are small leukemia cells left after treatment.
Tools like flow cytometry and molecular diagnostics find and count MRD. This helps doctors see if treatment is working and decide on more treatment.
Combination Strategies: The Future of Leukemia Treatment
Combination strategies are changing how we treat leukemia, giving patients new hope. By mixing different treatments, we can beat the limits of single treatments. This could lead to better results for patients.
Integrating Immunotherapy with Conventional Treatments
One exciting idea is to mix immunotherapy with old treatments like chemo and radiation. This combo can make traditional treatments work better. It uses the immune system to fight cancer cells.
Benefits of Combination Therapy:
- Enhanced treatment efficacy
- Potential to overcome resistance to single-modality treatments
- Improved patient outcomes
For example, studies show that adding CAR T-cell therapy to chemo can increase remission rates in some leukemia patients.
Multiple Immunotherapy Modalities
Another strategy is to use different immunotherapies together. This includes CAR T-cell therapy, bispecific antibodies, and checkpoint inhibitors. This approach attacks leukemia cells from many sides, aiming for lasting results.
“The future of leukemia treatment lies in combining different immunotherapies to create a more complete attack on cancer cells.” –
Leukemia Researcher
A clinical trial combining CAR T-cell therapy with a bispecific antibody showed good results in patients with relapsed/refractory leukemia.
Personalized Treatment Algorithms
Creating personalized treatment plans is key in the era of combination therapies. We analyze each patient’s unique traits, like their genes and treatment history. This helps us make the best combination of treatments for each person.
Key factors in personalizing treatment:
- Genetic and molecular profiling of the patient’s leukemia
- Previous treatment history and response
- Patient’s overall health and comorbidities
By tailoring treatments to each patient, we can make treatments more effective. This improves the lives of leukemia patients.
Conclusion: Is Immunotherapy a Cure for Leukemia?
Immunotherapy has changed how we treat leukemia, giving new hope to many patients. It’s not a cure for everyone, but it has made treatments better for some. This is a big step forward.
How well immunotherapy works depends on the type of leukemia and the patient. For example, CAR T-cell therapy has been a game-changer for some with acute lymphoblastic leukemia (ALL). It has helped some patients stay in remission for a long time. But it’s not a success for everyone, and we’re always looking to improve.
Immunotherapy is showing great promise, and we’re getting better at using it. By making treatments more personal and exploring new ways to combine them, we might find more cures. The journey to cure leukemia is complex, but the future looks brighter with each discovery.
FAQ
What is leukemia, and how does it affect the body?
Leukemia is a cancer that affects the blood and bone marrow. It causes the body to make too many abnormal white blood cells. This can lead to anemia, infections, and bleeding problems.
What are the different types of leukemia and their prevalence?
There are several types of leukemia, including Acute Lymphoblastic Leukemia (ALL), Acute Myeloid Leukemia (AML), Chronic Lymphocytic Leukemia (CLL), and Chronic Myeloid Leukemia (CML). ALL is more common in kids, while AML is more common in adults.
What is immunotherapy, and how does it target leukemia cells?
Immunotherapy uses the immune system to fight cancer. It targets leukemia cells by using CAR T-cell therapy and bispecific antibodies. These methods help recognize and destroy cancer cells.
What is CAR T-cell therapy, and how is it used in leukemia treatment?
CAR T-cell therapy is a form of immunotherapy. It makes T-cells attack leukemia cells. It’s shown great promise in treating blood cancers, including leukemia, with FDA-approved therapies.
What are bispecific antibodies, and how do they work in leukemia treatment?
Bispecific antibodies are a type of immunotherapy. They connect immune cells and cancer cells, helping destroy cancer cells. They’ve shown effectiveness in leukemia, mainly in clinical trials.
How does immunotherapy impact Acute Lymphoblastic Leukemia (ALL) treatment outcomes?
Immunotherapy has greatly improved ALL treatment, mainly in kids. It has also shown benefits for adult ALL. It has made managing relapsed or refractory ALL better.
What are the challenges and breakthroughs in using immunotherapy to treat Acute Myeloid Leukemia (AML)?
AML is a tough disease to treat with immunotherapy. But research and trials have made progress. They’ve helped understand AML better and find effective treatments.
What patient factors influence the success of immunotherapy in leukemia treatment?
Several factors can affect immunotherapy’s success. These include age, health conditions, genetic and molecular profiles, and past treatments.
What is the role of the bone marrow microenvironment in leukemia, and how does immunotherapy target it?
The bone marrow microenvironment is key in leukemia. Immunotherapy can change this environment to fight leukemia. It’s important to measure minimal residual disease to see how well treatment works.
What is the future of leukemia treatment, and how will combination strategies impact it?
The future of leukemia treatment involves combining different therapies. This includes using immunotherapy with traditional treatments or other immunotherapies. Personalized treatment plans will also be important in tailoring therapy to each patient.
Can leukemia be cured with immunotherapy, and what are the survival rates for different types of leukemia?
Immunotherapy has shown great promise in treating leukemia. Some types, like ALL, have high cure rates. Survival rates vary by leukemia type, with AML being a focus area.
What are the treatment options for leukemia, and how do they vary depending on the type and stage?
Leukemia treatments include chemotherapy, radiation, stem cell transplants, and immunotherapy. The choice depends on the leukemia type and stage, as well as the patient’s health.
What is the significance of leukemia medication and treatment for leukemia cancer?
Medications and treatments are vital in managing leukemia. They help improve patient outcomes. The right treatment depends on the leukemia type and stage.
References
- National Cancer Institute. (2023). Leukemia”Patient Version. Retrieved from https://www.cancer.gov/types/leukemia
- Maude, S. L., Laetsch, T. W., Buechner, J., Rives, S., Boyer, M., Bittencourt, H., … & Grupp, S. A. (2018). Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. New England Journal of Medicine, 378(5), 439-448. https://doi.org/10.1056/NEJMoa1709403