Last Updated on November 13, 2025 by
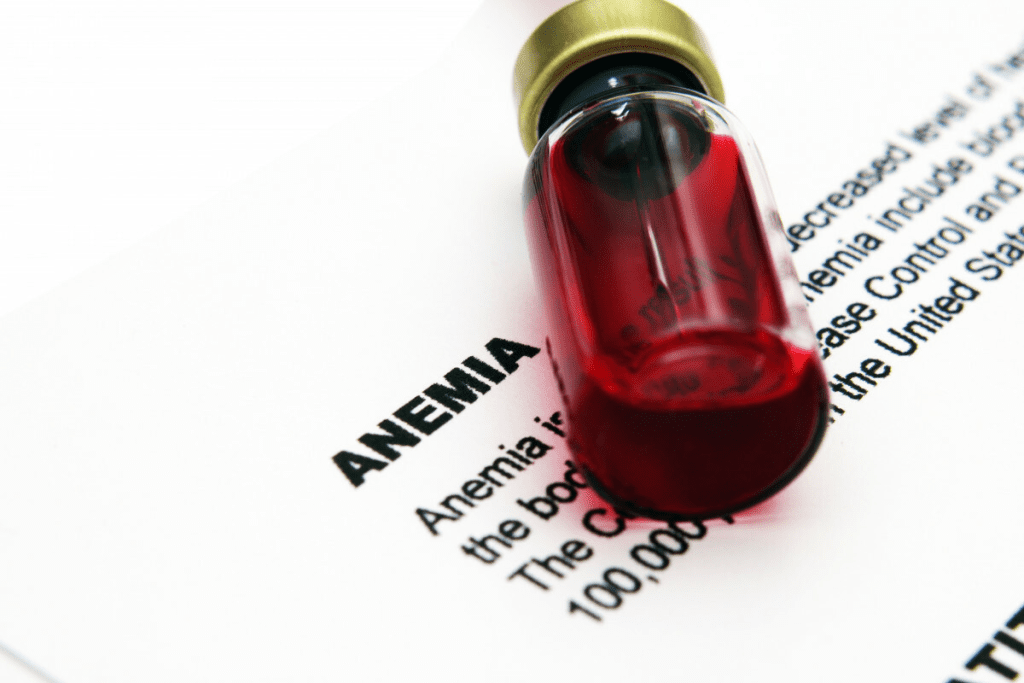
Chemotherapy-induced anemia (CIA) is a common problem for people getting cancer treatment. It happens when chemotherapy harms the bone marrow cells that make red blood cells. This leads to a low count of red blood cells. What is chemo-induced anemia called? Learn the link between anemia and cancer and the crucial term for this powerful side effect of treatment.
This results in patients feeling tired and having a lower quality of life. It’s important to know about CIA to help manage its effects on those getting chemotherapy.
Key Takeaways
- Chemotherapy-induced anemia (CIA) is a common side effect of cancer treatment.
- CIA occurs when chemotherapy damages bone marrow cells that produce red blood cells.
- The condition leads to a low red blood cell count, causing fatigue and decreased quality of life.
- Understanding the CIA is essential for managing its effects on chemotherapy patients.
- CIA affects more than half of the patients undergoing chemotherapy.
Understanding Chemotherapy-Induced Anemia (CIA)
Chemotherapy-induced anemia (CIA) is a big challenge in cancer care. It happens when chemotherapy lowers red blood cell production. This makes it hard for tissues and organs to get enough oxygen.
This side effect of chemotherapy really affects cancer patients’ lives. It makes their quality of life much worse.
Official Medical Terminology and Classification
CIA is graded based on how severe it is. The Common Terminology Criteria for Adverse Events (CTCAE) system is used. It ranges from mild (Grade 1) to very serious (Grade 4).
Getting the right diagnosis and grade is key to choosing the right treatment.
CIA is a big problem in cancer treatment. It leads to more fatigue, less energy, and a lower quality of life. It can also make cancer treatment less effective. This might mean having to reduce or delay chemotherapy doses.
Prevalence Rates Among Different Cancer Types
Up to 70% of people getting chemotherapy might get CIA. This is more common in lung, lymphoma, or reproductive system cancer patients. The chance of getting CIA depends on the cancer type, the chemotherapy, and the patient’s health.
For example, people with lung cancer or lymphoma are at higher risk. This is because their treatment is very intense. Knowing how common CIA is helps doctors prepare and manage it better.
By understanding CIA, we can improve care for cancer patients. We can use different treatments to help manage anemia. This includes medicines that help make more red blood cells and nutrition support.
The Relationship Between Anemia and Cancer
Anemia and cancer are linked in a complex way. Anemia happens when there aren’t enough red blood cells. This makes it hard for tissues and organs to get enough oxygen.
Cancer and its treatment can lead to anemia. We’ll look at how cancer itself can cause anemia. We’ll also see how chemotherapy affects red blood cell production.
Can Cancer Itself Cause Anemia?
Yes, cancer can cause anemia without treatment. Some cancers, like leukemias and lymphomas, affect the bone marrow. This disrupts blood cell production.
Cancer can cause anemia in several ways:
- It can fill the bone marrow with cancer cells, leaving less room for normal blood cells.
- It can make substances that slow down red blood cell production.
- It can cause long-term inflammation, leading to anemia of chronic disease.
Lung cancer can cause anemia through inflammation and bone marrow metastasis. Knowing if lung cancer can cause anemia is key to managing it well.

How Chemotherapy Damages Red Blood Cell Production
Chemotherapy is a big reason for anemia in cancer patients. It targets fast-growing cells, including cancer and bone marrow cells that make red blood cells.
Chemotherapy harms red blood cell production in a few ways:
- It directly weakens the bone marrow, making it hard to produce new red blood cells.
- It can lower the levels of erythropoietin, a hormone that helps make red blood cells.
So, patients on chemotherapy are at high risk of anemia due to chemotherapy. This is why there are specific ICD-10 codes for it.
It’s important to understand anemia in cancer patients. We’ll talk about how to diagnose and treat it next.
Common Signs of Low Hemoglobin in Cancer Patients
Chemotherapy can cause anemia, leading to many symptoms that affect patients’ lives. It’s important to know the physical and heart-related effects of low hemoglobin in cancer patients.
Physical Symptoms of Chemotherapy-Induced Anemia
Patients with chemotherapy-induced anemia often feel very tired. This is because their bodies don’t get enough oxygen. It makes it hard to do everyday things.
They might also feel short of breath or dizzy. Some notice their skin looks pale because of fewer red blood cells.
Some patients get headaches or feel cold in their hands and feet. This is because their bodies don’t get enough oxygen to these areas. It’s important for them to tell their doctors about these symptoms.
Low Blood Pressure and Other Cardiovascular Effects
Anemia from chemotherapy can also affect the heart. It can cause low blood pressure, leading to dizziness and fainting. This is because the body’s organs don’t get enough blood.
Also, the heart has to work harder without enough red blood cells. This can cause heart palpitations or a fast heartbeat. In severe cases, it can make heart problems worse or cause new ones.
“Anemia is a common complication in cancer patients, and its symptoms can significantly impact a patient’s quality of life. Managing anemia effectively is critical to improving patient outcomes.”
It’s key for both patients and doctors to understand these symptoms. Recognizing them early helps in managing anemia’s effects from chemotherapy.
Diagnosis and Monitoring of CIA
Diagnosing Chemotherapy-Induced Anemia depends on blood tests to check hemoglobin levels. Accurate diagnosis is key for managing CIA well and improving patient outcomes.
Blood Tests for Detecting Low Hemoglobin
Blood tests, like the Complete Blood Count (CBC), are the main way to diagnose anemia in cancer patients on chemo. The CBC looks at different parts of the blood, including hemoglobin levels. These levels are important for figuring out how severe the anemia is.
Regular blood tests help doctors keep an eye on hemoglobin levels. This lets them act quickly if there are any changes.
How Often Should Blood Counts Be Checked During Chemo?
The timing of blood count checks during chemo can change. It depends on the chemo plan, the patient’s health, and any signs of anemia.
Usually, blood counts are checked often, like weekly or before each chemo cycle. This helps see how chemo affects blood cell making.
- Patients with more severe anemia might need checks more often.
- Changes to chemo or starting treatments for anemia could be based on blood test results.
By watching blood counts closely, doctors can make smart choices about treatment. This helps manage CIA and supports the patient’s health.
Treatment Options for Chemotherapy-Induced Anemia
Managing chemotherapy-induced anemia (CIA) needs a mix of treatments. We’ll look at the different ways to tackle this condition. This will help improve patient outcomes and quality of life.
Erythropoiesis-Stimulating Agents (ESAs)
Erythropoiesis-stimulating agents (ESAs) are a key treatment for CIA. They help make more red blood cells, easing anemia. ESAs are very helpful for patients getting chemotherapy, as they cut down on blood transfusions.
Using ESAs has shown to be effective in treating CIA. It offers several benefits:
- Less need for blood transfusions
- Better hemoglobin levels
- Improved quality of life for patients
Blood Transfusions for Severe Anemia
In severe cases of anemia, blood transfusions are needed to quickly boost red blood cell count. Blood transfusions can quickly help patients with severe anemia symptoms.
Though blood transfusions work well in the short term, they’re mainly for severe cases. This is because of the risks and the need for matching blood types carefully.
Iron Supplementation Strategies
Iron supplementation is vital in managing CIA. Iron is key for making red blood cells, and supplements can help fix deficiencies.
There are many iron supplement strategies, like oral and intravenous iron. The choice depends on the patient’s condition, how severe the iron deficiency is, and other factors.
Dose Adjustments to Chemotherapy Regimens
In some cases, changing the chemotherapy regimen might help with anemia. This could mean adjusting the dose or schedule of chemotherapy drugs.
Adjusting doses is done on a case-by-case basis. It considers the patient’s health, how severe the anemia is, and the cancer being treated.
By knowing and using these treatment options, healthcare providers can manage CIA well. This improves patient outcomes and quality of life.
Improving Blood Cell Counts During Cancer Treatment
Improving blood cell counts is key in cancer treatment. Keeping blood cell counts healthy is vital for cancer patients. Low blood cell counts can cause anemia, infections, and bleeding disorders during treatment.
White Blood Cell Injections After Chemo
White blood cell injections, or G-CSF, boost white blood cell production after chemo. They help lower the risk of infections by speeding up white blood cell recovery. G-CSF injections are common in chemotherapy support.
Key benefits of white blood cell injections include:
- Reduced risk of infections
- Faster recovery of white blood cell counts
- Ability to continue chemotherapy as scheduled
Nutritional Approaches to Support Blood Cell Production
Nutrition is important for blood cell production during cancer treatment. A balanced diet with essential nutrients helps recover blood cell counts. Foods rich in iron, vitamin B12, and folate are best.
“A diet rich in fruits, vegetables, whole grains, and lean proteins can help support the body’s ability to produce healthy blood cells.”
Some good nutritional strategies are:
- Eat more iron-rich foods like red meat, spinach, and fortified cereals
- Choose foods high in vitamin B12, such as fish, poultry, and dairy
- Include folate-rich foods like leafy greens, legumes, and citrus fruits
Low PCV Treatment Strategies
Low packed cell volume (PCV) often means anemia in cancer patients. Treatment for low PCV includes:
- ESAs to boost red blood cell production
- Blood transfusions to quickly increase red blood cell counts
- Iron supplements for iron deficiency
Using these strategies can help manage blood cell counts during cancer treatment. This improves patients’ quality of life.
Conclusion
Understanding and managing chemotherapy-induced anemia (CIA) is key for better quality of life and treatment results for cancer patients. CIA is a big side effect of cancer treatment. It can cause fatigue, weakness, and even heart problems.
We talked about how to spot and track CIA with blood tests. There are treatments like erythropoiesis-stimulating agents, blood transfusions, and iron supplements. To manage CIA well, we need to tackle the root causes and support the patient’s health fully.
By focusing on treating chemo-induced anemia, doctors can lessen its effects on patients. This helps patients handle cancer treatment better. As we move forward in cancer care, we must keep an eye on patients’ overall health. This includes managing anemia and other cancer-related issues.
FAQ
What is chemotherapy-induced anemia (CIA)?
Chemotherapy-induced anemia (CIA) is when patients get low red blood cells or hemoglobin during chemo. It’s also called anemia of chronic disease or chemotherapy-induced anemia.
How common is anemia in cancer patients?
Anemia is very common in cancer patients, mainly those getting chemo. Many studies show a big number of cancer patients get anemia during treatment.
Can cancer itself cause anemia?
Yes, cancer can cause anemia. It can either invade the bone marrow or make substances that stop red blood cell production.
What are the symptoms of low hemoglobin in cancer patients?
Symptoms of low hemoglobin include tiredness, weakness, and shortness of breath. Dizziness and pale skin are also signs. Low blood pressure can happen too.
How is chemotherapy-induced anemia diagnosed?
Doctors use blood tests to find CIA. They check hemoglobin levels, red blood cell count, and other things. It’s important to get regular blood counts during chemo.
What are the treatment options for chemotherapy-induced anemia?
Treatments for CIA include ESAs, blood transfusions, iron supplements, and adjusting chemo doses. The right treatment depends on how bad the anemia is and what the patient needs.
How can the white blood cell count be improved during chemotherapy?
White blood cell injections, or G-CSF, can help after chemo. Eating a balanced diet rich in nutrients also helps make more blood cells.
What is the role of iron supplementation in managing CIA?
Iron supplements treat iron deficiency anemia, which can happen with CIA. They help refill iron stores and help make more red blood cells.
Can low PCV be treated?
Yes, low PCV can be treated. It depends on the cause and how bad it is. Treatments include iron supplements, ESAs, or blood transfusions.
How often should blood counts be checked during chemotherapy?
Blood counts need to be checked often during chemo. This is to catch anemia, neutropenia, and other blood problems early. How often depends on the chemo and the patient
References
U.S. National Library of Medicine. (2022). Chemotherapy-Induced Anemia: Pathophysiology and Management. Journal of the National Comprehensive Cancer Network, 20(4), 398-408. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9010001