Last Updated on October 21, 2025 by mcelik
Get a detailed comparison. We analyze whether the toxicity profile of immunotherapy matches or exceeds that of traditional cancer treatment and chemotherapy.
When we talk about fighting cancer, two big therapeutic approaches stand out: immunotherapy and chemotherapy. Both aim to eradicate cancer cells. But they work in different ways and have different side effects.

Immunotherapy boosts the immune system to find and destroy cancer cells. On the other hand, chemotherapy uses drugs to directly kill these cells. Knowing how these treatments affect people is key for both patients and doctors.
Our understanding of cancer is growing, leading to better treatments. Cancer care has moved from a one-size-fits-all method to more tailored options. This change is making treatments more effective and less harsh.
Older treatments like chemotherapy and radiation were common but had big side effects. Targeted therapies aim to hit cancer cells directly, sparing healthy tissues.
Thanks to new knowledge about cancer’s genetics, we can now pick treatments that work better. This means treatments that are more likely to help and less likely to harm.
Finding the right balance between fighting cancer and avoiding harm is tough. Immunotherapy is a new hope that uses the body’s immune system to fight cancer. But, it can also cause serious side effects, known as immune-related adverse events (irAEs).
Doctors must carefully choose treatments, considering both benefits and risks. This requires a deep understanding of how treatments work and their possible side effects.
By treating cancer in a personalized way, we can make treatments better and safer for patients.
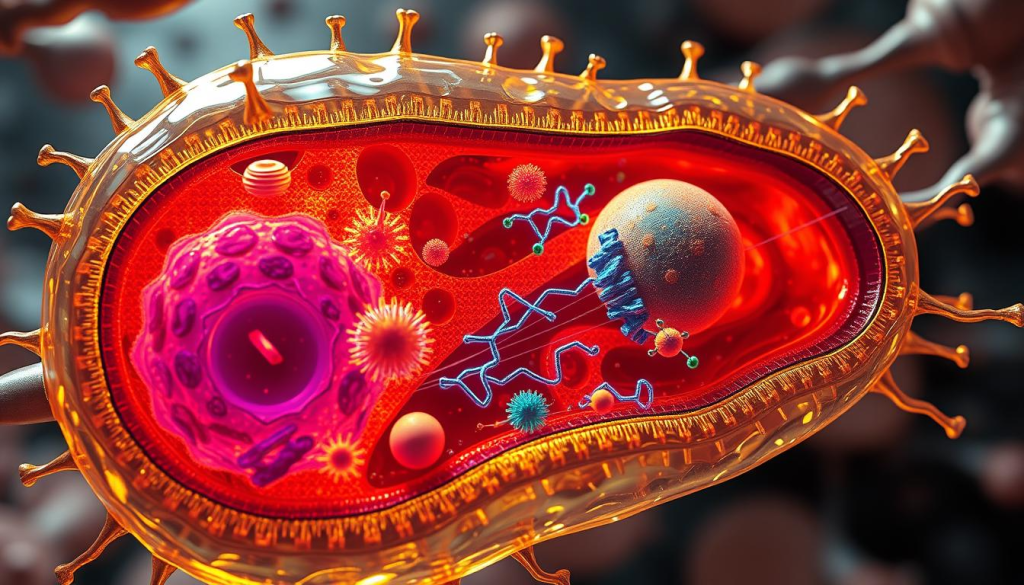
Chemotherapy is a key part of cancer treatment. It uses drugs to kill cancer cells. This treatment targets cells that grow fast, making it effective against many cancers.
Chemotherapy uses drugs that stop cancer cells from growing and dividing. These drugs can be taken by mouth or given through an IV. Once in the body, they travel through the blood to find and kill cancer cells.
This method is great for treating cancers that have spread or could spread to other parts of the body.
There are many types of chemotherapy drugs, each with its own way of fighting cancer. The main types include:
Chemotherapy is used to treat many cancers, often with other treatments like surgery and radiation. Some common cancers treated with chemotherapy include:
Understanding chemotherapy and its role in cancer treatment helps patients make informed decisions. Knowing what to expect and how it can treat their cancer can guide them through their treatment.
Immunotherapy is a new way to fight cancer by using the body’s immune system. It has changed how we treat cancer, offering a chance to cure many types of cancer.
Immunotherapy boosts the body’s defenses to fight cancer cells better. It’s different from old treatments that directly attack cancer. Instead, it makes the immune system stronger to find and destroy cancer cells.
The immune system fights off foreign substances and abnormal cells. But cancer cells can hide from it. Immunotherapy helps the immune system find and kill these hidden cancer cells.
There are many types of immunotherapy, each working in its own way to help the immune system fight cancer.
Immunotherapy has shown great promise in treating many cancers. Some patients have seen long-lasting benefits.
| Cancer Type | Immunotherapy Approach | Response Rate |
| Melanoma | Checkpoint Inhibitors | High |
| Non-Small Cell Lung Cancer (NSCLC) | Checkpoint Inhibitors | Moderate to High |
| Renal Cell Carcinoma | Checkpoint Inhibitors, Cytokines | Moderate |
| Bladder Cancer | Checkpoint Inhibitors | Moderate |
The table shows some cancers respond well to immunotherapy. This gives hope to patients with these cancers.
Chemotherapy is a key part of cancer treatment but has a big side effect list. It’s important to know how it affects patients’ lives and how to lessen these effects.
Chemotherapy can cause many side effects, some right away and others later. Common ones include hair loss, nausea, and fatigue. Studies show many patients get these, with effects ranging from mild to severe.
A study in Nature shows how common these side effects are and how they affect patients.

These side effects highlight the need for care that covers all aspects of a patient’s health. Knowing what are chemo and its side effects is key for doctors and patients alike.
Chemotherapy can also cause long-term and delayed side effects. These might include heart problems, new cancers, and brain issues. The risk depends on the type of chemo, dose, and how long it’s used.
It’s vital to watch for these effects, especially as more people survive cancer.
Chemotherapy’s side effects can really hurt a patient’s life during treatment. They can cause physical pain and fatigue, as well as emotional issues like anxiety and depression. Knowing the differences between chemo vs radiation can help choose the best treatment.
Healthcare teams can make treatment better by understanding and reducing side effects. This includes supportive care and teaching patients how to handle side effects. This way, they can improve life during and after chemo.
Immunotherapy is a new way to fight cancer, but it has risks. These risks are mainly immune-related adverse events (irAEs). It’s important for patients and doctors to know about these side effects.
Immunotherapy boosts the body’s fight against cancer cells. But, this strong immune action can sometimes harm healthy tissues and organs. This leads to irAEs. The type of immunotherapy used affects how common and severe these side effects are.
irAEs can affect many parts of the body. Symptoms include skin issues like rashes and itching, and stomach problems like diarrhea. They can also cause thyroid and adrenal gland problems. Knowing about these side effects helps manage them better.
To treat irAEs, doctors often use corticosteroids or other drugs to calm the immune system. Sometimes, stopping immunotherapy is needed.
Immunotherapy can also cause severe inflammation in organs. This can lead to lung, liver, or colon inflammation, which can be dangerous. It’s important to catch and treat these problems quickly.
Severe irAEs need fast medical help. Treatment usually includes strong corticosteroids and care to manage symptoms and prevent lasting damage.
The number of side effects from immunotherapy varies. Some people have mild side effects that are easy to handle. Others may face more serious reactions.
Even though severe irAEs are rare, it’s key for patients to know the risks. They should tell their doctors about any symptoms right away. By understanding and managing these side effects, we can make immunotherapy safer and more effective.
Choosing between immunotherapy and chemotherapy depends on several factors, including side effects. It’s important for patients and doctors to know these differences to make the best choice.
Immunotherapy and chemotherapy have different side effects. Chemotherapy can cause severe issues like hair loss, nausea, and tiredness right away. Immunotherapy, on the other hand, can lead to immune-related problems that are serious but less expected.
Chemotherapy’s side effects are often more immediate and can be dose-limiting, whereas immunotherapy’s irAEs can occur at any time during treatment and sometimes after.
The timing and length of side effects vary between treatments. Chemotherapy side effects usually start during or right after treatment and may go away once treatment ends. Immunotherapy side effects can show up weeks or months after starting.
Managing side effects well means knowing what to expect. Chemotherapy side effects are usually more predictable and can be handled with known methods. Immunotherapy’s side effects, though serious, can also be managed with careful monitoring and treatment.
Early detection and treatment of irAEs are critical to preventing severe outcomes.
How easily side effects can be reversed varies between treatments. Many chemotherapy side effects can be reversed, but some may last. Immunotherapy’s side effects can sometimes be treated with steroids or other treatments, but they can also have long-term effects if not managed right.
Understanding how side effects of immunotherapy relate to its effectiveness is key. This knowledge helps both patients and healthcare providers. The link between immunotherapy’s side effects and its success is complex and multifaceted.
Research shows that side effects, especially immune-related adverse events (irAEs), can mean a good response to treatment. This has been seen in many studies. It suggests that patients with certain side effects might have a better chance of recovery.
A study in a top medical journal found a link. Patients with advanced melanoma who had irAEs while on immunotherapy lived longer. This shows that side effects could be a sign of treatment working well.
Moderate irAEs are linked to better survival in several cancers. These side effects show the immune system is fighting the treatment, making it more effective against tumors.
Severe side effects are more complex. They can greatly affect a patient’s life quality and might stop treatment.
But, some studies show severe irAEs can still mean better survival, if managed right. The goal is to balance treatment benefits with the risks of side effects.
Knowing how side effects and effectiveness are linked is crucial. It helps doctors:
As we learn more about immunotherapy, understanding its side effects and success is key. This knowledge helps us improve cancer treatment for better patient results.
Cancer treatment is changing, with new therapies combining immunotherapy and chemotherapy. These combined methods show great promise. It’s key to understand why they’re used, their benefits, and the challenges they face.
Using both immunotherapy and chemotherapy together makes sense. Chemotherapy helps immunotherapy work better by releasing more tumor antigens. This makes the tumor environment better for treatment, as shown in PMC5514969.
This approach is moving towards more tailored and effective treatments. It’s a step towards better cancer care, combining different methods to fight cancer.
Studies show that combining these therapies can greatly improve survival in non-small cell lung cancer (NSCLC) and other cancers. For example, adding immunotherapy to chemotherapy has led to better survival and less cancer growth in advanced NSCLC.
This benefit isn’t just for NSCLC. Bladder cancer and some breast cancers also show good responses to this combined treatment.
One big challenge is dealing with the side effects of both treatments together. Both can cause different problems, and together, these can get worse. This can lead to more health issues.
To tackle this, we need to closely watch patients on these treatments. We must also have plans ready to handle any bad side effects early on. This includes spotting and treating immune-related side effects quickly.
Not every patient is right for these combined treatments. Choosing the right patients is crucial. We look at the tumor, the patient’s health, and biomarkers to predict how well they’ll do.
By picking the right patients and tailoring treatments, we can make the most of these therapies. This way, we can enjoy the benefits while reducing the risks.
| Cancer Type | Treatment Approach | Outcome |
| NSCLC | Immunotherapy + Chemotherapy | Improved Survival Rates |
| Bladder Cancer | Immunotherapy + Chemotherapy | Enhanced Response Rates |
| Breast Cancer | Immunotherapy + Chemotherapy | Better Clinical Outcomes |
Managing cancer treatment’s side effects is crucial. Today’s treatments are getting better, but we can’t treat everyone the same way. Each person’s body reacts differently to treatment.
Every patient’s response to treatment is unique. This depends on their genes, health, and lifestyle. Patient-specific risk assessment helps predict how well they’ll do.
Doctors can adjust treatments based on a patient’s risk. This can help avoid serious side effects. It’s a step towards better managing treatment’s effects.
After assessing a patient’s risk, proactive monitoring strategies kick in. This includes regular check-ups and advanced tests. It also involves listening to what patients say about their health.
For example, patients on immunotherapy need close watch for immune problems. Early detection helps doctors act fast, improving results.
Supportive care is key in handling treatment side effects. It includes medicines, nutrition advice, and mental health support.
Patients on chemo might get meds for nausea. Those on immunotherapy might learn how to save energy. Customizing care for each patient boosts their quality of life.
Good communication is vital in managing side effects. Patients need to know what side effects might happen and how they’ll be handled.
“Clear communication about expected side effects empowers patients to take an active role in their care, improving adherence to treatment and overall satisfaction with their care experience.” – An Oncologist
Open talks help doctors address concerns and adjust plans. This leads to better care for patients.
It’s key for patients and doctors to know how cancer treatments work. We’ve looked at the differences between immunotherapy and chemotherapy. This helps us see the good and bad sides of each.
Choosing between immunotherapy and chemotherapy depends on many things. This includes the cancer type, the patient’s health, and what the treatment aims to do. Immunotherapy might have fewer side effects for some cancers. But, both treatments have their own risks and benefits.
Patients and doctors can work together to find the best treatment plan. This plan should aim for the best results while keeping side effects low. This way, people can make smart choices about their care. It helps improve how well treatments work and how good a person feels.
Chemotherapy is a treatment for cancer that uses drugs. It kills cancer cells by targeting cells that grow fast. This method can treat many types of cancer.
Immunotherapy uses the body’s immune system to fight cancer. It’s different from chemotherapy because it doesn’t directly attack cancer cells. Instead, it helps the immune system find and destroy them.
Immunotherapy might be able to cure some stage 4 cancers. But, how well it works depends on the cancer type and the patient’s health.
Chemotherapy can cause side effects like nausea, tiredness, hair loss, and a higher risk of infections. The severity and how long these side effects last vary.
Immunotherapy can lead to side effects like inflammation, skin issues, and problems with hormones. How severe these side effects are can vary.
The side effects of immunotherapy and chemotherapy are different. Understanding these differences helps patients and doctors make better treatment choices.
Yes, combining these treatments can improve survival rates in some cancers. But, managing the side effects together can be tough. Choosing the right patients for this combination is key.
Personalized care is crucial for managing treatment side effects. This includes assessing risks, monitoring, supportive care, and talking with doctors. Patients should work closely with their healthcare team to create a personalized plan.
Sometimes, the side effects of immunotherapy can mean the treatment is working. This understanding helps patients and doctors see the potential benefits and risks of immunotherapy.
Radiation therapy and chemotherapy are both treatments for cancer. But, they work in different ways. Radiation uses rays to kill cancer cells, while chemotherapy uses drugs. The choice between them depends on the cancer type and stage.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!