Last Updated on October 21, 2025 by mcelik
If it’s not the right option, what’s next? We list and explain the effective alternative treatments to immunotherapy for various types of cancer.
Immunotherapy has changed how we fight cancer today. But, other treatments are also key, working well for different patients.
There are many ways to treat cancer, like surgery, chemotherapy, and radiation therapy. These methods have shown great success, helping many people live longer and healthier lives.
We are dedicated to top-notch healthcare for patients from around the world. We explain how these treatments can help fight cancer in different ways.
Immunotherapy is becoming key in cancer treatment. It uses the immune system to fight cancer. This approach is very promising.
Immunotherapy boosts or suppresses the immune system to fight cancer better. There are different types of immunotherapy. These include monoclonal antibody therapy, checkpoint inhibitors, and adoptive T-cell therapy.
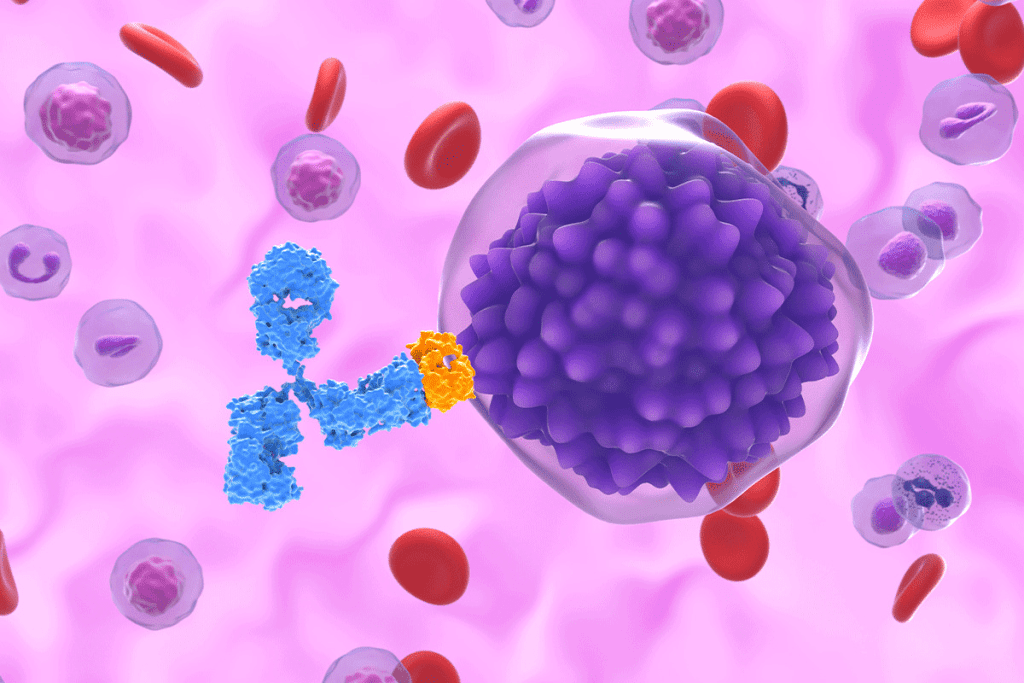
Monoclonal antibody therapy targets specific cancer cells with antibodies. Checkpoint inhibitors help the immune system attack cancer cells more. Adoptive T-cell therapy modifies T-cells to recognize cancer cells and then reinfuses them.
Immunotherapy has its limitations and challenges. It doesn’t work for everyone. The success of immunotherapy depends on the cancer type and the patient’s immune response.
Another issue is severe side effects. Immunotherapy can sometimes attack healthy tissues. Finding ways to manage these side effects and predict who will benefit is ongoing research.
We are working hard to understand and improve immunotherapy in cancer treatment. We aim to overcome its challenges and make it more effective.
Surgery is a key part of cancer treatment, a good choice instead of immunotherapy for many. It’s a proven method for treating cancers like breast, prostate, and colorectal.
Surgery for cancer can differ based on the disease type and stage. The main goal is to take out the tumor and any nearby tissue. There are several types of surgeries:
Surgery works well for early-stage cancers. Early detection means the tumor can often be removed, leading to high cure rates. For example, early-stage breast cancer treated with surgery alone or with other treatments has a 5-year survival rate over 90%.
Several factors contribute to surgery’s success in early-stage cancers:
Surgery is often the first choice over immunotherapy in some cases. For instance, if the cancer is localized and can be removed surgically, surgery is usually the first treatment. Surgery is also preferred when the cancer type doesn’t respond well to immunotherapy.
When deciding between surgery and immunotherapy, we consider several factors:
Healthcare providers carefully weigh these factors to choose the best treatment plan. This might include surgery, immunotherapy, or a mix of both.
Chemotherapy is a key treatment for cancer. It targets cancer cells throughout the body. It’s used for many types of cancer and helps lower death rates.
Chemotherapy kills or stops cancer cells from growing. This treatment is vital for cancers that have spread.
Chemotherapy drugs fall into different groups based on how they work. These include:
Knowing about these drug types helps doctors choose the best treatment for each patient.
Today’s chemotherapy plans are more advanced. They use new drugs and combinations to improve results. These plans are made just for each patient, based on their cancer type, stage, and health.
Some modern methods include:
Chemotherapy has a big impact on cancer death rates. It helps control cancer growth and spread.
“Chemotherapy has been a cornerstone in the treatment of various cancers, significantly improving survival rates and quality of life for patients.”
” Oncology Expert
Understanding chemotherapy’s role in cancer treatment helps patients and doctors make better choices.
Radiation therapy is used in about 50% of cancer cases. It kills cancer cells and shrinks tumors. This method can cure or lead to long-term remission in over 40% of cases for localized cancers.

External beam radiation therapy (EBRT) uses radiation from outside the body. EBRT is highly versatile and can be tailored to the specific needs of the patient. It delivers precise doses of radiation to the tumor site while protecting healthy tissues.
The technology behind EBRT has improved a lot. Modern linear accelerators allow for precise radiation delivery. Techniques like IMRT and SBRT have made EBRT even more effective, enabling higher doses to be given with greater accuracy.
Brachytherapy places a radioactive source inside or near the tumor. This method delivers high doses of radiation directly to cancer cells, reducing harm to healthy tissues. It can be temporary or permanent, depending on the cancer type and treatment plan.
Brachytherapy works well for cancers like prostate and cervical. It delivers radiation directly to the tumor, which can reduce side effects and improve treatment results.
The results of radiation therapy depend on the cancer type, stage, and patient’s health. For many patients, radiation therapy can significantly shrink tumors and improve survival rates. In some cases, it can even be curative, mainly for localized cancers.
Radiation therapy is often combined with surgery and chemotherapy. The choice of radiation therapy depends on the cancer type, stage, and patient’s health status.
Targeted therapies have changed cancer treatment, making it more effective. These treatments focus on specific changes in cancer cells. They are designed to be more precise, reducing harm to healthy cells and side effects.
Tyrosine kinase inhibitors (TKIs) block enzymes that help cancer cells grow. They are used for cancers like chronic myeloid leukemia (CML) and non-small cell lung cancer (NSCLC). TKIs have significantly improved outcomes for patients with certain genetic mutations.
Monoclonal antibodies are a game-changer in cancer treatment. They are made to target specific antigens on cancer cells. Monoclonal antibodies can also carry drugs or radiation to cancer cells, making treatment more effective and reducing side effects.
PARP inhibitors are a new type of targeted therapy. They work well for cancers with specific genetic weaknesses, like BRCA1 and BRCA2 mutations in breast and ovarian cancers. By stopping the PARP enzyme, these drugs prevent cancer cells from repairing DNA damage, causing them to die. Other targeted therapies target angiogenesis and specific molecular changes in cancer cells.
In summary, targeted therapies are a big step forward in cancer treatment. They offer precision medicine that improves patient outcomes. By understanding a patient’s cancer, we can tailor treatments to be more effective and safer.
Hormone-sensitive cancers, like some breast and prostate cancers, can be treated with hormonal therapies. These treatments either lower hormone levels or block hormone effects on cancer cells. This makes hormonal therapies key in fighting hormone receptor-positive cancers.
“Hormonal therapy is a cornerstone in managing hormone-sensitive cancers,”, a leading oncologist. “It offers patients a treatment option that can greatly improve their quality of life and survival rates.” This shows how important it is to tailor treatments to each patient’s cancer.
In breast cancer, hormonal therapies work best for tumors that are estrogen or progesterone receptor-positive. Treatments include:
These therapies have been shown to reduce recurrence risk and improve survival in hormone receptor-positive breast cancer patients.
For prostate cancer, hormonal therapies aim to lower male hormones (androgens) like testosterone. These hormones can fuel prostate cancer growth. Common treatments include:
These treatments can control prostate cancer progression and ease symptoms of advanced disease.
While immunotherapy has changed cancer treatment by using the body’s immune system, hormonal therapies offer unique survival benefits for hormone-sensitive cancers. For example, in ER-positive breast cancer, hormonal therapies significantly lower mortality rates. In prostate cancer, ADT improves survival and quality of life.
A study in the Journal of Clinical Oncology found that patients with hormone receptor-positive breast cancer treated with hormonal therapies had a lower risk of recurrence. Immunotherapy, while effective in some cases, may not offer the same benefits for these cancers.
In conclusion, hormonal therapies are a vital treatment for hormone-sensitive cancers, providing significant survival and quality of life benefits. As cancer treatment evolves, understanding the role of hormonal therapies and their comparison to treatments like immunotherapy is key for improving patient care.
Choosing alternatives to immunotherapy depends on several factors. These include the type of cancer, the patient’s health, and the cost. It’s important to know when alternatives might be better than immunotherapy.
Not all cancers react the same to treatments. Some cancers might not respond well to immunotherapy. In these cases, other treatments could be more effective.
Each patient’s situation is unique. Factors like age, health, and past treatments are important. They help decide the best treatment.
Cost and where to get treatment also matter. Immunotherapy is effective but can be expensive. It might not be available to everyone.
Healthcare providers can make better choices by considering these factors. This ensures patients get the best care for their needs.
In the fight against cancer, combination treatment approaches have become a key strategy. They combine several therapies to target cancer cells more effectively. This improves patient outcomes.
Combination treatments use different therapies to attack cancer cells in various ways. This approach helps overcome the weaknesses of single treatments.
Surgery is a mainstay in cancer treatment. When paired with adjuvant therapy, it boosts patient results. Adjuvant therapy, like chemotherapy or radiation, is used after surgery to kill any leftover cancer cells.
In breast cancer, surgery is followed by chemotherapy or radiation to lower recurrence risk. This combo has shown to increase survival rates in many cancers.
Chemoradiation combines chemotherapy and radiation therapy. It’s used for cancers that are hard to remove or need aggressive treatment.
Chemoradiation makes cancer cells more sensitive to radiation. This increases the chance of controlling tumors. For example, it’s a standard treatment for some head and neck cancers.
Multimodal treatment planning mixes different treatments like surgery, chemotherapy, and radiation. It creates a custom plan for each patient.
This method considers each patient’s cancer type and stage. By combining therapies, we aim for better results and lower recurrence risk.
In summary, combining treatments is a big step forward in cancer care. It uses the strengths of various therapies to offer better options for patients.
New treatments are changing how we fight cancer. These new methods are not just about immunotherapy. They show great promise in the fight against cancer.
Gene therapy fixes genes in cells. It aims to fix genes that lead to cancer. Advances in CRISPR technology make this possible.
Gene therapy can treat cancers caused by certain genes. It fixes or replaces bad genes, stopping cancer cells from growing.
Photodynamic therapy uses light to kill cancer cells. A special compound reacts to light, creating oxygen that kills cancer. It’s great for treating surface tumors.
This therapy is good because it only targets cancer cells. It’s also gentle on healthy tissue. It’s a good option for those who can’t have surgery.
Oncolytic virus therapy uses viruses to kill cancer cells. These viruses can also carry genes to boost the immune system or kill cancer cells directly.
This therapy is promising because it targets cancer cells without harming normal cells. It’s being tested in many cancers and shows promise.
These new treatments offer hope for cancer patients. Gene therapy, photodynamic therapy, and oncolytic virus therapy are changing cancer treatment. They show the future of fighting cancer is bright.
The future of cancer treatment is all about personalization. Therapies are picked based on each patient’s unique cancer. This new way of treating cancer is more effective and meets each person’s needs.
Biomarkers and genetic testing are key in choosing personalized cancer treatments. They help find specific genetic changes or biomarkers in a patient’s cancer. This lets us pick the best treatment plan.
Genetic testing looks at a patient’s DNA for mutations that might be causing their cancer. Knowing this helps us tailor treatments to fit the tumor’s genetic makeup. This approach can lead to better results and fewer side effects.
Each patient’s health, medical history, and what they prefer are also important. We look at these when deciding on treatments. This makes sure the chosen therapy is not just effective but also right for the patient.
For example, someone with heart disease might need a different treatment than someone without. Also, what the patient wants in terms of treatment, side effects, and quality of life matters a lot.
The shared decision-making process is a team effort. It involves patients, their families, and doctors working together. This way, everyone is informed and involved in making treatment choices.
By using biomarkers, genetic testing, and considering each patient’s unique situation, we can offer treatments that work well. These treatments also match what the patient wants and needs.
There are many ways to treat cancer, not just immunotherapy. Options include surgery, chemotherapy, and radiation therapy. Targeted and hormonal therapies are also available.
The right treatment depends on the cancer type and the patient’s needs. It also considers economic and accessibility factors.
At our institution, we focus on top-notch healthcare for international patients. We understand that each patient is different. So, we tailor cancer treatment plans to fit their needs.
We look at each patient’s unique situation and cancer type to choose the best treatment. This might be immunotherapy or another approach. Our aim is to give our patients the best care possible.
We use a team effort and the latest cancer treatment methods. This way, we ensure our patients get the best results.
In summary, while immunotherapy is a big step forward in cancer treatment, it’s not the only choice. We need to look at all treatment options to get the best results for our patients.
Immunotherapy for cancer uses the body’s immune system to fight cancer. It helps the immune system find and attack cancer cells.
Alternatives include surgery, chemotherapy, and radiation therapy. There are also targeted therapies and hormonal therapies. These can be used alone or together to treat cancer.
Surgery is often chosen for early-stage cancers. It’s used when the cancer is in one place and can be removed. It also helps when symptoms like obstruction or bleeding need to be relieved.
Chemotherapy uses drugs to kill cancer cells. It’s used for cancers that have spread to many parts of the body.
Radiation therapy kills cancer cells with high-energy rays. It can be given from outside the body (external beam radiation) or inside (brachytherapy).
Targeted therapies focus on specific molecules in cancer cells. Examples include tyrosine kinase inhibitors and monoclonal antibodies. They aim to stop cancer growth.
Hormonal therapies block hormones that help cancer grow. This is used in cancers like breast and prostate cancer.
Using treatments together can improve results. This includes surgery with other therapies. It attacks cancer from different angles.
New treatments include gene therapy and photodynamic therapy. They are being studied to treat different cancers.
Treatment choices are based on biomarkers and genetic tests. They consider patient-specific factors and involve the patient and healthcare team.
Immunotherapy boosts the immune system to fight cancer. Chemotherapy uses drugs to kill cancer cells directly.
Yes, alternatives include immunotherapy, targeted therapies, and hormonal therapies. These options are available instead of chemotherapy.
Immunotherapy uses the immune system to fight cancer and other diseases. It’s a treatment approach.
Examples include checkpoint inhibitors and cancer vaccines. Adoptive T-cell therapy is also an example.
Types include monoclonal antibodies and checkpoint inhibitors. Cancer vaccines are also part of immunotherapy.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!