Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 30% of patients see their brain tumors come back within a year after surgery. This shows why we need to understand what makes regrowth happen.
We dive into the details of post-surgery tumor recurrence. This includes the type of tumor, how surgery is done, and care after surgery. Our goal is to shed light on the brain tumor recurrence rate. This way, patients and doctors can make better choices.
Key Takeaways
- The rate of brain tumor regrowth changes a lot based on the tumor type and surgery methods.
- Knowing about post-operative care is key to lowering the chance of recurrence.
- It’s important to keep up with regular check-ups to spot tumor recurrence early.
- The speed of post-surgery brain tumor growth can be affected by many things, like how much of the tumor was removed.
- New surgical methods are helping improve results for patients.
Understanding Brain Tumors and Their Growth Patterns
Brain tumors are complex and varied. It’s important to understand their growth patterns for effective treatment. Knowing the different types and their characteristics helps predict recurrence and create personalized treatment plans.
Types of Primary and Secondary Brain Tumors
Brain tumors are divided into primary and secondary types. Primary tumors start in the brain, while secondary tumors spread from other parts of the body. The most common primary brain tumors are gliomas, meningiomas, and astrocytomas.
Gliomas come from the brain’s glial cells and are graded by aggressiveness. Meningiomas are usually benign and grow in the meninges, the brain and spinal cord’s protective membranes. Astrocytomas are a type of glioma that starts from astrocytes, a specific glial cell.
Natural Growth Characteristics of Different Tumor Types
The growth of brain tumors varies by type. For example, low-grade gliomas grow slowly, while high-grade gliomas grow quickly. Meningiomas are slow-growing but can be malignant in some cases.
Tumor Type | Growth Rate | Malignancy |
Low-Grade Glioma | Slow | Low |
High-Grade Glioma | Rapid | High |
Meningioma | Slow | Usually Benign |
Knowing how tumors grow is key to predicting recurrence and planning treatment. By analyzing a tumor’s type and characteristics, doctors can give better prognoses and tailor treatments to each patient’s needs.
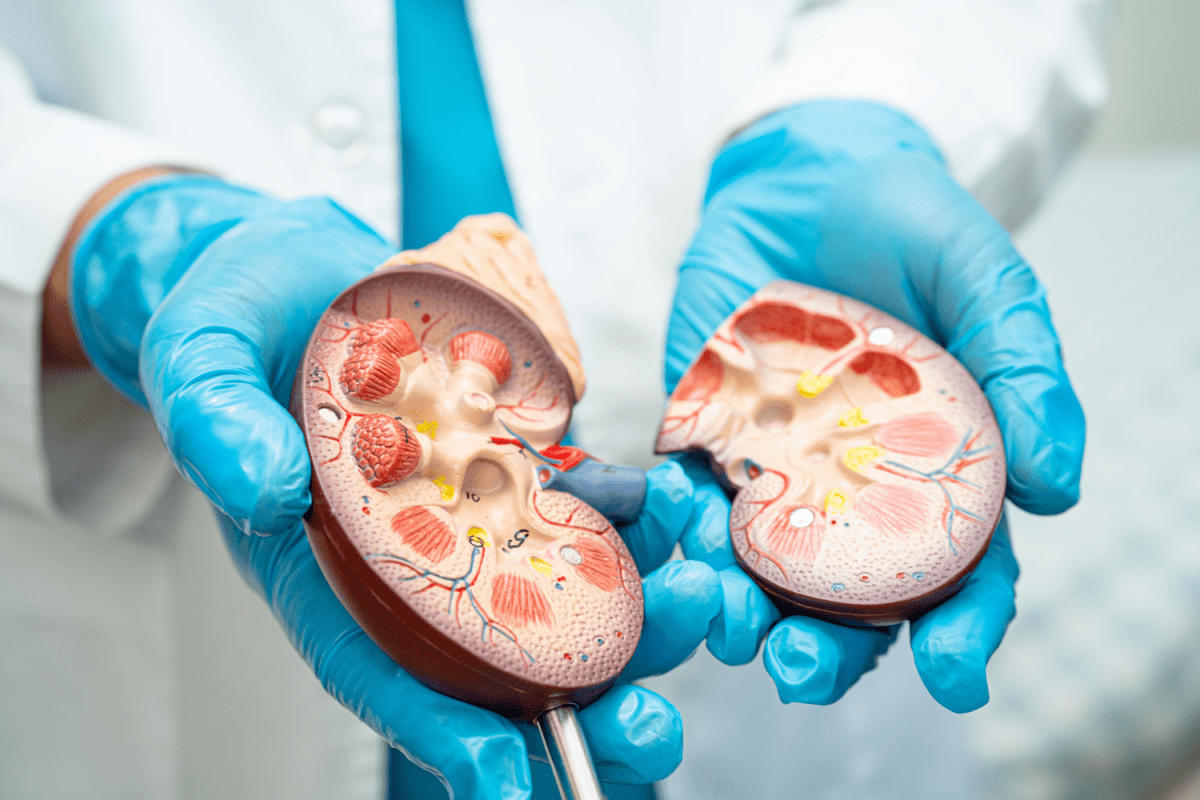
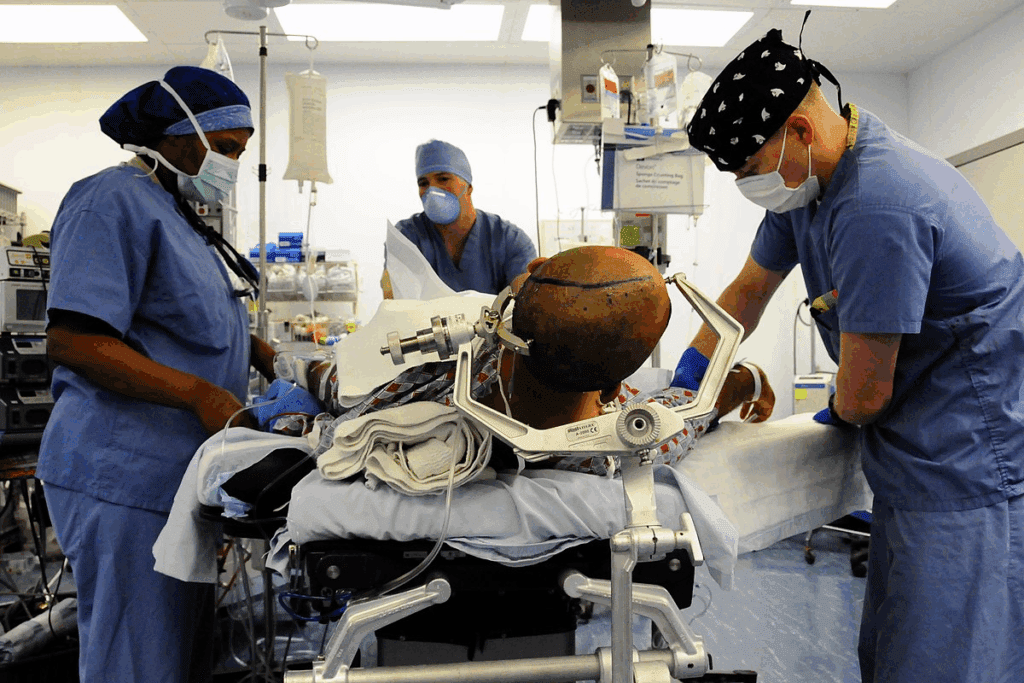
The Brain Tumor Surgical Process
Brain tumor surgery is a detailed process. It’s tailored to the tumor’s type and the patient’s health.
Types of Surgical Resections
Surgical resections for brain tumors vary based on how much is removed. The main types are:
- Gross Total Resection (GTR): Removing the whole tumor
- Subtotal Resection (STR): Taking out most of the tumor, but some stays
- Biopsy Only: Taking a small tumor sample for diagnosis
The choice of surgery depends on the tumor’s location, size, and type. It also depends on the patient’s health and brain function.
Importance of Surgical Margins
Clear surgical margins are key in brain tumor surgery. They mean no tumor cells are left at the edge of the removed tissue. This can greatly affect how likely the tumor is to come back.
But, getting clear margins is hard because of the brain’s complex structure. Surgeons use special techniques and tools to try to achieve this. They also plan carefully before surgery using advanced imaging.
How Fast Can Brain Tumors Grow Back After Surgery?
After surgery, brain tumors can grow back, and how fast they do depends on several things. These include the type of tumor, how much of it was removed, and any additional treatments. Each case is different, showing how complex brain tumors are and why treatments need to be tailored.
General Recurrence Timelines
How long it takes for brain tumors to come back varies a lot. Some may return in just a few months, while others might not show up again for years. The time to recurrence can depend on the tumor’s type and how aggressive it is. For example, aggressive tumors tend to come back sooner than less aggressive ones.
Research shows that some brain tumors can come back as high as 80% within two years after surgery. But, this number can change based on how much of the tumor was removed and if additional treatments were used.
Factors Affecting Regrowth Speed
Several things can affect how fast brain tumors come back after surgery. These include:
- The type and grade of the tumor, with higher-grade tumors typically recurring more quickly.
- The extent of surgical resection, with more complete resections generally associated with longer times to recurrence.
- The presence of residual tumor cells post-surgery, which can lead to earlier recurrence.
- The use and effectiveness of adjuvant therapies such as radiation and chemotherapy.
- Patient-specific factors, including age and overall health status.
Understanding these factors is key to managing patient expectations and tailoring post-surgical care. By looking at each patient’s tumor and how they respond to treatment, doctors can create better plans for follow-up and treatment.
Recurrence Rates by Tumor Type
Different brain tumors have their own recurrence rates. It’s key to know these rates for the best care. The chance of a tumor coming back depends on its type, grade, and genetics.
High-Grade Gliomas
High-grade gliomas, like glioblastoma, grow fast and often come back. Research shows glioblastoma can recur up to 90% within two years. The glioblastoma recurrence rate is high, with most recurrences happening 6-12 months after treatment.
Low-Grade Gliomas
Low-grade gliomas have a lower chance of coming back. But, they can grow into more serious tumors over time. The glioma regrowth speed varies, with some growing slowly over years.
Meningiomas
Meningiomas, which grow from the brain’s meninges, usually have a better outlook. The meningioma return rate depends on the tumor’s grade and how much of it was removed. Benign meningiomas (WHO Grade I) are less likely to come back than atypical (WHO Grade II) or malignant (WHO Grade III) ones.
Other Common Brain Tumor Types
Other tumors, like astrocytomas and oligodendrogliomas, also have specific recurrence patterns. The astrocytoma recurrence timeline can differ, with higher grades leading to more recurrences. Oligodendroglioma regrowth is often linked to genetic traits, like the 1p/19q codeletion.
Knowing these recurrence rates helps in creating better follow-up plans. This improves patient outcomes. We’ll look at more factors affecting brain tumor recurrence next.
Factors That Influence Brain Tumor Recurrence
Understanding what makes brain tumors come back is key to better treatment. Brain tumor recurrence is complex, influenced by many factors. We’ll look at these factors to understand their impact and how doctors can tailor treatments.
Tumor Grade and Aggressiveness
The grade and how aggressive a brain tumor is play big roles in recurrence. High-grade tumors are more aggressive and likely to come back than low-grade tumors. The World Health Organization (WHO) grading system helps classify tumors based on their features.
Tumors with lots of cell division, blood vessel growth, and dead cells are high-grade. Knowing the tumor grade helps doctors predict recurrence and plan treatments.
Extent of Surgical Resection
The amount of tumor removed during surgery is also key. The goal is to remove as much tumor as possible while keeping brain tissue safe. Gross total resection lowers recurrence risk more than subtotal resection.
Extent of Resection | Recurrence Rate | Prognosis |
Gross Total Resection | Lower | Favorable |
Subtotal Resection | Higher | Guarded |
Molecular and Genetic Factors
Molecular and genetic factors greatly influence brain tumor behavior and recurrence risk. Certain genetic changes and molecular pathways affect tumor aggressiveness and treatment response.
For example, IDH1 and IDH2 gene mutations are linked to better outcomes in gliomas. Knowing these molecular details helps tailor treatments and find new targets.
Patient Age and Overall Health
Patient age and health also impact recurrence. Older patients often face poorer outcomes and higher recurrence rates. This is due to decreased physical strength and more health issues.
Also, a patient’s overall health and immune system affect treatment tolerance and response. A thorough assessment of these factors is vital for effective treatment planning.
The Role of Tumor Location in Recurrence
The place of a tumor in the brain can change how hard surgery is and the chance of the tumor coming back. The brain’s complex structure and function make some tumor spots harder to treat.
Challenging Locations for Complete Resection
Some brain tumor spots are harder to remove completely because of their closeness to important brain parts or their deep location. Tumors near areas that control speech or movement need careful surgery to avoid harm. Specifically, these hard spots include:
- Tumors in the brainstem, which controls many vital functions
- Tumors near major blood vessels or critical neural pathways
- Tumors in deep-seated areas, such as the thalamus or basal ganglia
Impact on Recurrence Timelines
The spot of a brain tumor can greatly affect when it might come back. Tumors in hard spots might not be removed completely, leading to quicker return. Studies have shown that tumors in certain spots have different patterns of coming back, showing why where the tumor is matters in treatment planning.
Multifocal and Diffuse Tumors
Multifocal and diffuse tumors are special challenges for surgery and recurrence risk. These tumors can start in many places or spread all over the brain, making full removal hard or impossible. Managing these tumors often needs a mix of treatments, like surgery, radiation, and chemotherapy.
Knowing how tumor location affects recurrence is key for making good treatment plans. By understanding the specific challenges of a tumor’s location, doctors can tailor treatments better for each patient.
Post-Surgical Residual Disease
Post-surgical residual disease is a big factor in brain tumor recurrence and patient outcome. After surgery, leftover disease can greatly affect treatment success and survival chances.
Microscopic vs. Visible Residual Tumor
Residual disease can be tiny or big. Microscopic residual tumor is too small to see with the naked eye but can be found with special tests. Visible residual tumor is big enough to see during surgery or on scans.
Knowing the difference is key. It helps decide on extra treatments and the best plan for care. We’ll look at how these differences affect when tumors come back.
How Residual Cells Lead to Recurrence
Cells left behind can cause tumors to come back in several ways:
- They can grow back.
- They might not respond to treatments.
- They can spread to nearby brain tissue.
It’s important to understand these ways to fight recurrence with targeted treatments.
Techniques to Identify Residual Disease
Finding leftover disease is key for planning care after surgery. We use:
- Advanced imaging modalities like MRI and PET scans.
- Molecular diagnostics to spot tiny diseases.
- Intraoperative fluorescence-guided surgery to see tumor edges.
These methods help figure out how much disease is left and guide treatment choices.
By using these methods together, we can understand how much disease is left. This helps us make treatment plans that work better for patients.
Early vs. Late Recurrence Patterns
After brain tumor surgery, tumors can come back early or late. Each type has its own effects on patient outcomes. Knowing these recurrence patterns helps create better plans for watching and treating tumors.
Rapid Recurrence: Causes and Implications
Rapid recurrence means a tumor comes back soon after surgery. It can happen for many reasons, like the tumor being very aggressive or not being fully removed. Rapid recurrence often means a worse outlook and might need stronger treatments.
The reasons for quick recurrence are complex. They involve the tumor itself and how much of it was removed. Research shows that tumors with high-grade histology or not fully removed tend to come back sooner.
Delayed Recurrence: Patterns and Significance
Delayed recurrence, on the other hand, is when a tumor comes back after a long time after surgery. It can be influenced by how well treatments worked, changes in the tumor, and late-emerging disease.
The importance of delayed recurrence is in its impact on long-term care. Patients with delayed recurrence might need changes in their treatment plans. This could include new therapies or joining clinical trials.
Understanding the difference between early recurrence and late recurrence helps doctors tailor care for each patient. This approach can lead to better outcomes and a better quality of life.
Detecting Brain Tumor Recurrence
Knowing how to spot brain tumor recurrence is key to better patient care. Finding it early means we can act fast. This can greatly improve treatment success.
Imaging Techniques for Monitoring
Imaging is vital for keeping an eye on brain tumors. We mainly use MRI and CT scans for this.
MRI is great for spotting soft tissue issues, perfect for brain tumors. CT scans are quicker and more common, used in emergencies or when MRI isn’t possible.
Distinguishing Between Recurrence and Treatment Effects
Telling if it’s a tumor coming back or treatment side effects is hard but very important. Side effects can look like a tumor on scans.
Special MRI scans and MR spectroscopy help tell them apart. They give us detailed info about the tissue.
Recommended Monitoring Schedules
How often we need to scan depends on the tumor type, grade, and the patient’s health. High-grade tumors usually need more checks.
Tumor Type | Monitoring Frequency |
High-Grade Gliomas | Every 3-6 months |
Low-Grade Gliomas | Every 6-12 months |
Meningiomas | Every 6-12 months |
Warning Signs of Brain Tumor Regrowth
Knowing the signs of brain tumor regrowth is very important. After surgery, it’s key for patients to watch for warning signs. This can help a lot in patient care.
Common Symptoms of Recurrence
Brain tumor regrowth can show in many ways. Some common signs are:
- Headaches: Often more severe or frequent than before.
- Seizures: New or increased seizure activity.
- Cognitive Changes: Memory issues, confusion, or difficulty concentrating.
- Motor Symptoms: Weakness, numbness, or difficulty with coordination and balance.
- Visual Disturbances: Blurred vision, double vision, or loss of peripheral vision.
These symptoms can change based on the tumor’s location and size. It’s important for patients to watch their condition closely. They should tell their healthcare provider about any new or worsening symptoms.
When to Contact Your Doctor
If you notice any of these, contact your doctor right away:
- A sudden increase in the severity or frequency of symptoms.
- New symptoms that were not present before.
- Difficulty with speech, vision, or motor functions.
- Changes in personality or cognitive function.
Spotting recurrence early can greatly improve treatment options and outcomes. Your healthcare team can best assess your symptoms and guide you.
Differentiating Normal Recovery from Recurrence Signs
Telling normal recovery symptoms from signs of recurrence can be hard. Generally, recurrence symptoms are:
- Persistent or worsening over time.
- Different from the typical post-surgical recovery symptoms.
- Accompanied by new neurological deficits.
If you’re unsure about your symptoms, talk to your healthcare provider. They can do the needed tests, like imaging studies, to figure out what’s causing your symptoms.
Being alert to brain tumor regrowth signs and talking openly with your healthcare team are key for good care after surgery.
Treatment Options for Recurrent Brain Tumors
When a brain tumor comes back, finding the right treatment is key. Doctors look at different options to see what works best. They often mix treatments to fit each patient’s needs.
Second Surgery Considerations
If the tumor is in a spot that’s easy to reach, surgery might be an option. The choice to have surgery again depends on several things. These include where the tumor is, how big it is, and the patient’s health. Advances in surgical techniques have helped many patients get better after surgery again.
Radiation Therapy for Recurrence
Radiation therapy is often used for brain tumors that come back. It’s used when surgery isn’t possible. Different types of radiation therapy are chosen based on the tumor and what treatments have been tried before.
Chemotherapy and Drug Options
Chemotherapy is important for treating brain tumors that come back. The right drugs depend on the tumor type, past treatments, and the patient’s health. Targeted therapies and new drugs are being tested to find better treatments.
Emerging Treatments and Clinical Trials
New treatments like immunotherapy and gene therapy are being tested in clinical trials. Participation in clinical trials lets patients try new treatments. This helps doctors find better ways to treat brain tumors that come back.
In summary, treating brain tumors that come back needs a mix of treatments. This includes surgery, radiation, chemotherapy, and new treatments. Clinical trials are also key in finding new ways to help patients.
Adjuvant Therapies to Prevent or Delay Recurrence
After brain tumor surgery, adjuvant therapies are key to prevent or delay recurrence. These treatments aim to get rid of any tumor cells left behind. This helps lower the chance of the tumor coming back.
We take a full approach to adjuvant therapies. This includes post-surgical radiation, chemotherapy, and targeted and immunotherapies. Each treatment is picked based on the tumor type, grade, and the patient’s health.
Post-Surgical Radiation
Post-surgical radiation therapy kills any leftover tumor cells in the brain. Radiation therapy can be delivered externally or internally, depending on the tumor. External beam radiation therapy (EBRT) is common, using a machine outside the body to target the tumor.
The goal is to stop the tumor from coming back by getting rid of tiny cells left after surgery. The timing and dose of radiation are planned carefully to work well and cause fewer side effects.
Chemotherapy Protocols
Chemotherapy is another treatment for brain tumors. Chemotherapy protocols vary based on the tumor type, grade, and patient’s health. It can be taken orally or through an IV, and sometimes directly into the cerebrospinal fluid.
The choice of chemotherapy agents and how long treatment lasts depends on the patient. We often mix chemotherapy with other treatments like radiation to make it more effective.
Targeted and Immunotherapies
Targeted therapies and immunotherapies are new and promising for brain tumors. Targeted therapies target specific molecular abnormalities that cause tumors to grow. Immunotherapies boost the body’s immune system to fight tumor cells.
These treatments offer hope for patients with brain tumors, even those with aggressive or recurring tumors. We’re always looking for new ways to use targeted and immunotherapies to help patients and reduce recurrence risk.
Lifestyle Factors and Brain Tumor Recurrence
Recent studies show that lifestyle choices can help lower the risk of brain tumors coming back after surgery. We’re learning more about how our lifestyle affects brain tumor recurrence. Several key areas stand out as very important.
Nutrition and Supplementation
Eating a balanced diet full of important nutrients is key for health. It might help lower the chance of tumors coming back. Nutritional supplements can also help, but always talk to a doctor first to find the right ones for you.
Some foods and nutrients are good for preventing brain tumor recurrence. Eating foods high in antioxidants, like fruits and veggies, is beneficial. Omega-3 fatty acids in fish and nuts are also good.
Stress Management and Quality of Life
Stress management, like meditation and yoga, can greatly improve life for patients. These methods help deal with the emotional side of having a brain tumor. They might also help prevent recurrence.
Keeping a good quality of life involves many things. This includes getting psychological support, staying connected with others, and doing things that make you happy.
Exercise and Physical Activity Benefits
Regular exercise and physical activity are good for many reasons. They might even lower the risk of tumors coming back. Physical activity helps manage stress, boosts mood, and keeps you physically fit.
It’s important for patients to work with their healthcare team. They can help create a workout plan that fits their health and abilities.
Psychological Impact of Tumor Recurrence Risk
The risk of brain tumor recurrence can deeply affect patients and their families. This uncertainty can change many parts of their lives.
Coping with Uncertainty
Dealing with the risk of tumor recurrence needs a wide approach. Mindfulness practices like meditation and deep breathing can help with anxiety. Cognitive-behavioral therapy (CBT) also helps by changing negative thoughts.
It’s important for patients to keep in touch with their support networks. This includes family, friends, and support groups. Sharing feelings with others who get it can make a big difference.
Support Resources for Patients and Families
Having access to good support resources is key. This includes psychological counseling, support groups, and educational materials. Many hospitals have special programs for brain tumor patients, with services like counseling and rehab.
Families can learn to support their loved ones better. This means understanding their needs, recognizing signs of recurrence, and knowing the healthcare system.
Communicating with Your Healthcare Team
Talking well with your healthcare team is vital. Patients should ask about their condition, treatment options, and any worries. Regular check-ups can catch changes early, helping outcomes.
Patients should also share their fears and anxieties with their doctors. This way, they get reassurance, guidance, and support that fits their needs.
By using these strategies, patients and their families can handle the psychological effects of tumor recurrence risk better. This improves their quality of life.
Advances in Preventing Brain Tumor Regrowth
We’re getting better at stopping brain tumors from coming back. New discoveries in neuro-oncology bring hope to those affected. This is a big step forward.
New Surgical Techniques
New ways to operate on brain tumors are making a difference. Fluorescence-guided surgery and intraoperative MRI help doctors remove tumors more accurately. This means they can take out more of the tumor without harming the brain.
Innovative Treatment Approaches
New treatments are being tested too. Targeted therapies and immunotherapies are designed to attack tumors in new ways. They could lead to better results with fewer side effects.
Promising Research Directions
Scientists are studying brain tumors to find new treatments. They’re looking at the tumor’s environment and how stem cells play a role. This research could lead to even better treatments in the future.
Advance | Description | Potential Benefit |
Fluorescence-Guided Surgery | Uses fluorescent dyes to highlight tumor tissue during surgery | More complete tumor removal |
Targeted Therapies | Drugs that target specific genetic mutations in tumors | Reduced side effects, improved efficacy |
Immunotherapies | Treatments that use the immune system to fight cancer | Potential for long-term tumor control |
Conclusion
Understanding brain tumor recurrence is key to better treatment plans and outcomes. We’ve looked at how tumor type, grade, and location affect recurrence. We also discussed the importance of surgery and other treatments.
Stopping brain tumor recurrence needs a team effort. New surgical methods, radiation, and chemotherapy have helped patients. Research into new treatments, like targeted and immunotherapies, is also promising.
As we learn more about brain tumors, we see the need for a detailed approach to treatment. By combining knowledge of tumor biology, surgery, and other treatments, we aim to help more patients. This way, we can improve the lives of those with brain tumors.
FAQ
How fast can a brain tumor grow back after surgery?
The speed of recurrence depends on the tumor type, its grade, and how much was removed. Some tumors may regrow quickly, while others take months or years to recur.
What factors influence brain tumor recurrence?
Factors include the tumor’s biology, completeness of surgical removal, patient’s overall health, and post-operative care. Understanding these helps doctors plan follow-up and treatment.
What are the different types of brain tumors and their recurrence rates?
Different tumors have varying risks of returning. High-grade gliomas are more likely to recur quickly, whereas low-grade gliomas and meningiomas often have lower recurrence rates.
How does the extent of surgical resection impact recurrence?
The more tumor that can be safely removed during surgery, the lower the risk of recurrence. Complete resection helps reduce the chance of regrowth.
What is the role of post-operative treatments in preventing or delaying recurrence?
Post-operative therapies like radiation, chemotherapy, targeted therapy, and immunotherapy help reduce the likelihood of tumor regrowth and improve long-term outcomes.
How can lifestyle factors impact brain tumor recurrence?
Healthy lifestyle choices—such as balanced nutrition, exercise, stress management, and avoiding harmful habits—can support recovery and overall well-being, although their direct effect on tumor recurrence is limited.
What are the common symptoms of brain tumor recurrence?
Symptoms may include headaches, seizures, vision changes, or cognitive difficulties. Any new or worsening symptom should be promptly reported to your doctor.
How is brain tumor recurrence detected?
Recurrence is usually detected through imaging tests like MRI or CT scans. Sometimes additional scans are needed to distinguish new tumors from regrowth.
What are the treatment options for recurrent brain tumors?
Treatment may include repeat surgery, radiation, chemotherapy, targeted therapies, immunotherapy, or participation in clinical trials exploring new approaches.
How can patients cope with the psychological impact of tumor recurrence risk?
Emotional support, counseling, open communication with healthcare providers, support groups, and stress management techniques can help patients manage anxiety about recurrence.
What advances are being made in preventing brain tumor regrowth?
Advances include improved surgical techniques, new radiation methods, targeted therapies, immunotherapies, and research into genetic and molecular tumor profiling to personalize treatment.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC2467481/