Last Updated on November 13, 2025 by
Keeping platelet levels healthy is key for cancer patients on chemo. Chemotherapy-induced thrombocytopenia (CIT) affects up to 25% of patients. This puts them at risk for serious problems.
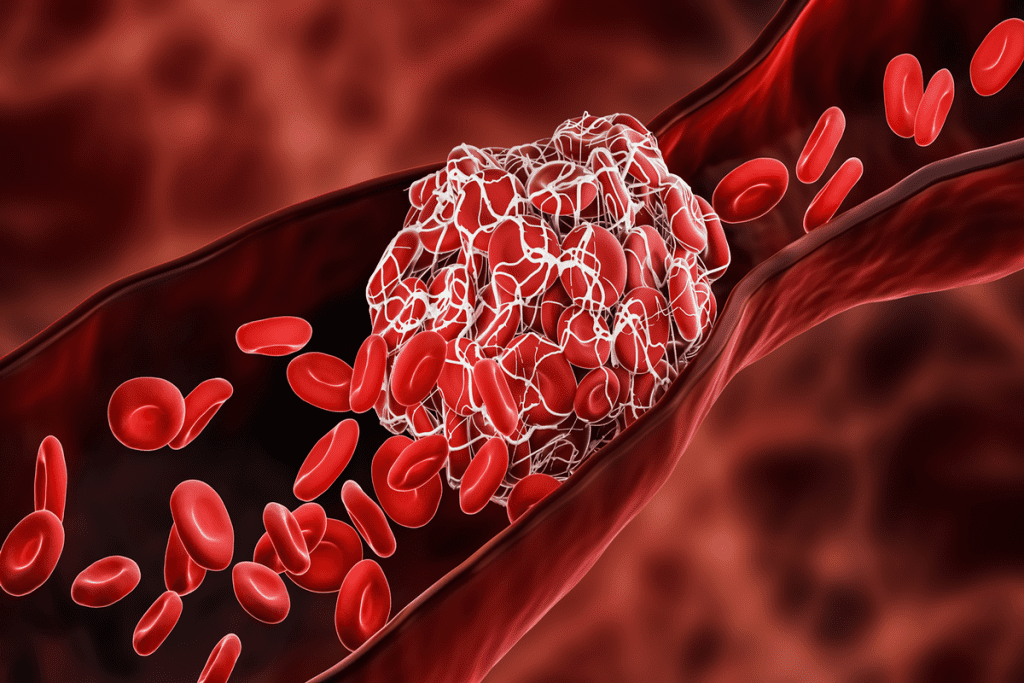
Platelets are important for stopping bleeding from damaged blood vessels. A normal count is between 150,000 to 450,000 platelets per microliter of blood. If counts drop, patients face risks of bruising, bleeding, and more.
We’ll look at ways to keep platelet levels up during chemo. This is based on top research and care protocols. Knowing about chemotherapy-induced thrombocytopenia and how to manage it is vital for supporting patients. How to increase platelet count during chemo? Discover strategies to combat thrombocytopenia and reduce the dangerous risk of bleeding.
Keeping platelet levels healthy is key during chemotherapy. But first, we must know what platelets do. Platelets are tiny, colorless parts in our blood that help stop bleeding by forming clots. They are vital for healing injuries and preventing too much bleeding.
Platelets, or thrombocytes, are made in the bone marrow and move through our blood. Their main job is to stick together and form clots. This stops bleeding when a blood vessel gets hurt. A normal count is between 150,000 to 450,000 platelets per microliter of blood. Having enough platelets is key to avoiding bruising and bleeding problems.
Chemotherapy attacks fast-growing cells, including those in the bone marrow that make platelets. This can lower platelet production, causing thrombocytopenia (low platelet count). The severity of this issue depends on the type and amount of chemotherapy.
A low platelet count raises the risk of bleeding and bruising. People with thrombocytopenia might see petechiae (small red or purple spots on the skin), nosebleeds, and bleeding gums. In serious cases, it can cause dangerous bleeding. Knowing these risks is important for managing them during chemotherapy.
Chemotherapy-induced thrombocytopenia, or CIT, is a big worry for cancer patients. It happens when there are too few platelets in the blood. This can make it easier to bleed.
“Thrombocytopenia is a common side effect of chemotherapy, affecting up to 25% of cancer patients,” says medical research. This condition makes treatment harder and affects the patient’s life quality a lot.
CIT means having fewer than 150,000 platelets per microliter of blood. How common it is depends on the chemotherapy and the patient’s health.
CIT happens because chemotherapy weakens the bone marrow. This makes it hard for the bone marrow to make platelets. It’s a big worry because it can make chemotherapy less effective.
CIT can mess up cancer treatment plans. If platelet counts get too low, chemotherapy might be delayed or the dose lowered. This is to avoid more problems.
“Dose adjustments or treatment delays due to CIT can compromise the efficacy of cancer treatment,” say oncology experts. It’s important to manage CIT well to keep the treatment on track and get the best results.
Knowing the signs of low platelet counts is key. Look out for a lot of bruising, nosebleeds, bleeding gums, and cuts that won’t stop bleeding.
In serious cases, CIT can cause dangerous bleeding. Patients and their caregivers should watch for these signs and tell their doctor right away.
Understanding CIT helps patients deal with their cancer treatment better. Managing CIT well is important to keep treatment on track and care for the patient.
Understanding how to increase platelet count during chemotherapy is important for patient safety. Medical treatments are key in managing low platelet counts during chemotherapy. Healthcare providers use several strategies to help. This is to reduce the risks of low platelet counts.
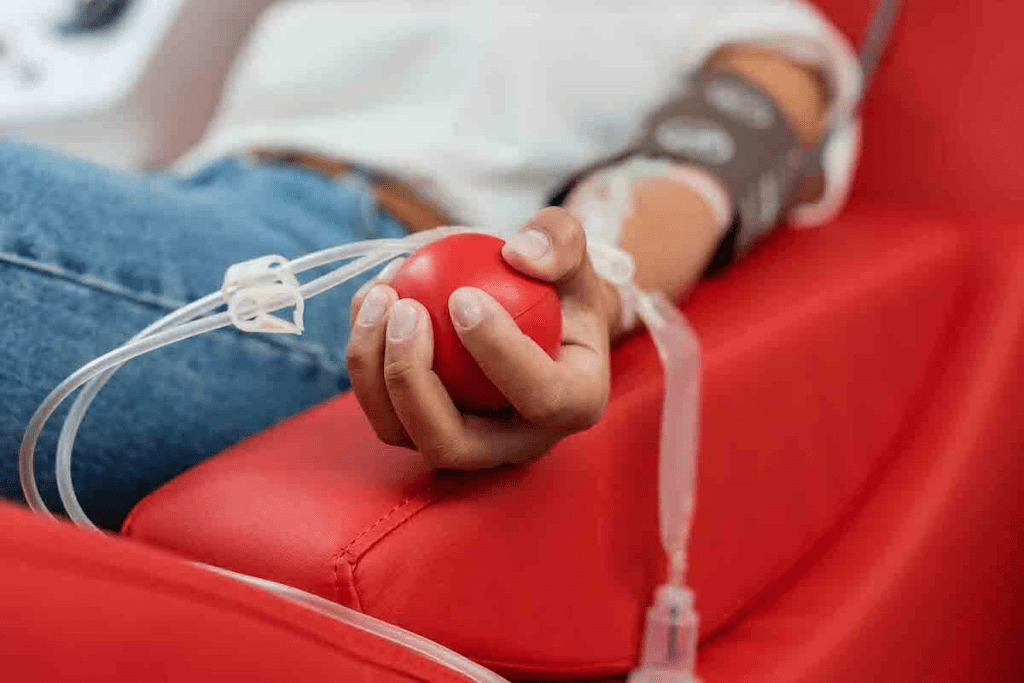
Platelet transfusions are often used for low platelet counts. They involve giving platelet-rich blood to boost the count. This is very important when counts are very low or when there’s a risk of bleeding.
Platelet transfusions help with bleeding or before surgery. But, they can cause allergic reactions or other problems. So, doctors decide on a case-by-case basis, considering the patient’s health and treatment.
Thrombopoietin receptor agonists (TPO-RAs) help make more platelets in the bone marrow. Romiplostim is a TPO-RA used for low platelet counts from chemotherapy. Studies show it helps avoid dose changes in 84% of patients.
TPO-RAs work like thrombopoietin, a hormone that helps platelet production. They activate receptors on bone marrow cells, helping platelets mature and enter the blood.
Cryopreserved platelets are another option for low counts in cancer patients. These frozen platelets are ready for use when needed. They are safe and effective, helping patients with chemotherapy.
Cryopreserved platelets are great in emergencies or when other platelets aren’t available. They ensure patients get the platelet support they need to keep up with treatment.
Certain foods can help boost platelet production, which can be low after chemotherapy. Eating a balanced diet with key nutrients is important for healthy platelets.
Some vitamins are key for making platelets. Vitamin K helps with blood clotting and is found in spinach and kale. Vitamin B12 is vital for platelet production and is in meat, fish, and dairy. Vitamin C boosts white blood cells and is in citrus fruits, strawberries, and bell peppers. Folate, or vitamin B9, is important for blood cells and is in legumes, nuts, and dark greens.
Protein is key for making new platelets. Eat foods high in protein like lean meats, fish, eggs, and legumes. Nuts and seeds are also good protein sources and can be added to meals or snacks.
Drinking enough water is vital for healthy blood cells, including platelets. It helps the body work right. Drink lots of water all day.
Here’s a meal plan to help with platelet production during chemotherapy:
This meal plan has foods full of vitamins and minerals good for platelets.
To keep platelet levels healthy during chemotherapy, making smart lifestyle choices is key. We can do this by choosing safe physical activities, managing stress well, getting enough sleep, and staying away from things that could cause bleeding.
Doing gentle exercises during chemotherapy can boost your immune system and health. Short walks, yoga, or light stretching are good choices. They help keep blood flowing and lower stress without putting too much strain on your body.
Before starting any new exercise, always talk to your doctor. They can give advice that fits your specific situation and treatment plan.
Stress can hurt your immune system, making it important to manage it during chemotherapy. Meditation, deep breathing, or mindfulness can help lower stress and improve your overall health.
Doing things that make you happy and relaxed, like reading, listening to music, or being with loved ones, also helps manage stress.
Good sleep is essential for your body to make new blood cells, including platelets. Having a regular sleep schedule and a cozy sleep area can improve your sleep quality.
Strategies like staying away from caffeine and screens before bed and using relaxation techniques can also help you sleep better.
During chemotherapy, it’s important to avoid activities that could cause bleeding or injury. This means staying away from contact sports, using sharp objects carefully, and being careful when doing things that could cause bruises or cuts.
By being careful and taking the right precautions, you can help keep your platelet levels healthy and stay safe during treatment.
When chemotherapy lowers platelet counts too much, quick action is key. We know how serious this can be. Here, we’ll talk about fast ways to boost platelet counts. These steps are important for those who need to keep up with treatment or avoid bleeding risks.
For very low platelet counts, doctors must act fast. Platelet transfusions are often used to quickly raise counts. We also use drugs that help make more platelets. These steps are key to managing low platelet risks.
Boosting platelets in just 2 days is tough, but some methods can help. While quick increases are hard, transfusions can offer quick relief. Eating right and staying hydrated also help with blood cell production.
Knowing when to go to the emergency room is important. Signs like bad bruising, bleeding gums, or hard-to-stop nosebleeds mean platelet counts are too low. If you see these signs, get help right away.
At times, changing your chemotherapy plan might help your platelets recover. We work with you to find the right balance. This means managing cancer treatment while watching out for side effects.
Managing platelets during chemotherapy needs teamwork with your healthcare team. Together, you can spot problems early and adjust your treatment to keep platelet counts safe.
Talking openly with your oncologist is key for platelet management. Ask questions like:
Knowing the answers helps you be more involved in your care.
Tell your healthcare team about any symptoms right away. Keep a record of any unusual bleeding or bruising. This helps your doctors make better decisions for you.
At times, changing your chemotherapy dose is needed to help platelet counts recover. Your team will check your platelet levels and other factors to decide if a change is needed. This ensures your treatment works well without risking low platelet counts.
Centers like LIV Hospital have advanced platelet management plans. They might use new treatments to help make more platelets. Talk to your oncologist about these options for your care.
Working closely with your healthcare team and knowing your treatment options helps you face chemotherapy challenges. Remember, managing platelet counts is a big part of your cancer treatment plan.
Knowing and tracking your platelet levels is key to better chemotherapy results. Regular checks help spot problems early. This way, you can get help right away.
A Complete Blood Count (CBC) is a key test that checks your blood’s parts, like platelets. Understanding your CBC results is important for managing your platelet levels well. Your healthcare team will go over these results with you. They’ll explain what your platelet count and other blood values mean.
The CBC test shows your blood cell counts, including white blood cells, red blood cells, and platelets. By looking at these numbers, your healthcare providers can check your health. They can then decide the best treatment plan for you.
How often you get blood tests during chemotherapy depends on several things. These include the type of chemotherapy, your health, and your treatment plan. Usually, blood tests are done before each chemotherapy session to make sure your blood counts are safe for treatment.
Your healthcare team will figure out the best schedule for your blood tests. They’ll make sure you’re monitored closely but also avoid too many blood draws.
Today, there are many digital tools and apps to track your health, including platelet counts. Using digital tools lets you be more involved in your care. You can watch trends and share your data with your healthcare providers.
Before each chemotherapy session, your healthcare team checks your blood counts. They make sure they’re safe for treatment. Specific thresholds for platelet counts, white blood cell counts, and other parameters must be met to continue treatment.
Knowing these thresholds and how they affect your treatment can help you understand your chemotherapy better.
Keeping platelet levels healthy is key for cancer patients on chemotherapy. We’ve looked at ways to boost platelet production. This includes medical treatments, diet changes, and lifestyle tweaks.
Medical steps like platelet transfusions and certain drugs can help with low counts. Eating foods rich in vitamins K, B12, C, and folate helps. Drinking enough water also supports blood cell making. Safe exercise, managing stress, and good sleep are also important.
Knowing the dangers of low platelet counts and teaming up with your healthcare is essential. This way, you can manage your platelet health well during cancer treatment. Stay informed and active in caring for your platelets for the best results.
A normal platelet count is between 150,000 to 450,000 platelets per microliter of blood. Counts outside this range might show a problem.
Chemotherapy can slow down bone marrow activity. This leads to fewer platelets and might cause thrombocytopenia.
Low platelet counts raise the risk of bleeding and bruising. They can even lead to serious hemorrhages. This might make treatment harder and need changes in the schedule.
You can get platelet transfusions or use thrombopoietin receptor agonists (TPO-RAs). Eating foods rich in vitamins K, B12, C, and folate helps too. Also, staying active, managing stress, and drinking enough water supports platelet health.
Some treatments can quickly raise platelet counts. But, a 2-day increase is hard. If your counts are very low, you need to see a doctor right away. How fast you can increase depends on your situation.
Foods high in vitamins K, B12, C, and folate, and proteins, help make more platelets. Good examples are leafy greens, citrus fruits, nuts, and lean meats.
How often you get blood tests depends on your treatment and how you react. Usually, you’ll have tests weekly or before each treatment.
Look out for a lot of bruising, small red spots on the skin, bleeding gums, nosebleeds, and heavy periods. If you have severe symptoms, get help right away.
Try meditation, deep breathing, yoga, and getting enough sleep. These can help your immune system and overall health.
TPO-RAs are medicines that make the bone marrow make more platelets. They help with low platelet counts, including those caused by chemotherapy.
Go to the emergency room for severe bleeding, a lot of bruising, or other serious signs of low platelet counts.
Use digital tools or apps to track your counts. Keeping a log of your blood test results and talking to your healthcare team often is also good.
The minimum platelet count needed varies based on your treatment and health. Your oncologist will decide what’s safe for you.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!