Patients with thrombocytopenia need to stay away from medicines that can lower platelet counts. These drugs can also increase the risk of bleeding. It’s important to know which medicines can make this condition worse.
The ITP Support Association says some drugs can cause low platelet counts through allergic reactions. Heparin, furosemide, and nonsteroidal anti-inflammatory drugs (NSAIDs) are examples. We will talk about the medicines to avoid for those with thromWhat are the early warning signs of lymphoma?bocytopenia. We’ll also give tips on how to manage this condition.
Key Takeaways
- Certain medications can worsen thrombocytopenia.
- Avoiding drugs that can further reduce platelet counts or increase bleeding risk is important.
- Medicines like heparin, furosemide, and NSAIDs can lead to low platelet counts.
- Knowing the causes of low platelet counts is key to good care.
- People with thrombocytopenia should be careful with their medications.
Understanding Thrombocytopenia and Medication Risks
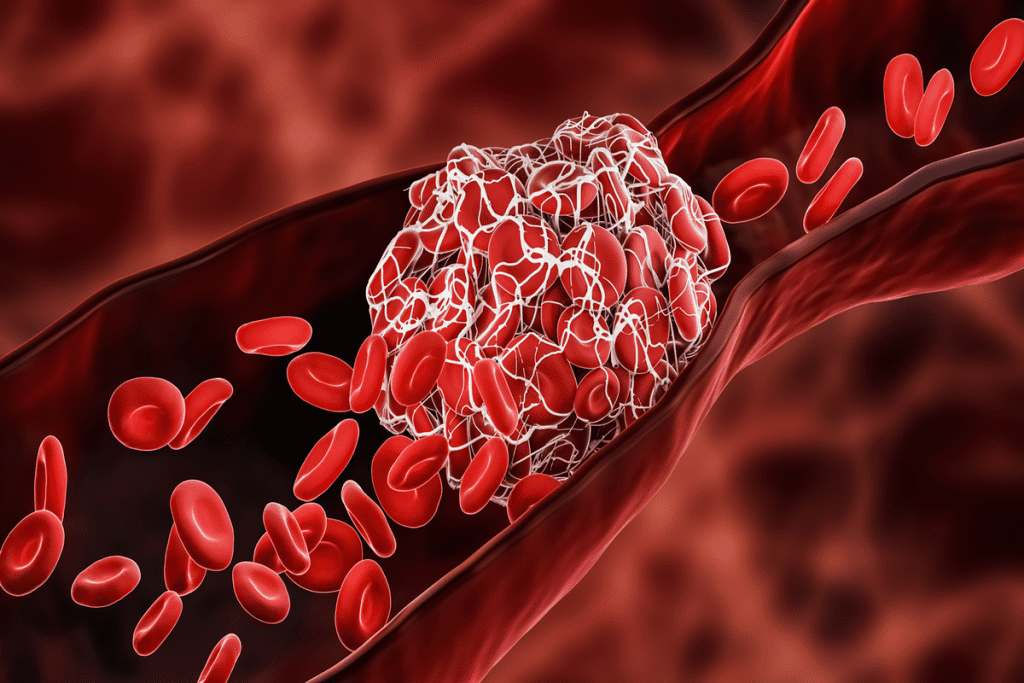
It’s important to know how medications can affect thrombocytopenia. This condition, marked by low platelet counts, increases the risk of bleeding and bruising. Some drugs can harm platelets or stop the bone marrow from making them.
Definition and Normal Platelet Ranges
Thrombocytopenia happens when platelet counts fall below 150,000 per microliter of blood. Platelet counts usually range from 150,000 to 450,000. A low count can cause thrombocytopenia symptoms like easy bruising and prolonged bleeding.
A normal platelet count is key to blood clotting. Low counts can make even small injuries bleed a lot.
How Medications Can Affect Platelet Counts
Over 300 drugs can cause thrombocytopenia, including heparin and some antibiotics. These drugs can either destroy platelets or stop the bone marrow from making them.
For example, heparin can trigger an immune response that destroys platelets. Some antibiotics and chemotherapy drugs can also lower platelet production by affecting the bone marrow.
| Medication Category | Examples | Potential Effect on Platelets |
| Anticoagulants | Heparin | Immune-mediated destruction |
| Antibiotics | Vancomycin, Sulfonamides | Bone marrow suppression |
| NSAIDs | Ibuprofen, Aspirin | Inhibit platelet function |
| Chemotherapeutics | Cisplatin, Methotrexate | Bone marrow suppression |
Importance of Medication Management
Managing thrombocytopenia well means being careful with medications. People with this condition should keep a close eye on their platelet counts. They should also work with their doctors to adjust their medications as needed.
It’s important for patients to tell their doctors about all the medications they take. This includes over-the-counter drugs and supplements, as they can also affect platelet counts.
Immune-Mediated Platelet Destruction
Some medications can cause the immune system to destroy platelets. This can lead to a quick drop in platelet counts and severe thrombocytopenia.
Understanding how this immune destruction happens is key to preventing and managing it.
NSAIDs and Platelet Function
Managing pain is hard for those with low platelets, thanks to NSAIDs. These drugs help with pain and swelling but harm platelets. This can lead to bleeding problems.
Ibuprofen and Related Medications
Ibuprofen and similar NSAIDs can make bleeding more likely. The ITP Support Association warns against using NSAIDs like ibuprofen because they mess with platelets sticking together.
Here are some NSAIDs to steer clear of:
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve)
- Ketoprofen (Orudis)
Aspirin’s Effect on Platelets
Aspirin also affects platelets by stopping them from sticking together. This effect can last for several days after aspirin is taken. It’s risky for those with low platelet counts.
Because of this, people with low platelets should avoid aspirin unless told to use it by their doctor.
Alternative Pain Management Options
For those with low platelets, finding other ways to manage pain is key. Acetaminophen (Tylenol) is safer than NSAIDs because it doesn’t affect platelets as much.
Other options include:
- Topical creams or gels for localized pain
- Physical therapy to improve mobility and reduce pain
- Consulting with a pain management specialist for personalized advice
Antiepileptic Drugs Associated with Thrombocytopenia
Antiepileptic drugs help manage seizures but can cause thrombocytopenia. This condition lowers platelet levels, leading to more bleeding and bruising. We’ll look at the risks of certain medications and how they affect platelets.
Concerns with Carbamazepine
Carbamazepine is a common drug for seizures, but it can cause thrombocytopenia. Medical News Today says it can trigger an immune response that destroys platelets. People taking carbamazepine should watch for signs like easy bruising or prolonged bleeding.
Monitoring is key for those on carbamazepine. Regular blood tests can catch any platelet count issues early, helping to act quickly.
Phenytoin and Its Effects on Platelets
Phenytoin, another seizure drug, is also linked to thrombocytopenia. It’s thought to affect the bone marrow’s platelet production. Patients should know the symptoms of low platelets, like petechiae and bleeding gums.
Safety Profiles of Newer Antiepileptics
Newer antiepileptic drugs might have fewer side effects, including less thrombocytopenia risk. Drugs like lamotrigine and levetiracetam are safer options for some. But it’s important for patients to talk to their doctors to find the best treatment.
We suggest patients talk to their healthcare provider about their medication if they have thrombocytopenia symptoms or concerns.
Chemotherapeutic Agents and Their Impact on Platelets
Chemotherapy is a key part of cancer treatment. It can greatly affect platelet counts. The drugs target fast-growing cells, including cancer cells and some healthy cells in the bone marrow.
The ITP Support Association says chemotherapy drugs can lower platelet counts. This happens because they slow down bone marrow production. This slowdown can cause thrombocytopenia, a condition with too few platelets.
Methotrexate Mechanisms
Methotrexate is a common chemotherapy drug. It stops DNA synthesis by blocking an enzyme. While it fights cancer, it can also harm platelet production in the bone marrow.
The effect of methotrexate on platelets depends on the dose and treatment length. It’s important to keep an eye on platelet levels for patients taking methotrexate.
Cisplatin and Bone Marrow Suppression
Cisplatin is another chemotherapy drug that can harm the bone marrow. It works by linking DNA in cancer cells, stopping them from growing. But, it can also slow down blood cell production, including platelets.
This bone marrow suppression can lead to thrombocytopenia. It’s key to manage this side effect to avoid bleeding problems.
Managing Cancer Treatment with Thrombocytopenia
Dealing with thrombocytopenia in chemotherapy patients needs a careful plan. This includes checking platelet counts often, adjusting drug doses, and finding ways to lower bleeding risks.
| Management Strategy | Description |
| Regular Blood Count Monitoring | Frequent checks on platelet counts to catch any significant drops early. |
| Dose Adjustment | Adjusting the dosage of chemotherapeutic agents to minimize bone marrow suppression. |
| Bleeding Precautions | Educating patients on how to minimize the risk of bleeding, such as avoiding sharp objects and using soft-bristled toothbrushes. |
Understanding how chemotherapy affects platelets and using the right management strategies can help reduce thrombocytopenia risks in cancer patients.
Over-the-Counter Medications and Supplements to Avoid with Thrombocytopenia
People with low platelet counts need to watch out for certain OTC meds and herbal supplements. These can raise the chance of bleeding. It’s key to know which ones to steer clear of.
Common OTC Pain Relievers
Many OTC pain meds can mess with platelet function. NSAIDs, like ibuprofen and naproxen, can make bleeding worse. Look for other ways to manage pain instead.
- Avoid NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve)
- Consider acetaminophen (Tylenol) for pain relief, but check with your doctor first
Herbal Supplements with Antiplatelet Effects
Some herbal supplements can also increase bleeding risk. Be careful with:
- Ginkgo biloba
- Garlic supplements
- Fish oil
- Vitamin E
These can interact with other meds or make bleeding worse. Always talk to a doctor before starting new supplements.
Reading Labels for Hidden Ingredients
Some OTC products have hidden ingredients that can affect platelets. Always read labels carefully.
- Check the active ingredients list for NSAIDs or other platelet inhibitors
- Be aware of combo products with multiple active ingredients
- Ask your pharmacist or doctor if you’re unsure about any ingredient
By being careful with OTC meds and supplements, you can manage your thrombocytopenia better. This helps lower the risk of serious problems.
Cardiovascular Medications to Approach with Caution
Using cardiovascular medications in patients with thrombocytopenia needs careful thought because of bleeding risks. Heart diseases are a big cause of illness and death worldwide. Managing them often means using different medicines. But, some heart drugs can make bleeding risks worse for those with low platelets.
Glycoprotein IIb/IIIa Inhibitors
Glycoprotein IIb/IIIa inhibitors are antiplatelet drugs used in angioplasty and for acute heart attacks. The ITP Support Association says these drugs can cause thrombocytopenia by destroying platelets. This can make bleeding risks higher for those with already low platelet counts.
Examples include abciximab, eptifibatide, and tirofiban. These drugs are key in some heart procedures but need careful watch on platelet counts because of thrombocytopenia risks.
Thiazide Diuretics
Thiazide diuretics are used to treat high blood pressure and swelling. Some studies link thiazides to thrombocytopenia, though the exact reason is unclear. It’s thought they might trigger an immune response that destroys platelets.
For those with thrombocytopenia, using thiazide diuretics should be thoughtfully considered. It might be better to use other blood pressure medicines to avoid making low platelet counts worse.
Other Cardiac Medications
Other heart medicines, like some antiarrhythmics and vasodilators, can also be risky for those with thrombocytopenia. For example, some antiarrhythmics can affect how platelets work or their numbers, which can increase bleeding risks.
Healthcare providers should weigh the benefits and risks of heart medicines in patients with thrombocytopenia. It’s important to regularly check platelet counts and adjust medicines as needed to manage these patients well.
Monitoring and Managing Medication-Related Thrombocytopenia
Managing medication-related thrombocytopenia needs a detailed plan. This includes regular checks and quick action when warning signs appear. A proactive approach helps lower the risks of low platelet counts.
Regular Blood Count Testing
Testing blood counts often is key in managing thrombocytopenia. Patients should get regular complete blood counts (CBCs) to track their platelets. The Mary Bird Perkins Cancer Center suggests CBCs for early thrombocytopenia detection and timely action.
Table: Recommended Frequency for CBC Testing
| Patient Condition | CBC Frequency |
| Stable patients on medication | Every 4-6 weeks |
| Patients with a history of thrombocytopenia | Every 2-4 weeks |
| Patients on chemotherapy | As directed by the oncologist, typically every 1-3 weeks |
Recognizing Warning Signs
Spotting thrombocytopenia warning signs early is critical. Patients should watch for signs like too much bruising, small red spots on the skin, and bleeding that won’t stop. Healthcare experts say, “Spotting these signs early can greatly help in managing thrombocytopenia.”
“Patients should be educated on the signs of bleeding and the importance of seeking immediate medical attention if they experience severe symptoms.”
When to Contact Healthcare Providers
Knowing when to call healthcare providers is vital. Patients should contact their team for severe bruising, long-lasting nosebleeds, bleeding gums, or heavy periods. Quick action can prevent serious issues and adjust treatment plans as needed.
Understanding the need for regular checks, recognizing warning signs, and knowing when to seek help is key. This way, patients can manage medication-related thrombocytopenia well. We aim to provide thorough care and support to our patients to reduce the risks of this condition.
Conclusion
Understanding the risks of certain medications helps patients avoid bleeding problems. Platelets are key in blood clotting. Low platelet counts can cause serious health issues.
Knowing the symptoms of low platelets is vital for getting medical help quickly. Medical News Today says stopping the drug causing thrombocytopenia can help patients recover. We work with healthcare providers to reduce bleeding risks and improve outcomes.
We avoid certain medications, check platelet counts, and watch for warning signs. Knowing how platelets work shows their importance in preventing bleeding. Being aware of drugs that affect platelet counts helps patients protect their health.
FAQ
What is thrombocytopenia?
Thrombocytopenia is when you have too few platelets in your blood. This can make it easier to bleed.
What is a normal platelet count?
A normal platelet count is between 150,000 and 450,000 per microliter of blood.
How do NSAIDs affect platelet function?
NSAIDs, like ibuprofen and aspirin, can mess with how platelets work. This can make bleeding more likely for people with thrombocytopenia.
Why should aspirin be avoided in patients with low platelet counts?
Aspirin stops platelets from sticking together. This is a big problem for people with low platelet counts.
What antiepileptic medications are associated with thrombocytopenia?
Some antiepileptic drugs, like carbamazepine and phenytoin, can cause thrombocytopenia.
How do chemotherapeutic agents affect platelet counts?
Chemotherapy drugs, such as methotrexate and cisplatin, can slow down bone marrow. This can lead to low platelet counts.
What over-the-counter medications should be avoided with thrombocytopenia?
Avoid common OTC pain relievers like ibuprofen and aspirin. Also, steer clear of herbal supplements that can affect platelets.
Why is it essential to read labels carefully?
Reading labels helps you avoid hidden ingredients that can harm your platelets.
What cardiovascular medications require caution in patients with thrombocytopenia?
Be careful with medications like glycoprotein IIb/IIIa inhibitors and thiazide diuretics. They can be risky for people with thrombocytopenia.
How often should platelet counts be monitored?
It’s important to get regular blood tests to keep an eye on your platelet count.
What are the warning signs of thrombocytopenia?
Watch out for signs like bruising, petechiae, and bleeding that doesn’t stop.
When should healthcare providers be contacted?
If you notice any unusual bleeding or bruising, call your doctor right away.
References
Mary Bird Perkins Cancer Center. (2022). Thrombocytopenic precautions. https://marybird.org/wp-content/uploads/2022/06/2022_THROMBOCYTOPENIC_MBPCC.pdf
Medical News Today. (2024, September 25). Drug-induced thrombocytopenia: Causes and more. https://www.medicalnewstoday.com/articles/drug-induced-thrombocytopenia
StatPearls. (2023, July 3). Thrombocytopenia. https://www.ncbi.nlm.nih.gov/books/NBK542208/









