Menopause brings many changes, like hot flashes and mood swings. But some women also face persistent pelvic pain. Postmenopausal ovary pain affects about 15% of women during these times, making daily life tough.
Feeling ovary pain after menopause can be scary and mess up your day. At Liv Hospital, we focus on caring for your gynecologic health. We use proven methods and work with a team to find and treat the cause of menopause ovary discomfort. Find relief for postmenopausal ovary pain. This guide reveals 5 ultimate fixes and powerful strategies to manage discomfort today.
Key Takeaways
- Postmenopausal ovary pain is a common issue affecting approximately 15% of women.
- It can significantly impact daily life and overall well-being.
- Liv Hospital offers comprehensive gynecologic care for managing postmenopausal ovary pain.
- Effective relief strategies are available to alleviate symptoms.
- Proper diagnosis is key to treating the underlying causes of ovary pain after menopause.
Understanding Postmenopausal Ovary Pain
It’s important to understand ovarian pain after menopause to manage it well. This pain affects many women, causing discomfort and worry. We’ll look into how common it is, its effects, and what it means for women’s health.
Prevalence and Impact on Women’s Health
About 15% of women experience postmenopausal ovary pain. This pain can feel like cramps, pressure, or a dull ache in the lower abdomen or pelvis. It can really affect a woman’s life, making everyday tasks harder.
Knowing how common this pain is shows we need to talk about it more. We should look at what causes it to find ways to help.
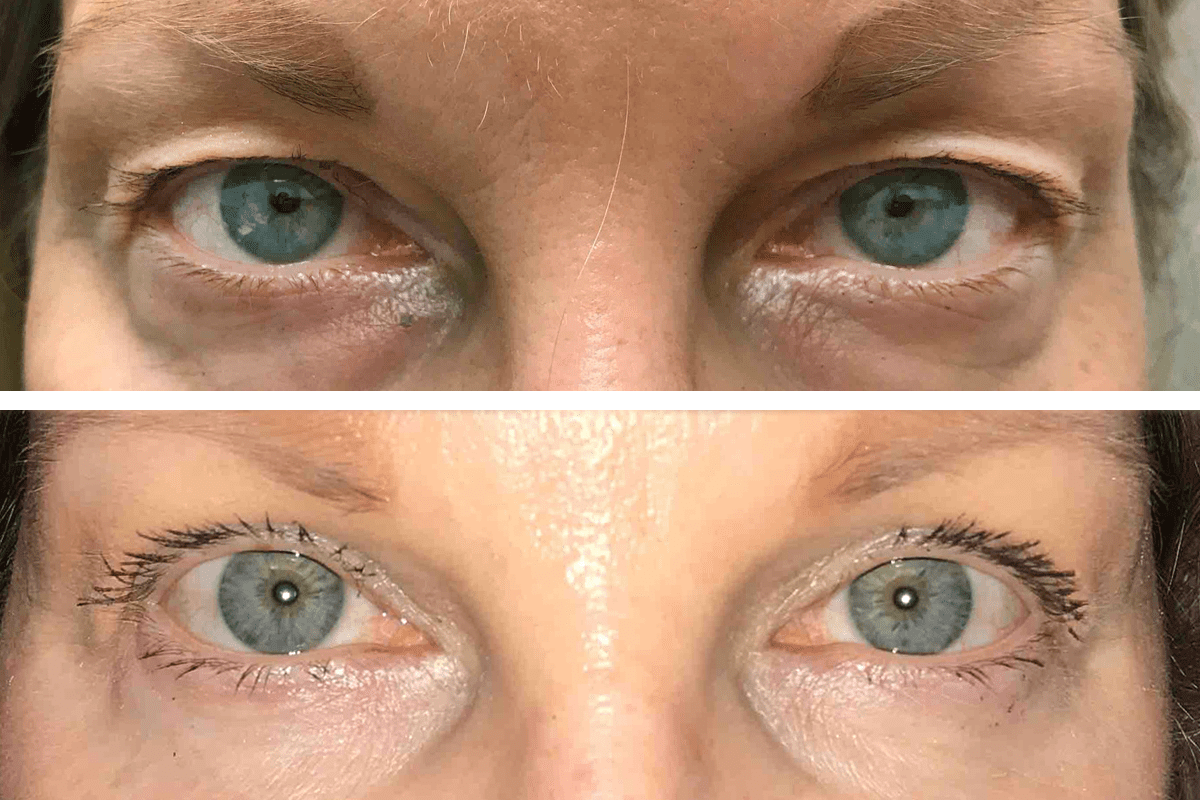
Normal vs. Abnormal Pain After Menopause
Telling normal pain from abnormal pain is key. Some discomfort is okay during menopause, but not constant or severe pain.
Abnormal pain is sharp, stabbing, or lasts a long time. It can really disrupt your life. Finding out why it happens is important to help manage it.
Common Causes of Ovarian Pain After Menopause
Ovarian pain after menopause can come from many sources. We’ll look at these in this section. Menopause ends a woman’s childbearing years, but health issues can cause pain in the ovaries.
Ovarian Cysts and Their Prevalence
Ovarian cysts are fluid-filled sacs in the ovaries. Women can get them even after menopause, causing pain. These cysts are common and can be seen on ultrasound.
Prevalence: Many postmenopausal women have ovarian cysts. They are often found during pelvic exams or imaging for other reasons.
Uterine Fibroids and Related Pain
Uterine fibroids are noncancerous growths in the uterus. They’re more common before menopause but can persist or cause symptoms afterward. This includes pain that might feel like it’s coming from the ovaries.
Symptoms: Women with fibroids may feel pelvic pressure, heavy bleeding (less common after menopause), and pain. These symptoms can be treated.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infection of the reproductive organs. It’s less common after menopause but can happen, mainly in women with certain risk factors. PID can cause a lot of pain and needs quick medical care.
Risk Factors: Postmenopausal women with a history of PID, those with certain sexually transmitted infections, or those who have procedures that might introduce bacteria are at higher risk.
Ovarian Neoplasms and Cancer Risk
Ovarian neoplasms, including both benign and malignant tumors, can cause ovarian pain after menopause. While ovarian cancer is rare, it’s serious and needs early detection and treatment.
Symptoms and Detection: Ovarian neoplasms might not show symptoms early, but as they grow, they can cause pain, bloating, and discomfort. Regular check-ups and knowing the symptoms are key for early detection.
Secondary Causes of Postmenopausal Ovary Pain
Secondary factors like ovarian torsion and pelvic adhesions can cause ovary pain in postmenopausal women. These issues are hard to diagnose and treat. A detailed approach is needed to manage symptoms well.
Ovarian Torsion
Ovarian torsion is a serious issue where the ovary twists, cutting off blood supply. This can lead to severe, sharp pain after menopause. Quick medical help is key to avoid lasting damage.
Symptoms of Ovarian Torsion:
- Severe, sharp pain on one side of the abdomen
- Nausea and vomiting
- Fever
Pelvic Adhesions
Pelvic adhesions are bands of fibrous tissue between organs or the abdominal wall. They can cause pain and discomfort, often from past surgeries or infections.
Common causes of pelvic adhesions include:
- Previous pelvic surgery
- Endometriosis
- Pelvic inflammatory disease
Pelvic Congestion Syndrome
Pelvic congestion syndrome has varicose veins in the lower abdomen, causing a dull ache or heaviness. It’s often linked to ovarian vein incompetence.
Condition | Symptoms | Treatment Options |
Ovarian Torsion | Sharp pain, nausea, fever | Surgery to untwist or remove the ovary |
Pelvic Adhesions | Chronic pain, bowel obstruction | Surgical adhesiolysis |
Pelvic Congestion Syndrome | Dull ache, heaviness | Embolization, hormonal therapy |
Postmenopausal Endometriosis
Endometriosis can persist or develop after menopause, causing ovary pain. Hormone therapy may be needed to manage symptoms.
We’ve talked about secondary causes of postmenopausal ovary pain, like ovarian torsion, pelvic adhesions, pelvic congestion syndrome, and postmenopausal endometriosis. Knowing about these conditions is key for effective diagnosis and treatment.
Recognizing Symptoms and Pain Patterns
Postmenopausal ovary pain can show up in many ways. It’s important to know the symptoms well. This helps in diagnosing and managing the condition.
Types of Pain Sensations
Women with postmenopausal ovary pain might feel different kinds of pain. It can be a dull ache or sharp pains. The pain might be constant or episodic, changing in how bad it feels.
Some feel a deep, internal discomfort. Others might have sharp, stabbing pains. Knowing these differences helps doctors figure out the cause.
Location and Radiation Patterns
The pain’s location can give clues about its source. It usually hurts in the lower abdomen or pelvic area. But, it can also spread to the lower back, thighs, or hips.
It’s important to notice where the pain goes. For example, pain in the thighs might mean nerves are involved.
Associated Symptoms to Monitor
There are other symptoms to watch for too. These include abnormal vaginal bleeding, changes in bowel or urinary habits, or even fever or nausea. These can be signs of something more serious.
Keeping an eye on these symptoms is key. They can help doctors understand what’s causing the pain. For instance, fever and tenderness might point to an infection or inflammation.
By paying close attention to symptoms and pain patterns, doctors can find the right treatment. This is how we manage menopause and ovary pain well.
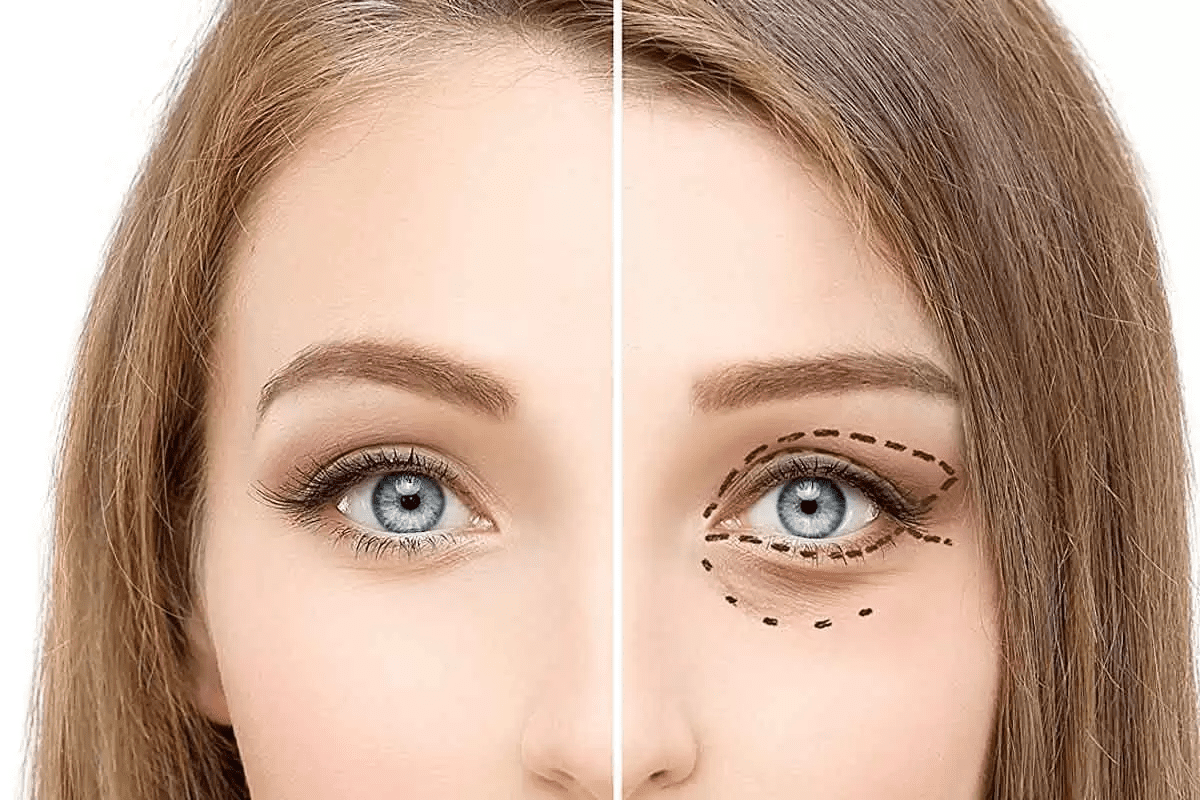
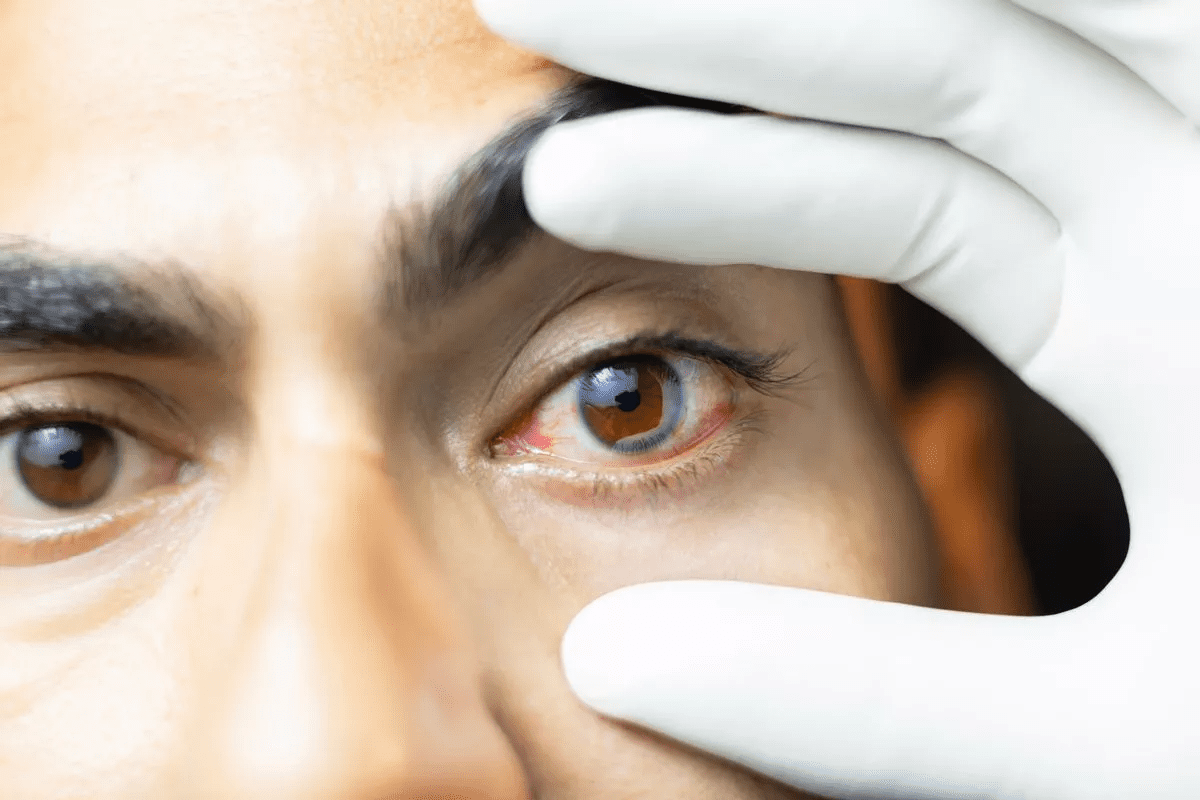
Diagnostic Approaches for Identifying Postmenopausal Ovary Pain
Understanding and addressing postmenopausal ovary pain requires a thorough diagnostic process. This process includes various tools and techniques to find the cause of pain after menopause.
Physical Examination Process
The first step is a detailed physical examination. We perform a pelvic exam to check the reproductive organs for any issues. This helps us find the source of pain and decide on further tests.
Imaging Studies and Their Benefits
Imaging studies are key in finding the cause of ovarian pain after menopause. We use ultrasound and MRI to see the ovaries and nearby areas. These tools help spot problems like cysts or fibroids that might be causing pain.
Laboratory Tests and Biomarkers
Laboratory tests are also vital. We do blood tests to look for signs of infection or inflammation. Biomarkers like CA-125 help check for ovarian cancer risk, but they’re not a sure sign.
Differential Diagnosis Considerations
When diagnosing postmenopausal ovary pain, we must consider many possible causes. We look at both gynecological and non-gynecological sources of pain. A detailed approach helps us find the real cause and plan the right treatment.
By using physical exams, imaging, lab tests, and careful diagnosis, we can accurately find the cause of postmenopausal ovary pain. Then, we can offer effective relief strategies.
Relief Strategy 1: Medical Management Options
Looking for relief from menopause ovary discomfort often starts with medical management. This approach offers various treatments to ease symptoms.
Over-the-Counter Pain Medications
OTC pain meds are often the first choice for ovarian pain after menopause. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can lessen pain and swelling. Acetaminophen is another option, though it doesn’t fight swelling, it helps with pain.
Prescription Medications for Specific Causes
If OTC meds don’t work, prescription meds might be needed. For example, if ovarian cysts cause pain, hormonal treatments can shrink cysts and ease pain. If pelvic inflammatory disease is suspected, antibiotics are used.
Hormone Therapy Considerations
Hormone therapy can help with postmenopausal ovary pain, mainly due to hormonal imbalances. But, it’s important to consider the risks, like blood clots or stroke. Consulting with a healthcare provider is key to decide if hormone therapy is right.
Monitoring Medication Effectiveness
It’s important to check how well any medication works for postmenopausal ovary pain. Keeping a pain diary can track pain levels and how meds affect them. Regular check-ups with a healthcare provider help adjust the treatment plan for better pain relief.
Relief Strategy 2: Physical Therapies and Exercises
Many women find relief from postmenopausal ovary pain through physical therapies and exercises. These methods can lessen discomfort, boost flexibility, and improve overall health.
Pelvic Floor Physical Therapy
Pelvic floor physical therapy targets the muscles and tissues around the pelvic area. It helps by easing tension in these muscles.
Benefits of Pelvic Floor Physical Therapy:
- Reduces pelvic pain and discomfort
- Improves bladder control
- Enhances overall pelvic health
Gentle Stretching Routines
Gentle stretching can ease tension and pain in the pelvic area. Simple moves like knee to chest stretches or pelvic tilts are helpful.
Example Stretching Routine:
- Lie on your back with knees bent and feet flat on the floor.
- Tilt your pelvis upwards and then back down again, repeating for 10 repetitions.
- Slowly bring one knee towards your chest, holding for 30 seconds before releasing.
Low-Impact Exercise Recommendations
Low-impact activities like walking, swimming, or yoga can boost circulation, reduce pain, and enhance health.
Exercise | Benefits |
Walking | Improves circulation, reduces pain |
Swimming | Low-impact, improves cardiovascular health |
Yoga | Enhances flexibility, reduces stress |
Building a Consistent Routine
Consistency is key in physical therapies and exercises. Start slow and gradually increase the intensity and duration of your routine.
“The key to managing postmenopausal ovary pain is finding a balance between activity and rest. By incorporating physical therapies and exercises into your daily routine, you can take control of your pain and improve your quality of life.”
Relief Strategy 3: Heat Therapy and Self-Care Techniques
Heat therapy and self-care are great for easing aching ovaries during menopause. They help relax muscles, lessen pain, and boost overall health.
Proper Application of Heat Therapy
Getting heat therapy right is key to its benefits. Use a warm heating pad or a hot water bottle in a towel to avoid skin contact. The temperature should be just right, not too hot. Heat for 15-20 minutes, then let your skin cool before applying again.
Tips for Effective Heat Therapy:
- Use a timer to avoid overheating
- Apply heat to the lower abdomen or lower back, where pain is most pronounced
- Combine heat therapy with relaxation techniques for enhanced relief
Relaxation Techniques for Pain Management
Relaxation techniques can greatly reduce ovarian pain in menopause. They lower stress and relax muscles. Deep breathing, progressive muscle relaxation, and meditation work well.
“Relaxation is not just a passive activity; it’s an active process that can help manage pain and improve quality of life.”
Sleep Positioning and Support
Right sleep positioning and support are key for managing ovary pain. Sleeping on your side with a pillow between your knees keeps your pelvis aligned and eases discomfort.
Sleep Enhancement Tips:
- Use a supportive mattress and pillows
- Avoid sleeping on your stomach, as it can cause pelvic misalignment
- Consider using a body pillow for additional support
Creating a Self-Care Plan
Creating a self-care plan is vital for managing menopause pain ovaries. It should include regular exercise, stress management, and healthy lifestyle choices.
Key Components of a Self-Care Plan:
- Regular physical activity tailored to your fitness level
- Stress reduction techniques such as yoga or tai chi
- A balanced diet rich in anti-inflammatory foods
By adding heat therapy and self-care to your daily routine, you can find relief from ovarian pain in menopause. Always talk to a healthcare provider before trying new pain management strategies.
Relief Strategy 4: Dietary and Lifestyle Modifications
Making changes in diet and lifestyle can help with postmenopausal ovary pain. Women can make choices that ease their symptoms and enhance their life quality.
Anti-Inflammatory Food Choices
An anti-inflammatory diet can help reduce inflammation and ease pain. Foods like salmon and sardines are good because they fight inflammation. Also, eating lots of fruits, vegetables, and whole grains can help.
Some foods that fight inflammation include:
- Berries rich in antioxidants
- Leafy greens like spinach and kale
- Nuts and seeds, specially those with omega-3s
- Olive oil, a healthy fat
Hydration and Its Impact on Pelvic Health
Drinking enough water is key for pelvic health and may lessen ovary pain. Water helps remove toxins and keeps tissues healthy. Aim for at least eight glasses of water a day.
Hydration Level | Impact on Pelvic Health |
Adequate Hydration | Reduces risk of pelvic inflammation and pain |
Inadequate Hydration | May increase risk of pelvic issues and discomfort |
Weight Management Considerations
Keeping a healthy weight is vital for managing ovary pain. Extra weight can strain the pelvic area, making pain worse. A balanced diet and regular exercise can help maintain a healthy weight.
Tips for Effective Weight Management:
- Eat a balanced diet rich in nutrients
- Engage in regular physical activity
- Monitor calorie intake
- Avoid fad diets; focus on sustainable lifestyle changes
Stress Reduction Strategies
Stress can make ovary pain worse, so managing stress is key. Techniques like meditation, yoga, and deep breathing can help lower stress.
By adopting these dietary and lifestyle changes, women can actively manage their postmenopausal ovary pain. This can improve their overall health and well-being.
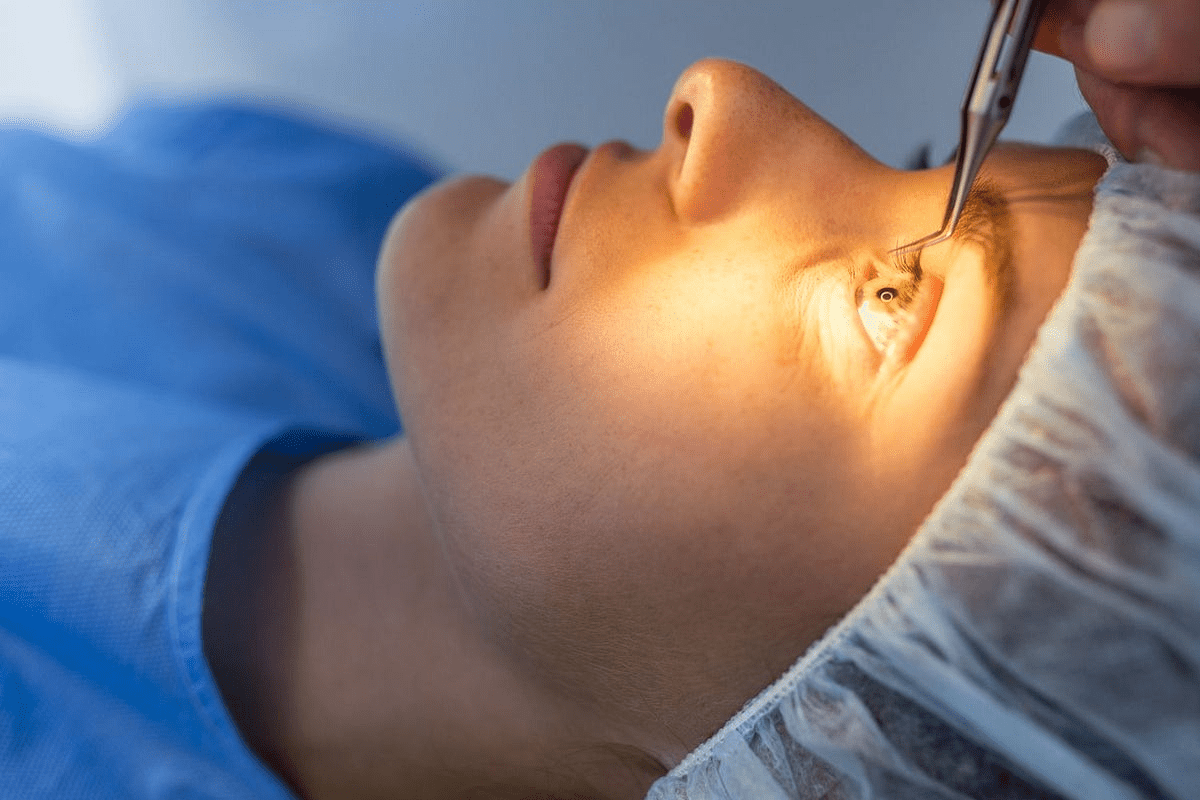
Relief Strategy 5: Surgical and Interventional Options
Women with severe postmenopausal ovary pain might find relief in surgery. Surgery is usually a last choice, but it’s needed when other treatments don’t work. It’s also used when certain conditions need surgery.
Minimally Invasive Procedures
Modern surgery has changed how we treat gynecological issues, including postmenopausal ovary pain. Laparoscopic surgery uses small cuts for a camera and tools. It helps find and fix problems like cysts or adhesions.
These surgeries cause less pain, shorter hospital stays, and faster healing than old methods. The choice depends on the pain cause and the patient’s health.
When Oophorectomy May Be Considered
In some cases, oophorectomy (ovary removal) might be an option for severe pain. It’s usually chosen when other treatments fail and pain greatly affects life quality.
Oophorectomy is considered for high cancer risk or when cysts or tumors cause pain. The surgery can be done laparoscopically or with a bigger cut, based on the case.
Recovery and Post-Surgical Care
Recovery time after surgery for ovary pain varies. Patients are told to avoid heavy lifting, bending, and hard work for weeks.
After surgery, care includes pain meds, check-ups, and advice on returning to normal activities. Following the surgeon’s advice is key for a smooth recovery.
Questions to Ask Your Surgeon
Talking to your surgeon before surgery is important. Ask these questions:
- What are the possible risks and problems with the procedure?
- What results can I expect, and how will it affect my condition?
- Are there other options instead of surgery, and why is it recommended for me?
- How long will I need to recover, and what care will I need after?
Understanding surgery options and asking the right questions helps women make informed choices. This can lead to significant pain relief after menopause.
Conclusion
Managing postmenopausal ovary pain needs a full approach. We’ve talked about five main ways to ease menopause ovary discomfort. These include medical treatments, physical therapies, heat therapy, self-care, diet changes, and surgery.
These methods can help women with ovarian pain after menopause feel better. It’s important for women to talk to their healthcare provider. They can find the best treatment for their situation.
If you’re dealing with ongoing or severe pain, see a doctor. They can check for any serious issues. By tackling postmenopausal ovary pain in a detailed way, women can lessen their discomfort. This improves their overall health and happiness.
FAQ
What is postmenopausal ovary pain?
Postmenopausal ovary pain is discomfort in the ovaries after menopause. It can be caused by cysts, fibroids, or other health issues.
Is ovary pain after menopause normal?
Some discomfort is normal during menopause. But, persistent or severe pain is not normal. You should see a doctor to find out why.
What are the common causes of ovarian pain after menopause?
Common causes include cysts, fibroids, and pelvic infections. Other causes are ovarian torsion, adhesions, and endometriosis.
How is postmenopausal ovary pain diagnosed?
Doctors use exams, imaging, and lab tests to diagnose. They check for biomarkers and hormonal imbalances.
What are the treatment options for managing postmenopausal ovary pain?
Treatments include medicines, physical therapy, and heat therapy. You can also try diet changes and lifestyle modifications. Sometimes, surgery is needed.
Can hormone therapy help with ovary pain after menopause?
Hormone therapy might help in some cases. But, it depends on the cause of pain. Always talk to a doctor first.
Are there any lifestyle changes that can help alleviate postmenopausal ovary pain?
Yes, eating anti-inflammatory foods and staying hydrated helps. Keeping a healthy weight and reducing stress also helps.
When should I seek medical attention for ovary pain after menopause?
See a doctor for persistent, severe, or worsening pain. Also, if you have fever, vaginal bleeding, or trouble urinating.
Can ovarian torsion occur after menopause?
Yes, ovarian torsion can happen after menopause. It’s rare but serious. Seek medical help for sudden, severe pain.
What are the benefits of pelvic floor physical therapy for postmenopausal ovary pain?
Physical therapy can reduce pain by improving muscle function. It also enhances pelvic health.
Are there any specific exercises that can help manage ovary pain after menopause?
Yes, gentle stretching and low-impact exercises like yoga help. Pelvic floor exercises also manage pain.
How can heat therapy help with postmenopausal ovary pain?
Heat therapy relaxes muscles and increases blood flow. Use a warm heating pad or a warm bath for 15-20 minutes.
What questions should I ask my surgeon if I’m considering surgery for ovary pain?
Ask about the procedure, risks, benefits, and recovery. Also, ask about post-surgical care to be well-informed.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10796202/