Menopause brings many changes, like hot flashes and mood swings. But some women also feel pelvic pain. This pain can range from ovarian discomfort to abdominal cramps. Are sore ovaries during menopause a sign of something serious? Get the essential facts on causes and when to be alarmed.
Menopause is tough for many, with physical and emotional symptoms. One surprise is pain in the ovarian area. Knowing why this happens is key to feeling better.
Key Takeaways
- Ovarian pain can be a symptom during the menopausal transition.
- Hormonal changes are a primary factor in pelvic discomfort.
- Understanding the causes is essential for proper diagnosis.
- Relief is possible with the right medical guidance.
- Women should seek a thorough evaluation for persistent pain.
Understanding Menopause and Ovarian Changes
It’s important to know about the changes in menopause to manage symptoms well. Menopause happens naturally in women, usually between 45 and 55 years old. The average age is 51. But, the transition phase, called perimenopause, can start years before.
The Menopausal Transition Timeline
Perimenopause can start between 30 and 50 years old. It can last 4 to 8 years, with some women feeling symptoms for up to 12 years. Women may see changes in their menstrual cycle and hot flashes during this time.
How Ovaries Change During Menopause
The ovaries change a lot during menopause. They make fewer hormones, like estrogen, which stops menstrual cycles. This drop in estrogen can lead to symptoms like changes in ovarian function and pain.
As women go through menopause, the drop in estrogen affects the ovaries and nearby areas. This can cause pain or discomfort. Knowing these changes helps manage ovarian pain during menopause.
Statistics on Menopause in the United States
In the U.S., the average age for menopause is 51. Many women go through menopause between 45 and 55. The length and symptoms of menopause vary a lot among women.
Understanding menopause and its changes helps women prepare and manage symptoms, like ovarian pain. It’s key to know that while menopause is natural, some symptoms might need medical help to check for other issues.
Why Sore Ovaries During Menopause Occur
The menopausal transition brings big changes in hormones, which can cause sore ovaries. Women going through this change may feel pain in their ovaries. It’s important to know why this happens to manage the pain better.
Hormonal Fluctuations and Pain
Hormonal changes are a big part of menopause. The levels of estrogen and other hormones change a lot. Estrogen decline is key because it affects the reproductive system’s health.
Hormonal changes make vaginal walls thinner and less elastic, causing discomfort. The drop in estrogen also weakens pelvic floor muscles, leading to pain.
The Role of Estrogen in Pain Modulation
Estrogen is important for managing pain. It has receptors in the nervous system that help control pain. When estrogen levels drop during menopause, pain perception can change.
Studies show estrogen keeps vaginal and pelvic tissues healthy. Without enough estrogen, these tissues can get inflamed and painful. Knowing this helps us tackle sore ovaries during menopause.
Neurological Aspects of Menopausal Pain
Menopausal pain involves complex interactions between hormones and the nervous system. Changes in estrogen levels can affect neurotransmitters and pain pathways. This can make women more sensitive to pain.
We’re discovering how these neurological changes cause pain during menopause. This knowledge is key to finding effective pain management strategies.
Common Symptoms Associated with Ovarian Pain
Ovarian pain during menopause can show up in many ways. Women might feel sharp pains or dull aches. These feelings can come and go or stay for a while.
Distinguishing Ovarian Pain from Other Pelvic Discomfort
It can be hard to tell if pain is from the ovaries or not. Ovarian pain often feels like it’s in the lower belly, pelvis, or even the lower back. Knowing where the pain comes from is key to getting the right treatment.
Women in perimenopause might feel sharp pains, twinges, or aches. These could be from irregular ovulation, cysts, or inflammation that’s sensitive to hormones. For some, this pain feels like menstrual cramps, even when they’re not having their period anymore.
Frequency and Duration of Pain Episodes
The timing and length of ovarian pain can differ a lot between women. Some might feel pain off and on, while others might have it all the time. Knowing how often and for how long the pain happens is important for managing it.
Women can feel pain in their ovaries during perimenopause or menopause, even when their ovaries aren’t working as much. The pain can feel sharp or dull, lasting from a few minutes to hours or even days.
Accompanying Symptoms to Monitor
Women might also notice other symptoms to watch out for. These include bloating, abdominal tenderness, and changes in how their bowels work. Sometimes, ovarian pain can also cause vaginal bleeding or discharge.
It’s important to keep track of these symptoms and tell a healthcare provider. This helps make sure there’s not something more serious going on that needs medical help.
Perimenopause vs. Menopause: Differences in Ovarian Pain
It’s important to know how ovarian pain changes from perimenopause to menopause. Perimenopause is a phase before menopause where the ovaries start to change.
Unique Aspects of Perimenopausal Ovarian Pain
Women in perimenopause might feel sharp pain due to irregular ovulation. They might also have twinges or aches from ovarian cysts or hormone-sensitive inflammation. This pain can be unpredictable and vary in intensity.
Key characteristics of perimenopausal ovarian pain include:
- Irregularity in frequency and severity
- Association with hormonal fluctuations
- Potential presence of ovarian cysts
Medical Expert, “The perimenopausal transition can be a time of significant hormonal variability. This leads to a range of symptoms, including ovarian pain.”
“The perimenopausal transition can be a time of significant hormonal variability, leading to a range of symptoms including ovarian pain.” – Medical Expert
How Pain Changes as You Progress Through Menopause
As women move from perimenopause to menopause, their ovarian pain changes. In menopause, the ovaries stop producing eggs, and hormone levels drop a lot.
The shift in pain characteristics may include:
- A decrease in the frequency and intensity of pain episodes
- Changes in the type of pain experienced (e.g., from sharp to dull)
- Potential cessation of ovarian pain due to reduced ovarian activity
Duration of Symptoms in Different Menopausal Stages
The time ovarian pain lasts can change a lot from perimenopause to menopause. In perimenopause, symptoms can last for years. In menopause, the pain may stop or become less frequent.
Menopausal Stage | Typical Duration of Ovarian Pain |
Perimenopause | Several years, with varying intensity |
Menopause | Generally decreases or ceases |
In conclusion, knowing the differences in ovarian pain between perimenopause and menopause helps women manage their symptoms better. It also helps them seek the right care when needed.
Medical Conditions That Can Cause Ovarian Pain During Menopause
Women going through menopause might feel ovarian pain due to various medical issues. While most pelvic pain during menopause is not serious, some cases need medical attention.
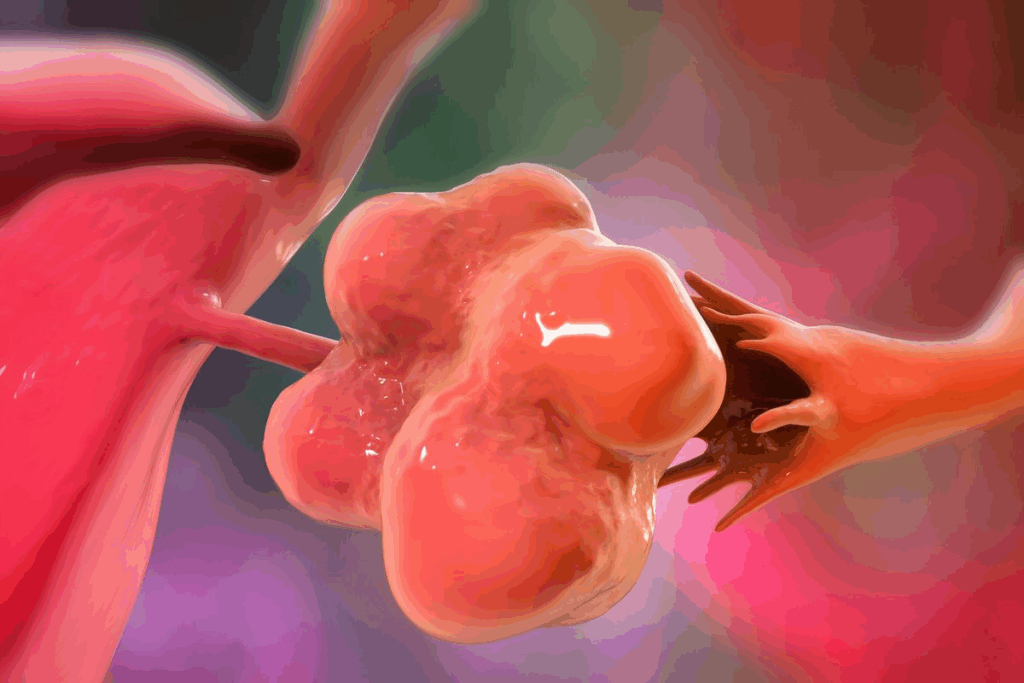
Ovarian Cysts in Postmenopausal Women
Ovarian cysts can happen in women after menopause, though it’s less common. Research shows that 2.5 to 14 percent of postmenopausal women might get these cysts. They can lead to pelvic pain and discomfort.
A study in the Journal of Ultrasound in Medicine found that most ovarian cysts in postmenopausal women are not cancerous. Yet, it’s important to watch them for any signs of cancer.
Characteristics | Benign Cysts | Potential Malignancy |
Size | Typically smaller | Often larger |
Growth Rate | Stable or slow-growing | Rapidly growing |
Symptoms | Mild or no symptoms | Severe pelvic pain, bloating |
Ovarian Cancer Risk Factors and Warning Signs
Ovarian cancer is more common in women over 50, with most cases in women over 63. Risk factors include family history, genetic mutations, and previous cancers.
“Early detection of ovarian cancer significantly improves survival rates. Women should be aware of the warning signs, including persistent pelvic pain, bloating, and difficulty eating.”
Warning signs of ovarian cancer include:
- Pelvic pain or pressure
- Bloating or swelling in the abdomen
- Difficulty eating or feeling full quickly
- Urinary urgency or frequency
Other Possible Causes of Pelvic Pain
Other conditions can also cause pelvic pain during menopause, such as:
- Endometriosis or adhesions
- Pelvic inflammatory disease
- Irritable bowel syndrome (IBS)
- Interstitial cystitis
Seeing a healthcare provider is key to figuring out the cause of pelvic pain and getting the right treatment.
When to See a Doctor About Menopausal Ovary Discomfort
Knowing when to see a doctor for ovarian pain during menopause is key to staying healthy. Menopause is a big change in a woman’s life. While some discomfort is normal, some symptoms need attention.
Red Flags That Shouldn’t Be Ignored
There are certain signs that mean you should see a doctor. These include:
- Severe or getting worse pain
- Bleeding after menopause
- Pain with other bad symptoms like fever or vomiting
- Unusual or bad-smelling vaginal discharge
If you notice any of these, you should talk to your healthcare provider. Early treatment can make a big difference.
What to Expect During Your Medical Evaluation
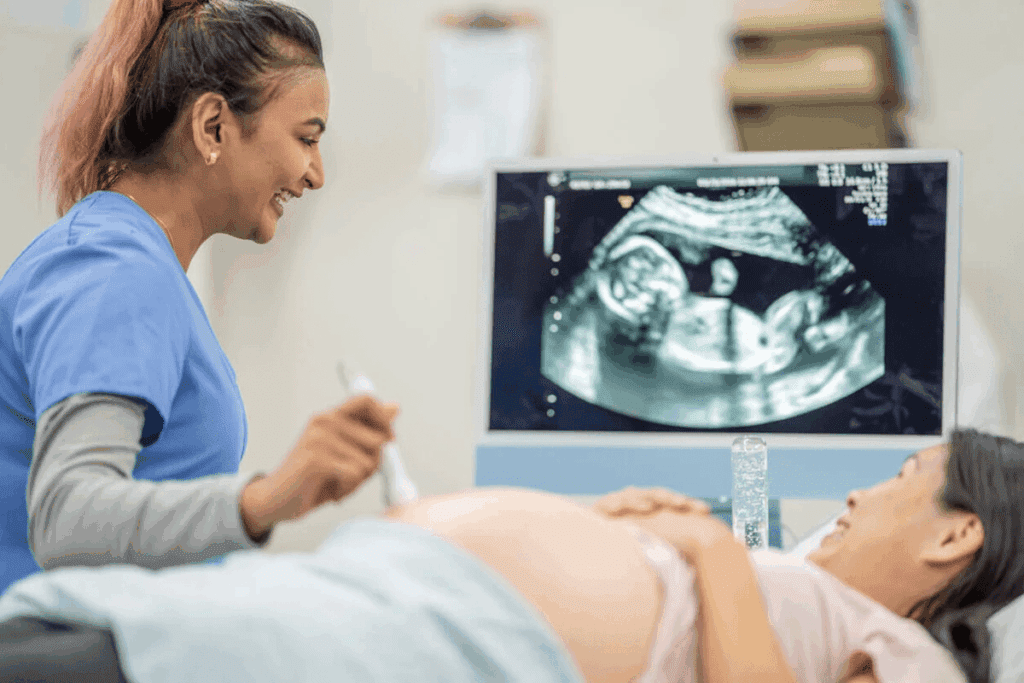
At your doctor’s visit, you’ll get a detailed check-up. This starts with a medical history and physical examination. Your doctor might do:
- External and internal pelvic exams
- Imaging tests like ultrasound or MRI
- Blood tests to check for infection or inflammation
Diagnostic Procedure | Purpose |
Pelvic Exam | To check for abnormalities in the reproductive organs |
Imaging Tests (Ultrasound, MRI) | To see the ovaries and nearby areas |
Blood Tests | To look for signs of infection or hormonal imbalances |
Questions to Ask Your Healthcare Provider
Being ready for your doctor’s visit helps you get the right care. Think about asking these questions:
- What could be causing my ovarian pain?
- Are there any more tests you suggest?
- What treatments are there for my condition?
- Are there lifestyle changes that can help my symptoms?
Understanding when to see a doctor and what to expect can help you manage your menopausal ovary discomfort.
Diagnostic Procedures for Ovarian Pain
Women going through menopause often feel ovarian pain. Finding out why this pain happens is key. Doctors use many steps to figure out the cause and find the right treatment.
Physical Examinations and Medical History
The first step is a physical examination and a medical history. Doctors check the pelvic area for any issues. They also look at the patient’s past health and any surgeries.
This helps doctors guess what might be causing the pain. Knowing the patient’s health history is also important. It helps doctors understand the whole picture of the patient’s health.
Imaging Tests and Laboratory Work
Imaging tests are very important for diagnosing ovarian pain. Tests like ultrasound, CT scans, and MRI help doctors see the ovaries and nearby areas. They can spot problems like cysts or tumors.
Laboratory tests are also used. Blood tests check for infections, hormonal issues, or other problems that might cause pain.
Ruling Out Serious Conditions
One main goal of testing is to rule out serious conditions that could be causing pain. This includes looking for cysts, endometriosis, or other serious issues. By finding the cause, doctors can treat the problem effectively.
Ovarian pain can be a sign of many things, some of which need quick medical help. Our detailed testing makes sure we find the cause and give the right care.
Treatment Options for Aching Ovaries During Menopause
Women going through menopause need to know about treatment options for ovarian pain. It’s important to find ways to ease discomfort and improve life quality during this time.
Medical Interventions and Hormone Therapy
Medical treatments are key in managing ovarian pain during menopause. Hormone replacement therapy (HRT) is a main approach. It aims to replace estrogen levels that drop and may cause pain.
Hormone Replacement Therapy (HRT) can help lessen menopausal symptoms, like ovarian pain. But, it’s important to talk to a doctor first. HRT might not be right for everyone.
Therapy Type | Description | Benefits |
Hormone Replacement Therapy (HRT) | Supplements estrogen levels | Reduces menopausal symptoms, including ovarian pain |
Pelvic Floor Physical Therapy | Targets pelvic floor muscles | Relieves pelvic pain, improves bladder control |
Pain Management Medications | Various medications for pain relief | Effective for managing acute and chronic pain |
Pain Management Strategies
Pain management is vital for treating aching ovaries during menopause. It includes different strategies, from medicines to lifestyle changes.
Medical Expert, a women’s health expert, says, “The key to effective pain management is a personalized approach that considers the individual’s overall health and specific needs.“
- Over-the-counter pain relievers
- Prescription pain medications for severe cases
- Lifestyle modifications, including diet and exercise
Alternative and Complementary Approaches
Along with medical treatments, alternative and complementary therapies can help with ovarian pain. These include:
“Acupuncture and other alternative therapies can provide significant relief for some women, making a great addition to traditional treatments.”Medical Expert, Integrative Medicine Specialist
- Acupuncture
- Herbal supplements
- Mind-body therapies like meditation and yoga
Exploring different treatment options and working with healthcare providers can help women manage ovarian pain during menopause effectively.
Lifestyle Changes to Reduce Ovary Pain in Menopause
Women going through menopause can find relief by making lifestyle changes. Menopause brings discomfort, including pain in the ovaries. By adopting certain habits, women can ease this pain and feel better overall.
Dietary Modifications That May Help
Diet is key in managing menopause symptoms, like ovary pain. Eating an anti-inflammatory diet with lots of fruits, veggies, and whole grains can help. Foods rich in omega-3s, like salmon and flaxseeds, are also good. Drinking plenty of water is important too.
Some foods can make ovary pain worse. Avoid foods high in sugar, salt, and unhealthy fats. Limiting caffeine and alcohol can also help, as they can make hot flashes and other symptoms worse.
Food Group | Beneficial Foods | Foods to Avoid |
Fruits and Vegetables | Berries, Leafy Greens | High-Sugar Fruits |
Proteins | Fatty Fish, Nuts, Seeds | Processed Meats |
Grains | Whole Grains | Refined Grains |
Exercise and Physical Activity Recommendations
Exercise is vital for reducing ovary pain in menopause. Low-impact exercises like walking, swimming, and yoga are best. These activities help with pain and improve health.
Exercise helps in many ways. It keeps weight healthy, reduces stress, and improves sleep. Aim for at least 30 minutes of moderate-intensity exercise most days.
Stress Management Techniques
Stress can make menopause symptoms worse, including ovary pain. Stress management techniques can help. Deep breathing, meditation, and mindfulness can reduce stress and promote relaxation.
Adding these techniques to daily life is easy. Start with a short meditation or deep breathing exercises during breaks. Consistency is key to feeling the benefits.
Conclusion: Managing Your Menopausal Journey
Managing ovarian pain during menopause needs a mix of strategies. Understanding the causes and symptoms is key. Exploring different treatments can help reduce pain and improve life quality.
Many women face unexplained cramps, aching ovaries, or stomach pain during or after menopause. You’re not alone in this. There are ways to get help.
Seeking the right care and making smart lifestyle choices can help. This includes changing your diet, exercising, and managing stress. Medical treatments and hormone therapy might also be needed.
We hope this guide helps women feel more confident during menopause. By tackling menopause comprehensively, women can ease ovarian pain. This ensures a smoother transition through this important life stage.
FAQ
Can ovaries hurt during menopause?
Yes, some women feel pain in their ovaries during menopause. This pain can be due to hormonal changes. But, it’s also important to think about other possible causes, like ovarian cysts or other health issues.
What are the common symptoms associated with ovarian pain during menopause?
Women may feel sharp or dull pain in their ovaries during menopause. The pain can happen often or last a long time. They might also feel bloated, crampy, or uncomfortable in their pelvic area.
How does perimenopause differ from menopause in terms of ovarian pain?
Perimenopause and menopause are different in how they affect ovarian pain. Hormonal changes in perimenopause can cause more pain. In menopause, pain might lessen as hormone levels stabilize.
What are the risk factors and warning signs for ovarian cancer during menopause?
Risk factors for ovarian cancer include family history, genetic mutations, and age. Signs to watch for are persistent pelvic pain, bloating, swelling, or trouble eating. If you notice these, see your doctor right away.
What diagnostic procedures are used to determine the cause of ovarian pain during menopause?
Doctors use physical exams, medical history, and tests like ultrasound or MRI to find the cause. They also do lab work. These steps help find serious issues and figure out why you’re in pain.
What treatment options are available for managing aching ovaries during menopause?
Treatments include hormone therapy, pain relief, and alternative methods like acupuncture. Changing your diet, exercising, and managing stress can also help. These steps can ease your symptoms.
When should I seek medical attention for ovarian pain during menopause?
See a doctor if your pain is severe, doesn’t go away, or gets worse. Also, if you have heavy bleeding, fever, or swelling, get help fast. It’s key to talk to your doctor if you’re unsure or worried about your pain.
Can lifestyle changes help reduce ovary pain during menopause?
Yes, making lifestyle changes can help with ovary pain during menopause. Eating right, exercising, and managing stress can help. Techniques like meditation or yoga can also improve your well-being.
Is ovarian pain during perimenopause a sign of an underlying medical condition?
Pain in ovaries during perimenopause might be due to hormone changes. But, it’s also important to think about other reasons, like cysts or health issues. If your pain is constant or severe, see your doctor to check for other problems.
How can I manage my menopausal journey with ovarian pain?
Managing ovarian pain in menopause needs a few steps. Understand the causes, know the symptoms, and try different treatments. Working with your doctor and making healthy choices can help reduce your symptoms and improve your life.
References
National Center for Biotechnology Information. Ovarian Pain During Menopause: Causes and Management. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507826/






