Menopause brings many changes, like hot flashes and mood swings. But some women also feel pelvic pain. About 15 percent of women deal with ovary pain during or after menopause. Struggling with ovarian discomfort after menopause? Discover 5 surprising causes and the best, simple strategies for ultimate relief.
It’s important to know why postmenopausal ovary pain happens. At Liv Hospital, a team of experts works together to help women with this issue. They aim to find the cause and manage the pain effectively.
Key Takeaways
- Ovary pain after menopause affects a significant percentage of women.
- Postmenopausal ovary pain can be caused by various underlying conditions.
- Early diagnosis is key for effective management.
- Liv Hospital offers complete care for women with ovarian discomfort.
- A team of experts ensures the best results.
The Reality of Ovarian Discomfort After Menopause
Women going through menopause might feel discomfort in their ovaries. This symptom needs attention and understanding. Menopause is a natural process, but it can cause pain in the ovarian area.
Prevalence and Statistics
Studies show that 18 percent of post-menopausal women get ovarian cysts in 15 years. This shows how common ovarian problems are after menopause.
It’s important to know about pelvic pain during menopause. This pain is in the lower belly, pelvis, or reproductive organs. Hormonal changes and ovarian cysts can cause this pain.
Normal Ovarian Changes During Menopause
Menopause brings big changes to the ovaries. Estrogen levels drop, and the ovaries stop making eggs. They also get smaller. But, some women might get ovarian cysts, leading to pain.
It’s key to know the difference between normal changes and problems. While some changes are expected, pain is not always normal during menopause.
The presence of ovarian pain after menopause should prompt a thorough evaluation to rule out underlying pathology.
- Ovarian cysts are a common issue post-menopause.
- Hormonal changes contribute to menopausal pelvic pain.
- Understanding normal ovarian changes can help in identifying possible issues.
Common Causes of Postmenopausal Ovary Pain
After menopause, women might feel pain in their ovaries. This pain can come from many reasons. A big one is the drop in estrogen levels. This change can make the pelvic area uncomfortable.
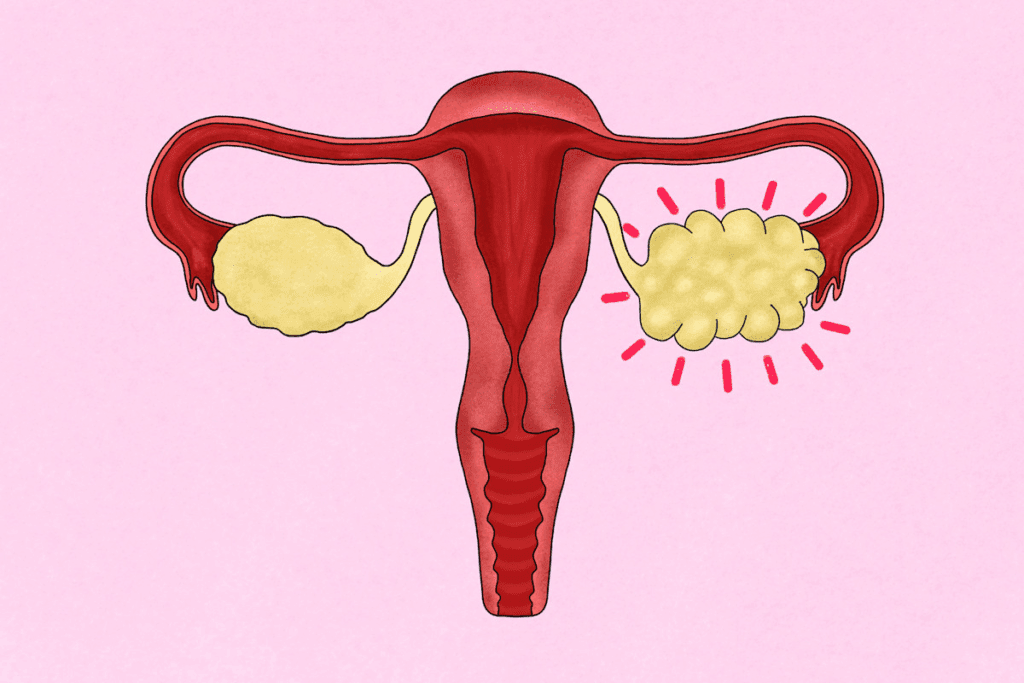
Ovarian Cysts
Ovarian cysts are fluid-filled sacs on the ovaries. They can happen before or after menopause. Simple cysts are usually not harmful, but complex cysts might need more checking.
- Simple cysts: usually harmless and might go away by themselves.
- Complex cysts: could have solid parts or thick walls, which might mean a bigger problem.
Ovarian Torsion
Ovarian torsion is when the ovary twists, cutting off blood. It’s rare but very serious. Symptoms include sharp pain on one side of the pelvis, nausea, and vomiting.
Quick diagnosis is key to avoid damage to the ovary.
Endometriosis Related to Hormone Replacement Therapy
Hormone replacement therapy (HRT) can sometimes make endometriosis worse. This condition has tissue like the uterine lining outside the uterus. It can cause pelvic pain, including pain in the ovaries.
- HRT can make endometrial implants grow.
- Symptoms include pelvic pain, heavy bleeding, or spotting.
Pelvic Congestion Syndrome
Pelvic congestion syndrome has varicose veins in the pelvic area, leading to chronic pain. It’s often linked to having given birth multiple times. It can also start or get worse after menopause.
Symptoms include dull, aching pain in the pelvic area. This pain gets worse after standing for a long time.
Distinguishing Left vs. Right Ovary Pain
It’s important for women after menopause to know the difference between left and right ovary pain. Where the pain is can help figure out what’s causing it.
Left-Sided Ovarian Pain
Left-sided pain can be due to certain conditions. Pelvic congestion syndrome often causes pain on the left side. This is because of varicose veins in the lower abdomen, leading to a dull ache or feeling of heaviness.
Other reasons for left-sided pain include:
- Ovarian cysts
- Endometriosis
- Adhesions from previous surgeries
Right-Sided Ovarian Pain
Right-sided pain can sometimes be mistaken for other issues, like appendicitis. But, it can also be due to ovarian torsion or a ruptured cyst, causing sharp, severe pain.
Right-sided pain can also be linked to:
- Ovarian pathology
- Gastrointestinal issues
- Urinary tract problems
Bilateral Ovarian Pain
Bilateral pain, or pain on both sides, is less common but can happen. It might be due to leftover ovarian tissue or other pelvic issues.
When you feel pain on both sides, consider:
- Hormonal influences
- Pelvic floor dysfunction
- Systemic conditions affecting the pelvic area
In conclusion, knowing the difference between left and right ovary pain is key for the right diagnosis and treatment. Always talk to a healthcare provider to find out why you’re in pain and what to do about it.
Ovarian Cancer Risk After Menopause
Menopause brings big changes in women’s health, including a higher risk of ovarian cancer. As we get older, the chances of getting ovarian cancer grow. It’s key for women after menopause to know their risk.
Age-Related Risk Factors
Ovarian cancer risk jumps up after 50, with most cases in women over 63. This age factor is a big deal for checking ovarian health.
Key age-related statistics include:
- Most ovarian cancer cases are diagnosed in women over 60.
- The risk keeps going up with age.
Knowing these facts helps women and doctors make better health choices.
Warning Signs vs. Normal Discomfort
Telling normal postmenopausal pain from possible cancer signs is key. Some pain might be okay, but serious or lasting pain needs a doctor.
“The challenge lies in differentiating between common postmenopausal symptoms and signs that may indicate a more serious condition like ovarian cancer.”
If you’re postmenopausal and have a painful cyst, there’s a 3 in 1,000 chance it’s cancer. Knowing the signs can help catch cancer early.
Screening Recommendations
There’s no routine test for ovarian cancer for all women. But, high-risk women might get special screening.
Screening considerations include:
- Talking about family history and genetic risks with your doctor.
- Knowing the good and bad of screening tests.
Women with a big family history or genetic risks might need more screening and prevention.
Postmenopausal women should keep up with their ovarian health and talk to their doctor about worries. Knowing the risks and watching for symptoms helps women stay healthy.
Diagnosing the Cause of Ovarian Pain
When you experience pain in your ovaries after menopause, finding the cause is key. We start by looking at your medical history. This helps us understand what might be causing your discomfort.
Physical Examination
A physical exam is the first step in figuring out ovarian pain. We do both outside and inside pelvic exams. This helps us find any problems or tenderness.
Imaging Tests
Imaging tests are needed to look deeper into the pain. We might use:
- Ultrasound to see the ovaries and nearby areas
- MRI for detailed pictures of the pelvic area
These tests help us see how the ovaries are doing and find any issues.
Blood Tests and Biomarkers
Blood tests are also important. We check for:
- Signs of infection or inflammation
- Tumor markers like CA-125 to check for ovarian cancer risk
Diagnostic Test | Purpose |
Physical Examination | Assess abnormalities or tenderness |
Ultrasound | Visualize ovaries and surrounding structures |
MRI | Provide detailed images of the pelvic area |
Blood Tests | Check for infection, inflammation, or tumor markers |
By looking at all these test results, we can find out what’s causing your pain. Then, we can create a plan to help you feel better.
Non-Ovarian Causes That Mimic Ovarian Pain
When you feel pain in your ovaries after menopause, it might not be from the ovaries. Other issues can cause similar pain, making it hard to figure out what’s wrong.
Gastrointestinal Issues
Menopause can make stomach problems worse. This includes bloating, constipation, and irritable bowel syndrome (IBS). These problems can feel like ovarian pain.
- Bloating and gas can cause sharp pains that feel like they’re coming from the ovaries.
- Constipation can lead to cramping that radiates to the pelvic area.
- IBS can cause a variety of symptoms that may mimic ovarian pain.
Urinary Tract Problems
Urinary tract infections (UTIs) and other issues can cause pain that’s sometimes blamed on the ovaries. Lower estrogen levels during menopause can make UTIs more common.
Condition | Symptoms |
UTI | Burning during urination, frequent urination, pelvic pain |
Overactive Bladder | Urinary urgency, frequency, nocturia |
Musculoskeletal Pain
Musculoskeletal issues, like pelvic floor dysfunction or lower back pain, can be mistaken for ovarian pain. The pelvic floor muscles support the uterus, ovaries, and bladder. When these muscles don’t work right, it can hurt a lot.
It’s important to know about these non-ovarian causes of pain. This helps doctors find the right treatment for women in pain after menopause.
Treatment Options for Postmenopausal Ovarian Discomfort
There are many ways to treat ovarian pain after menopause. Each woman’s needs are different. A good treatment plan should match the woman’s symptoms and health.
Medication Approaches
For many, starting with medication is the first step. Pain relief medications like NSAIDs are often used first. Sometimes, hormone therapy is suggested to help with hormonal changes.
Medication Type | Use | Benefits |
NSAIDs | Pain relief | Effective for mild to moderate pain |
Hormone Therapy | Symptom alleviation | Addresses hormonal imbalances |
Surgical Interventions
When pain is due to cysts or tumors, surgical intervention might be needed. The surgery type depends on the problem found.
“Surgical treatment for ovarian pathology is often effective in resolving pain and improving quality of life for postmenopausal women.”
— Expert Opinion
Hormone Replacement Considerations
Hormone Replacement Therapy (HRT) is key for managing symptoms. It helps by adding hormones that the body is missing.
Talking to a healthcare provider about HRT is important. They can help decide if it’s right for you.
Managing Ovarian Pain at Home
Ovarian pain after menopause can be a worry, but there are ways to feel better at home. Simple daily habits can make a big difference in how much pain you feel. Making smart choices can help ease your discomfort.
Pain Relief Strategies
It’s important to find ways to manage pain at home. Over-the-counter medicines like ibuprofen or acetaminophen can help with mild to moderate pain. Always talk to a doctor before trying new medicines.
Heat Therapy: A heating pad on your lower abdomen can relax muscles and improve blood flow. This can help reduce pain. Remember to use a towel between your skin and the heating pad to avoid burns.
- Use a heating pad on a low setting for 15-20 minutes at a time.
- Take breaks to avoid overheating.
- Consider using a warm bath as an alternative.
Lifestyle Modifications
Changing your lifestyle can help manage ovarian pain. Doing low-impact exercise like walking or yoga can help. It improves circulation and releases endorphins, which are natural painkillers.
Lifestyle Change | Benefit |
Regular Exercise | Improves circulation and releases endorphins |
Anti-inflammatory Diet | Reduces inflammation and promotes overall health |
Stress Reduction Techniques | Lowers stress levels, which can exacerbate pain |
Staying Hydrated | Helps maintain bodily functions and overall well-being |
Eating an anti-inflammatory diet can also help. It should include lots of fruits, vegetables, and omega-3 fatty acids. Stress reduction techniques like meditation or deep breathing can also help by lowering stress.
Complementary Therapies
Complementary therapies can offer extra relief when used with regular treatments. Acupuncture and massage therapy can help manage chronic pain. They promote relaxation and improve energy flow.
It’s important to talk to a healthcare provider about these options. They can make sure they’re safe and right for you.
Psychological Impact and Coping Strategies
It’s important to understand how ovarian pain after menopause affects women’s minds. This pain can impact not just their bodies but also their mental health.
Anxiety About Cancer Risk
Women often worry about ovarian cancer when they feel pain. Feeling anxious about cancer is normal because age increases the risk. But, it’s key to tell the difference between normal pain and serious symptoms.
Talking to a healthcare provider can help. They can give advice based on your risk and symptoms. Knowing your risk and getting early detection can lessen anxiety.
Dealing with Chronic Pain
Living with chronic ovarian pain can be tough. Finding ways to cope is important. This includes pain relief, lifestyle changes, and other therapies.
- Relaxation techniques like deep breathing or meditation can help with stress and pain.
- Regular exercise, as suggested by a doctor, can boost well-being and lessen pain.
- Getting support from loved ones or groups can offer emotional help and practical tips.
Support Resources
Having the right support can greatly help with ovarian pain’s mental effects. This includes doctors, support groups, and educational resources.
Support groups, online or in-person, can provide a sense of community. Sharing experiences and advice with others facing similar issues is very helpful.
Dealing with ovarian pain after menopause is complex. By tackling both physical and mental aspects, women can improve their lives.
Conclusion
Women who feel pain in their ovaries after menopause can find help. There are many ways to treat this pain. Knowing what causes it is the first step.
Ovarian pain can come from cysts, torsion, or pelvic congestion. It’s important to know if the pain is on the left or right side. This helps doctors figure out what’s wrong.
There are treatments for this pain. Women can talk to doctors about medicines, surgery, or hormone therapy. Each option is chosen based on the woman’s needs.
Women can also try to ease pain at home. Changes in lifestyle and using natural remedies can help a lot. Knowing about support groups and counseling can also help with the emotional side of pain.
By getting medical help and trying different treatments, women can feel better. They can live a happier life without the pain.
FAQ
What is postmenopausal ovary pain?
Postmenopausal ovary pain is discomfort or pain in the ovaries after menopause. It’s a concern and important to find the cause.
Is ovarian pain after menopause normal?
Some discomfort is normal during menopause. But, persistent or severe pain is not usual and needs a doctor’s check.
What are the common causes of ovarian pain after menopause?
Causes include ovarian cysts, torsion, and endometriosis from hormone therapy. Pelvic congestion syndrome and non-ovarian causes also play a role.
How is ovarian pain after menopause diagnosed?
Diagnosis includes a physical exam, ultrasound, and blood tests. We also look at your medical history and symptoms.
Can ovarian pain be a sign of ovarian cancer after menopause?
Ovarian pain can be from many conditions, including cancer. We talk about risk, signs, and screening with our patients.
What are the treatment options for postmenopausal ovarian discomfort?
Treatment varies based on the cause. It might include medication, surgery, or hormone therapy. We create a plan tailored to you.
How can I manage ovarian pain at home?
Home management includes pain relief, lifestyle changes, and therapies. We guide you on these methods to ease discomfort.
What is the psychological impact of ovarian pain after menopause?
Ovarian pain can affect your mind, causing anxiety and pain management issues. We offer support and strategies to cope.
Can hormone replacement therapy cause ovarian pain?
Hormone therapy can lead to endometriosis, causing pain. We discuss the risks and benefits with you.
Are there any lifestyle changes that can help alleviate ovarian pain?
Yes, lifestyle changes can help. We suggest maintaining a healthy weight, exercising, and managing stress.
When should I seek medical attention for ovarian pain after menopause?
Seek medical help for persistent, severe, or sudden pain. We aim to find the cause and treat it effectively.
References
https://my.clevelandclinic.org/health/symptoms/24726-ovary-pain








