Grade 4 thrombocytopenia is a serious condition where the platelet count drops below 25,000 per microliter of blood. This can lead to severe and life-threatening bleeding.
Understanding the thrombocytopenia grading system is key. It helps doctors figure out how severe the condition is and how to treat it. The CTCAE 5.0 grading system shows Grade 4 thrombocytopenia as a severe drop in platelet count. It usually needs quick medical help.
Exploring Grade 4 thrombocytopenia is important. We need to know its causes, symptoms, and treatments. This ensures the best care for patients.
Key Takeaways
- Grade 4 thrombocytopenia is defined by a platelet count below 25,000 per microliter.
- The CTCAE 5.0 grading system is used to determine the severity of thrombocytopenia.
- Grade 4 thrombocytopenia poses a significant risk of spontaneous and life-threatening bleeding.
- Understanding the grading system is key for proper management.
- Immediate medical attention is often needed for Grade 4 thrombocytopenia.
Understanding Platelets and Their Critical Role
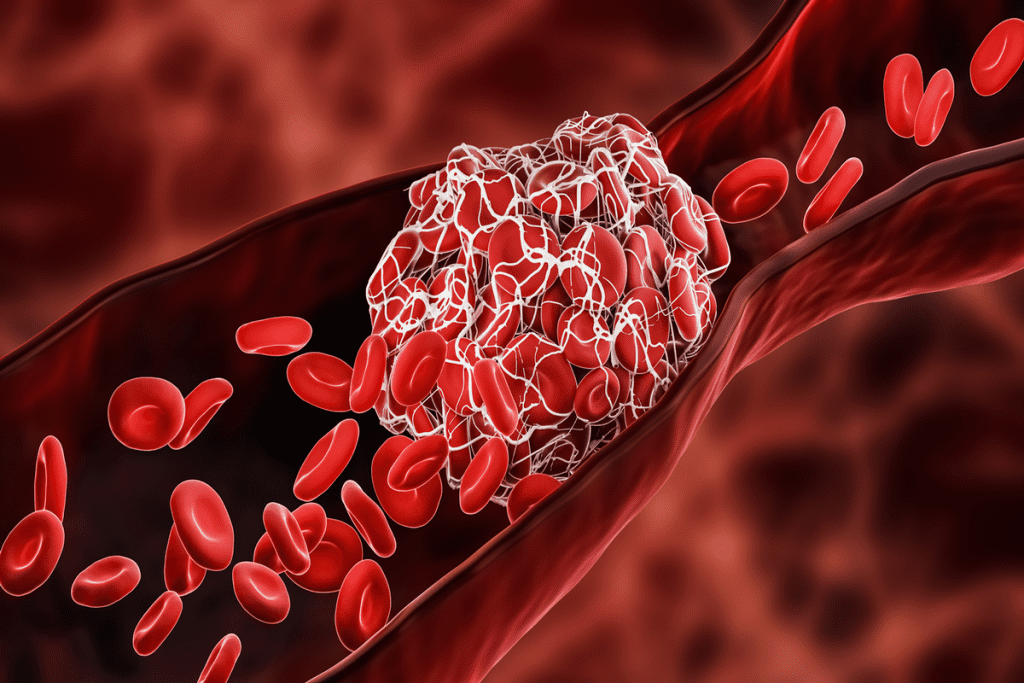
Platelets are small but vital blood cells that help prevent excessive bleeding. They play a key role in the blood clotting process. This process is essential for stopping bleeding when a blood vessel is injured.
Normal Platelet Function in Blood Clotting
Platelets are vital for stopping bleeding after an injury. When a blood vessel is damaged, platelets stick to the injury site. They then clump together to form a plug.
This plug is strengthened with fibrin, a protein that forms a clot. This clot stops the bleeding effectively.
Platelets are essential for keeping our blood vessels healthy. Without enough or functioning platelets, bleeding risks increase.
Healthy Platelet Count Ranges
A healthy platelet count is between 150,000 to 450,000 platelets per microliter of blood. Counts in this range usually mean normal blood clotting. We watch platelet counts closely in people at risk of low platelet counts.
Consequences of Platelet Deficiency
Thrombocytopenia, or low platelet count, increases the risk of bleeding. Low platelet counts make it hard for the body to form clots. This can lead to spontaneous or prolonged bleeding after injury.
Severe thrombocytopenia can be dangerous, highlighting the need to understand and manage it. Recognizing platelet deficiency signs and symptoms is key. Healthcare providers can then start the right treatment to reduce risks.
The CTCAE Grading System for Blood Disorders
The Common Terminology Criteria for Adverse Events (CTCAE) helps doctors and researchers understand the severity of side effects. This includes conditions like thrombocytopenia. It’s key for standardizing how side effects are assessed in cancer treatment and other medical procedures.
CTCAE Version 5.0 Overview
CTCAE Version 5.0 is the newest version of this system. It offers a detailed framework for assessing side effects. It includes criteria for conditions like thrombocytopenia, neutropenia, and anemia. The updates in Version 5.0 reflect the latest in clinical understanding, making the system more relevant and effective.
We use the CTCAE to have a common language for side effects. This helps healthcare providers communicate better and ensures side effects are reported and understood the same way.
Grading Criteria for Thrombocytopenia
According to CTCAE Version 5.0, Grade 4 thrombocytopenia is when the platelet count is less than 25,000/mm. This shows how severe thrombocytopenia is and helps doctors decide how to manage it.
The criteria for thrombocytopenia are:
- Grade 1: Platelet count less than the lower limit of normal (LLN) to 75,000/mm3
- Grade 2: Platelet count less than 75,000 to 50,000/mm3
- Grade 3: Platelet count less than 50,000 to 25,000/mm3
- Grade 4: Platelet count less than 25,000/mm3
Comparison with Neutropenia and Anemia Grading
The CTCAE also has grading for neutropenia and anemia. These conditions often happen with thrombocytopenia, mainly in patients getting chemotherapy or with bone marrow issues. Neutropenia grading is based on the absolute neutrophil count (ANC), with Grade 4 being less than 500 cells/mm. Anemia grading is based on hemoglobin levels, with Grade 4 being less than 6.5 g/dL.
Knowing the grading for these conditions helps doctors manage patients with multiple blood disorders. The CTCAE makes it easier to care for patients with complex needs by standardizing the assessment of these conditions.
Defining Grade4 Thrombocytopenia: The Critical Threshold
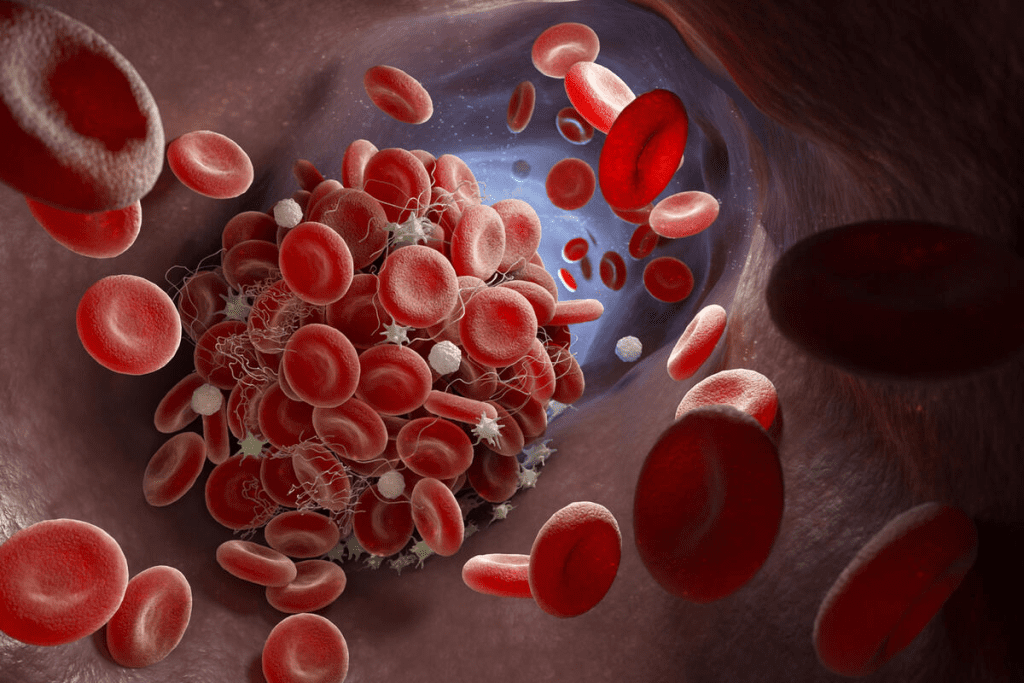
Grade 4 thrombocytopenia is a serious condition where platelet counts are very low. This makes it risky for spontaneous, dangerous bleeding. This risk is high when counts are below 10,000 per microliter.
Platelet Count Below 25,000/μL
A diagnosis of Grade 4 thrombocytopenia is made when platelet counts are under 25,000/μL. At this level, the body can’t form blood clots well. This increases the risk of bleeding.
Severe thrombocytopenia can happen for many reasons. These include chemotherapy, bone marrow problems, and some medicines. Knowing the cause is key to managing it well.
Clinical Significance of Severe Thrombocytopenia
The importance of Grade 4 thrombocytopenia is huge. At this level, patients face a high risk of spontaneous bleeding. This can be deadly if not treated quickly.
Key clinical implications include:
- Increased risk of internal bleeding
- Potential for hemorrhage
- Need for immediate medical intervention
Increased Risk of Spontaneous Bleeding
Grade 4 thrombocytopenia also means a higher chance of spontaneous bleeding. This can show up as petechiae, purpura, or severe bleeding.
Prompt medical attention is essential to manage this risk and prevent serious outcomes.
Pathophysiology of Severe Platelet Reduction
Grade 4 thrombocytopenia is a complex issue. It happens when the bone marrow can’t make enough platelets or when platelets get destroyed. Knowing how these problems work is key to treating them.
Mechanisms Leading to Grade 4 Thrombocytopenia
Several things can cause Grade 4 thrombocytopenia. These include:
- Bone Marrow Production Issues: Problems with the bone marrow, like aplastic anemia or cancer cells in the marrow.
- Peripheral Destruction of Platelets: Platelets being destroyed by the immune system, like in Immune Thrombocytopenia (ITP), or by mechanical means, like in Thrombotic Thrombocytopenic Purpura (TTP).
- Splenic Sequestration: The spleen holding too many platelets, which lowers their count in the blood.
Bone Marrow Production Issues
Bone marrow problems are a big reason for thrombocytopenia. The marrow makes megakaryocytes, which turn into platelets. If this process is blocked, it can lead to severe thrombocytopenia. Common reasons include:
- Chemotherapy and radiation therapy
- Bone marrow failure syndromes
- Cancer cells taking over the bone marrow
Peripheral Destruction of Platelets
Platelets being destroyed outside the bone marrow is another cause of Grade 4 thrombocytopenia. This can happen because of the immune system attacking platelets or due to mechanical damage in TTP or Hemolytic Uremic Syndrome (HUS).
Splenic Sequestration
The spleen can also play a role by holding onto too many platelets. This is often seen in hypersplenism, which can be caused by diseases like liver cirrhosis and lymphoproliferative disorders.
In summary, Grade 4 thrombocytopenia is a complex condition with many causes. Understanding its pathophysiology is vital for diagnosing and treating it.
Common Causes of Grade4 Thrombocytopenia
Grade 4 thrombocytopenia is a serious condition with very low platelet counts. Knowing what causes it is key to managing it well. Several factors can affect platelet production or destruction.
Chemotherapy-Induced Thrombocytopenia
Chemotherapy fights cancer by stopping cancer cells from growing. But, it can also harm the bone marrow, which makes platelets. This leads to thrombocytopenia in 8-24% of patients, depending on the treatment.
Key factors contributing to chemotherapy-induced thrombocytopenia include:
- The type and dose of chemotherapy agents used
- The duration of chemotherapy treatment
- Pre-existing bone marrow conditions
Immune Thrombocytopenia (ITP)
Immune thrombocytopenia (ITP) is when the immune system attacks platelets. This can cause severe thrombocytopenia, known as Grade 4, if platelet counts fall below 25,000/μL.
ITP can be triggered by various factors, including:
- Viral infections
- Autoimmune diseases
- Certain medications
Infection-Related Causes
Some infections can harm platelet production or increase their destruction. Severe infections, like sepsis, can lead to DIC. This makes thrombocytopenia worse.
Infections that can contribute to thrombocytopenia include:
- Viral infections like HIV, hepatitis C, and dengue fever
- Bacterial sepsis
- Parasitic infections such as malaria
Medication-Induced Thrombocytopenia
Some medicines can lower platelet counts by affecting bone marrow or increasing platelet destruction. Common offenders are heparin, antibiotics, and anticonvulsants.
Key considerations for medication-induced thrombocytopenia:
- Monitoring platelet counts in patients on potentially causative medications
- Discontinuing the offending drug if thrombocytopenia occurs
- Considering alternative treatments
What Are the Worst Days After a Stem Cell Transplant?
After a stem cell transplant, patients face a tough recovery. They risk getting thrombocytopenia, which means low platelet counts. This can cause serious bleeding. It’s key to know the timeline of thrombocytopenia, the nadir period, and how to manage blood crashes.
Thrombocytopenia Timeline Post-Transplant
The time when platelet counts drop after a transplant varies. Usually, counts start falling soon after, hitting their lowest 7-14 days later. We watch patients closely during this time to avoid and handle any issues.
Nadir Period and Recovery Phases
The nadir period is when blood counts are at their lowest. It’s a time we must watch closely. After this, patients start to get better, with counts slowly rising. This recovery can take weeks to months.
Important parts of recovery include:
- Platelet counts start to go up
- Supportive care gets better
- Looking out for bleeding or infection signs
Managing Blood Count Crashes
Dealing with blood count crashes needs a mix of care. This includes platelet transfusions and growth factor support. Sometimes, patients need to stay in the hospital to handle severe thrombocytopenia and avoid bleeding.
Good management includes:
- Platelet transfusions to stop bleeding
- Growth factor support to help blood cells grow
- Keeping a close eye on blood counts and health
Concurrent Neutropenia Concerns
Neutropenia, or low neutrophil counts, often happens with thrombocytopenia. This raises the risk of infections. It’s vital to manage both conditions together for patient safety. We must watch for infection signs and act quickly if needed.
Clinical Manifestations and Warning Signs
It’s important to know the signs of Grade 4 thrombocytopenia to get help quickly. This condition shows its severity through different warning signs.
Petechiae and Purpura
Petechiae are small spots on the skin, and purpura are larger bruises. They happen when blood vessels break. Petechiae often show up on the legs, and purpura can appear anywhere.
Spontaneous Bruising and Ecchymoses
Seeing bruises without any injury is a big warning sign. It means the body can’t make blood clots well. Ecchymoses can be big and very worrying.
Mucosal Bleeding (Nose, Gums)
Bleeding in the nose or gums is a serious sign. Blood in the nostrils or frequent nosebleeds are signs of severe thrombocytopenia. We need to take these signs seriously because they can lead to more serious bleeding.
“Bleeding signs such as petechiae, spontaneous bruises, nosebleeds, or blood in urine or stool are frequent clinical findings in patients with Grade 4 thrombocytopenia.”
Internal Bleeding Indicators
Seeing blood in urine or stool is a very serious sign. It means bleeding is happening inside the body, which can be dangerous. These signs need immediate medical help.
Diagnostic Approach to Grade4 Thrombocytopenia
Diagnosing Grade 4 thrombocytopenia needs a detailed approach. It includes several key tests. Early diagnosis is key for patient safety, allowing for quick action and management of risks.
Complete Blood Count Analysis
A Complete Blood Count (CBC) is the main tool for checking platelet levels. It gives vital info on the patient’s platelet count, which is key for diagnosing thrombocytopenia. A CBC also looks at white and red blood cells, helping spot other blood issues.
Peripheral Blood Smear Examination
A Peripheral Blood Smear test is also very important. It looks at blood under a microscope to check platelet and blood cell shapes. This test can find problems with platelet size and shape, helping figure out why thrombocytopenia is happening.
Bone Marrow Aspiration and Biopsy
In some cases, a Bone Marrow Aspiration and Biopsy is needed. This involves taking a bone marrow sample for testing. It helps see how platelets and other blood cells are made, giving insights into bone marrow health.
Additional Testing for Underlying Causes
More tests might be needed to find what’s causing Grade 4 thrombocytopenia. These include:
- Tests for infections and inflammation
- Imaging to check for spleen issues or other problems
- Immunological tests for autoimmune diseases
- Genetic tests for inherited platelet issues
By using these tests together, doctors can accurately diagnose Grade 4 thrombocytopenia. They can then create a treatment plan that fits the patient’s needs.
Treatment Strategies for Grade4 Thrombocytopenia
Managing Grade 4 thrombocytopenia needs a mix of treatments to prevent severe bleeding. These strategies aim to fix the root cause and handle serious side effects.
Platelet Transfusion Protocols
Platelet transfusions are key in treating Grade 4 thrombocytopenia. Platelet transfusion protocols help prevent and treat bleeding. We decide to transfuse platelets based on the count, the patient’s health, and if there’s bleeding.
We usually transfuse when the count drops below 10,000/μL or if there’s active bleeding. The goal is to safely increase the platelet count and lower bleeding risks. But, the success of transfusions can depend on several factors, like platelet antibodies and the cause of thrombocytopenia.
Thrombopoietin Receptor Agonists
Thrombopoietin receptor agonists boost platelet production in the bone marrow. Drugs like romiplostim and eltrombopag help increase platelet counts in patients with immune thrombocytopenia and other conditions.
These medications are a big step forward in treating thrombocytopenia. They offer hope for patients who don’t respond to other treatments. We use them for patients with persistent or hard-to-treat thrombocytopenia.
Immunosuppressive Therapies
For immune-related Grade 4 thrombocytopenia, immunosuppressive therapies are used. These treatments aim to stop the immune system from attacking platelets, helping platelet counts recover.
Corticosteroids are often the first choice. In tough cases, rituximab might be considered. The right treatment depends on the cause, the patient’s health, and other conditions.
Emergency Interventions for Life-Threatening Bleeding
When Grade 4 thrombocytopenia causes severe bleeding, quick action is needed. This might include immediate platelet transfusions, clotting factors, and other support to keep the patient stable.
It’s vital to quickly spot and treat severe bleeding. Handling life-threatening bleeding needs a team effort from many healthcare professionals, including hematologists and emergency doctors.
Conclusion: Prognosis and Long-term Management
Managing Grade4 thrombocytopenia needs a full plan. This plan covers both urgent needs and long-term goals. At Liv Hospital, we aim to give top-notch care to international patients. We follow international standards closely.
Understanding what causes thrombocytopenia is key. Then, we use the right treatments. How well a patient does depends on the cause, treatment success, and their health.
For long-term care, we watch platelet counts closely. We adjust treatments as needed. We also teach patients about bleeding signs and other issues.
Using treatments like thrombopoietin receptor agonists helps. So does using immunosuppressive therapies.
Healthcare teams can make a big difference with a proactive approach. Teaching patients how to manage their condition is very important. It helps them know when to get medical help.
FAQs
What is Grade 4 thrombocytopenia according to the CTCAE Version 5.0 grading system?
Grade 4 thrombocytopenia means your platelet count is below 25,000 per microliter. This is a severe drop in platelets. It can lead to serious and life-threatening bleeding.
How does the CTCAE Version 5.0 grading system assess thrombocytopenia, neutropenia, and anemia?
The CTCAE Version 5.0 grading system uses specific criteria for each condition. It looks at blood counts to assess severity. This helps in managing these conditions better.
What are the normal platelet count ranges, and what are the consequences of having a low platelet count?
Normal platelet counts are between 150,000 and 450,000 per microliter. A low count, or thrombocytopenia, raises the risk of bleeding. Severe cases (Grade 4) are very dangerous.
What are the common causes of Grade 4 thrombocytopenia?
Grade 4 thrombocytopenia can be caused by chemotherapy, immune thrombocytopenia (ITP), infections, or certain medications. Each case needs a specific treatment plan.
How is thrombocytopenia managed after a stem cell transplant?
After a stem cell transplant, managing thrombocytopenia involves understanding the recovery timeline. It includes monitoring, recovery strategies, and addressing neutropenia concerns to reduce risks.
What are the clinical manifestations and warning signs of Grade 4 thrombocytopenia?
Signs of Grade 4 thrombocytopenia include petechiae, purpura, and spontaneous bruising. Mucosal and internal bleeding are also indicators. These need immediate medical attention.
How is Grade 4 thrombocytopenia diagnosed?
Diagnosis involves a complete blood count and a peripheral blood smear. Bone marrow tests and other tests may also be needed. This ensures a thorough diagnosis.
What are the treatment strategies for Grade 4 thrombocytopenia?
Treatments include platelet transfusions and thrombopoietin receptor agonists. Immunosuppressive therapies and emergency care for severe bleeding are also used. The approach depends on the cause and severity.
What is the significance of understanding the pathophysiology behind severe platelet reduction?
Knowing why platelet counts drop is key to managing Grade 4 thrombocytopenia. Issues like bone marrow problems or platelet destruction need to be addressed for effective treatment.
How is long-term management of Grade 4 thrombocytopenia approached?
Long-term management involves regular monitoring and adjusting treatments as needed. Patient education is also important to ensure the best outcomes for those with Grade 4 thrombocytopenia.










