It’s important for women to know the difference between atypical endometrial hyperplasia and endometrial cancer. This is because atypical endometrial hyperplasia can turn into cancer. Research shows that a thicker uterine lining raises the risk of these issues, more so after menopause. Atypical endometrial hyperplasia is an alarming, high-risk diagnosis. This ultimate guide explains the critical link to cancer and powerful treatments.
Getting the right diagnosis and care is key for conditions like endometrial hyperplasia vs malignancy. At Liv Hospital, we focus on our patients, giving them the care they need.
Key Takeaways
- Understanding the differences between atypical endometrial hyperplasia and endometrial cancer is key.
- Atypical endometrial hyperplasia is a condition that can lead to cancer.
- A thicker uterine lining raises the risk of endometrial cancer, more so after menopause.
- Getting the right diagnosis is vital for effective treatment.
- Liv Hospital offers a patient-focused approach to managing these conditions.
The Endometrial Health Spectrum: From Normal to Pathological
The endometrial health spectrum includes everything from normal tissue to serious conditions like hyperplasia and cancer. Knowing this spectrum is key for correct diagnosis and treatment.
Normal Endometrial Tissue Structure
The normal endometrium changes with the menstrual cycle, thanks to hormones. It has glandular cells and stroma that grow and change with estrogen and progesterone.
Pathological Changes in the Endometrium
When hormones get out of balance, the endometrium can change for the worse. This leads to endometrial hyperplasia. Atypical Endometrial Hyperplasia (AEH) shows abnormal growth and cell changes, raising the risk of endometrial cancer.
Characteristics | Normal Endometrium | Endometrial Hyperplasia | Endometrial Cancer |
Glandular Structure | Regular, uniform glands | Crowded, irregular glands | Invasive glandular structures |
Cellular Atypia | Absent | Present in atypical hyperplasia | Marked cellular atypia |
Risk of Cancer | Low | Increased, specially in AEH | High |
It’s vital to understand these changes for early detection and treatment of endometrial problems. This can greatly improve patient outcomes.
Atypical Endometrial Hyperplasia: Definition and Significance
Atypical endometrial hyperplasia (AEH) is a serious condition that needs careful diagnosis and treatment. It can turn into endometrial cancer. AEH shows abnormal cell growth and atypia in the uterus lining.
Clinical Definition and Importance
AEH is known for its complex gland structure and abnormal cell look. It’s different from other endometrial hyperplasias. Its high risk of turning into endometrial cancer makes it very important.
Doctors use endometrial biopsy samples to diagnose AEH. They look for atypia and complex gland crowding.
The Premalignant Nature of AEH
AEH is a step towards cancer. It has genetic and molecular changes that raise cancer risk. Knowing this helps in planning treatment and follow-up.
Studies show AEH and endometrial cancer share genetic traits. Biomarkers and mutations help spot those at higher risk.
Types of Endometrial Hyperplasia: A Classification Overview
Endometrial hyperplasia is classified based on gland structure and cell atypia. This system helps understand the risks of each type.
Simple Hyperplasia Without Atypia
Simple hyperplasia without atypia has more endometrial glands. These glands are mostly regular in shape and size. It has a low risk of turning into cancer.
Research shows simple hyperplasia without atypia has a 1-3% risk of becoming endometrial cancer. This highlights the need for regular check-ups.
Complex Hyperplasia Without Atypia
Complex hyperplasia without atypia has more gland crowding and irregularity than simple hyperplasia. It has a higher risk of cancer than simple hyperplasia.
“The presence of complex hyperplasia without atypia signals a need for careful surveillance due to its increased risk of malignant transformation.”
Studies show complex hyperplasia without atypia has a 3-5% risk of turning into cancer.
Complex Atypical Hyperplasia
Complex atypical hyperplasia (CAH) is the most severe form. It has complex gland structure and cell atypia. CAH has a high risk of being or becoming endometrial carcinoma.
CAH’s risk is high, with up to 30% or more cases possibly having or becoming invasive cancer.
Knowing the different types of endometrial hyperplasia is key for doctors and patients. It helps in choosing the right treatment and understanding risks and follow-up needs.
Type of Hyperplasia | Characteristics | Cancer Risk |
Simple Hyperplasia Without Atypia | Increased number of glands, regular shape and size | 1-3% |
Complex Hyperplasia Without Atypia | Glandular crowding, irregular shapes | 3-5% |
Complex Atypical Hyperplasia | Complex glandular architecture, cellular atypia | Up to 30% or more |
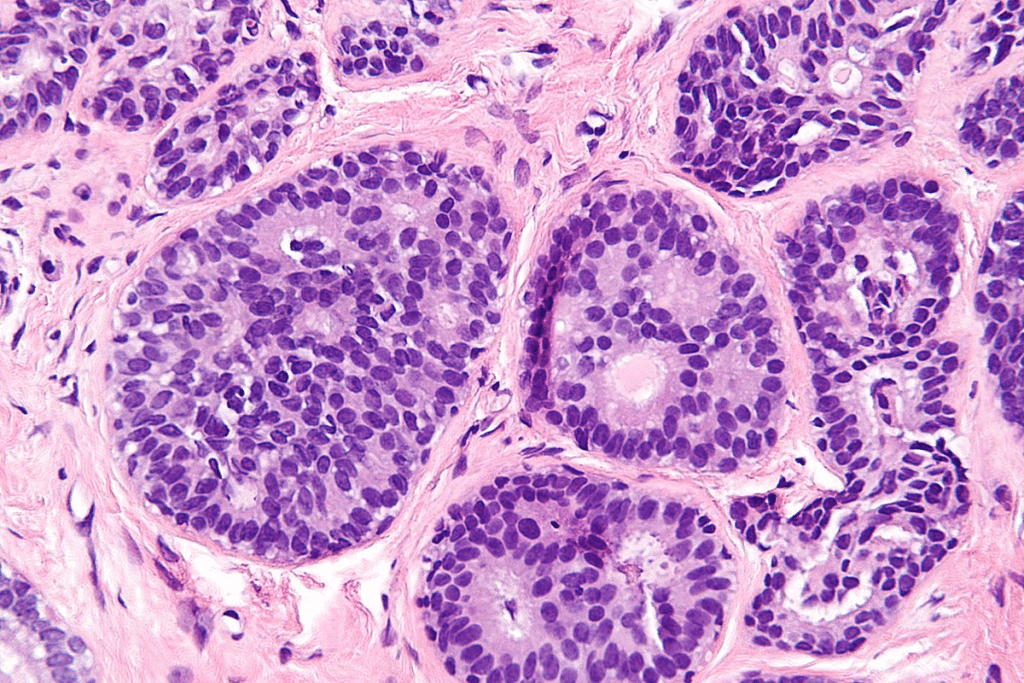
Difference #1: Histological Features and Cellular Architecture
The histological features of atypical endometrial hyperplasia (AEH) and endometrial cancer show a key difference. Knowing these differences is vital for correct diagnosis and treatment.
Glandular Crowding and Irregular Shapes in AEH
AEH is marked by glandular crowding and irregular gland shapes. These signs are unique to AEH and set it apart from other endometrial hyperplasias. The glands in AEH are packed tightly, with less stroma between them, creating a complex structure.
Invasive Patterns in Endometrial Cancer
Endometrial cancer, on the other hand, shows invasive patterns not seen in AEH. These include irregular growth into the surrounding stroma and a desmoplastic reaction. Invasion is a key factor that differentiates cancer from hyperplasia.
Gland-to-Stroma Ratio Comparisons
The gland-to-stroma ratio is another critical feature. In AEH, this ratio is high due to gland crowding. Comparing this ratio in AEH and endometrial cancer can shed light on the transition from hyperplasia to cancer.
Histological Feature | Atypical Endometrial Hyperplasia (AEH) | Endometrial Cancer |
Glandular Crowding | Present, with closely packed glands | May be present, but often with invasive patterns |
Gland Shapes | Irregular shapes | Variable, often with complex or cribriform patterns |
Gland-to-Stroma Ratio | Significantly increased | Variable, depending on the extent of invasion |
By studying these histological features, we gain insight into the differences between AEH and endometrial cancer. This knowledge leads to more precise diagnoses and treatments.
Difference #2: Nuclear Atypia and Cellular Characteristics
The cells and nuclei of atypical endometrial hyperplasia and endometrial cancer show key differences. One main difference is the amount and type of nuclear atypia.
Cytological Atypia in Hyperplasia
Atypical endometrial hyperplasia (AEH) has cytological atypia. This means the nuclei are not normal in size, shape, or color. An expert says, “Cytological atypia is a key sign of AEH, making it different from other hyperplasias.” Cytological atypia is when cells look abnormal, which is important for diagnosing AEH.
Malignant Nuclear Features in Carcinoma
Endometrial cancer, on the other hand, has more severe malignant nuclear features. These include big nuclei, uneven chromatin, and large nucleoli. These signs are more extreme than in AEH. A study found, “The nuclear signs in endometrial cancer are more aggressive. They show the cancer’s ability to spread and grow.”
Mitotic Activity Distinctions
Another difference is in mitotic activity. Endometrial cancer has a higher rate of cell division than AEH. This shows the cancer’s aggressive nature. Research points out, “Endometrial carcinoma has high mitotic rates. This is different from AEH’s lower rates.”
In summary, the differences in nuclear atypia, cytological atypia, malignant nuclear features, and mitotic activity are vital. They help doctors diagnose and plan treatment for AEH and endometrial cancer correctly.
Difference #3: Molecular and Genetic Markers
Recent studies show how important molecular markers are in telling AEH apart from endometrial cancer. Finding specific biomarkers and genetic mutations has really helped us understand these conditions better.
Biomarkers in Atypical Endometrial Hyperplasia
AEH has biomarkers that show it might turn into cancer. PTEN mutations are common in AEH. These mutations can start the PI3K/AKT signaling pathway, making cells grow more.
Other biomarkers like p53 and β-catenin also play a role in AEH. Their levels can tell us about the risk of the lesion getting worse.
Genetic Mutations in Endometrial Cancer
Endometrial cancer has its own set of genetic mutations. For example, POLE gene mutations are found in some cancers and are good news for patients.
Other common mutations in endometrial cancer include KRAS and PIK3CA. These mutations make the cancer grow faster and affect how it responds to treatment.
Molecular Progression Pathway
The change from AEH to endometrial cancer is complex. It involves many molecular events. Genetic and epigenetic changes lead to invasive cancer.
Knowing how AEH turns into endometrial cancer is key. It helps us find high-risk patients and create targeted treatments. By studying the genetic and molecular profiles of both conditions, we can understand how disease progression happens.
Difference #4: Clinical Presentation and Symptom Patterns
Atypical Endometrial Hyperplasia (AEH) and endometrial cancer share some symptoms. But, they have clear differences in how they show up. Both can cause abnormal bleeding in the uterus. This can be irregular periods, bleeding between periods, or bleeding after menopause.
Common Symptoms of AEH
AEH often shows up with:
- Abnormal uterine bleeding, which is often the primary symptom
- Menstrual irregularities, such as prolonged or heavy menstrual bleeding
- Intermenstrual bleeding, which can be a sign of hormonal imbalance
These symptoms are often non-specific. They can also show up in other gynecological conditions. This makes it hard to diagnose.
Warning Signs of Endometrial Cancer
Endometrial cancer shares some symptoms with AEH. But, it has clear warning signs. These include:
- Postmenopausal bleeding, which is a red flag for malignancy
- Unintended weight loss, which can be associated with advanced disease
- Pelvic pain or discomfort, which may indicate tumor invasion
These symptoms need immediate medical attention. They could mean cancer.
Distinguishing Features in Patient Presentation
Both AEH and endometrial cancer can cause abnormal bleeding. But, the nature and severity of the bleeding can vary. Endometrial cancer often causes bleeding after menopause. AEH usually causes irregularities in premenopausal women.
Knowing these differences is key for doctors. It helps them decide on the right tests and treatments.
Difference #5: Diagnostic Accuracy and Concurrent Malignancy
Diagnosing Atypical Endometrial Hyperplasia (AEH) is a big challenge in gynecology. It’s important to tell AEH apart from endometrial cancer. This is because their treatments and outcomes are very different.
Sampling Challenges in Diagnosis
Getting a good sample for diagnosing AEH is hard. Biopsies or curettage might not show the whole picture. This can lead to missing or wrong diagnoses.
Key challenges include:
- Insufficient sampling of the endometrium
- Variability in histological interpretation
- Difficulty in distinguishing between hyperplastic and malignant changes
Rate of Concurrent Cancer at AEH Diagnosis
Research shows many AEH cases have cancer at the same time. This affects how we treat patients and their outcomes. We’ll look at how common this is and why it matters.
Notably, studies show a big number of women with AEH also have cancer. This means we need to check them carefully and manage them well.
Study | Rate of Concurrent Cancer |
Study A | 25% |
Study B | 30% |
Study C | 20% |
Diagnostic Tools and Their Limitations
We use different tools to check for AEH and cancer, like looking at tissue, imaging, and molecular tests. But each tool has its own limits.
Diagnostic tools and their limitations:
- Histopathological examination: Subject to sampling error and variability in interpretation
- Imaging studies (e.g., ultrasound, MRI): Limited in their ability to distinguish between AEH and early-stage cancer
- Molecular diagnostics: Emerging biomarkers show promise but require further validation
Risk Factors for Developing Atypical Endometrial Hyperplasia
Knowing the risk factors for Atypical Endometrial Hyperplasia is key to catching it early. Hormonal, metabolic, and age-related factors all play a part.
Hormonal Influences and Estrogen Exposure
Hormonal imbalances, like too much estrogen, are big players in AEH. This can come from inside the body, like with PCOS, or from outside, like estrogen therapy without progesterone. Both can cause the lining of the uterus to grow too much.
Estrogen dominance can happen for many reasons. Being overweight is one, as it makes more estrogen and can cause inflammation and insulin resistance.
Metabolic Factors: Obesity, Diabetes, and PCOS
Metabolic issues raise the risk of AEH. Obesity is a big risk because it increases estrogen and causes inflammation. Diabetes, mainly type 2, also raises the risk, likely because of insulin resistance and metabolic syndrome.
Polycystic Ovary Syndrome (PCOS) is another big risk factor. It’s marked by hormonal imbalance, ovulation problems, and often insulin resistance. Women with PCOS are more likely to get AEH because of too much estrogen and metabolic issues.
Age-Related and Demographic Considerations
Age is a big deal for AEH, with more cases in perimenopausal and postmenopausal women. The risk goes up after 40.
Demographic factors also matter. Family history of endometrial or breast cancer can increase risk. Women with a family history of Lynch syndrome or other hereditary cancer syndromes are at higher risk.
Knowing these risk factors helps find women at high risk of AEH. It’s important for early prevention and monitoring.
Treatment Approaches: Balancing Conservation and Prevention
Treating atypical endometrial hyperplasia (AEH) is complex. It aims to stop cancer from getting worse while keeping fertility options open. We’ll look at different treatments, each with its own benefits and when to use them.
Conservative Management Options
For those wanting to keep their fertility, AEH can be managed carefully. This means regular check-ups and tests. Conservative management includes:
- Regular visits to a healthcare provider
- Endometrial biopsies at set times
- Ultrasound scans to watch the endometrium
This approach is best for women trying to get pregnant or who want to keep their uterus. But, they must understand the risks, like the chance of cancer.
Surgical Interventions and Their Indications
For many, surgical intervention is the best choice. Hysterectomy is common, recommended for those who’ve finished having kids or are at high cancer risk. Surgery’s decision depends on many factors, like risk, patient wishes, and symptoms.
When surgery is needed, it’s usually a total hysterectomy. The method, laparoscopic, robotic, or open, depends on health and surgeon skill.
Hormonal Therapies and Response Rates
Hormonal therapies are used for AEH, mainly for those not ready for surgery. Progestin therapy is common, as it helps prevent cancer by balancing estrogen’s effects.
How well hormonal therapy works varies. Regular checks are key to see if it’s working. Factors affecting success include:
- The type and amount of progestin
- How long treatment lasts
- Individual health, like obesity
Patients on hormonal therapy for AEH need close monitoring. This ensures the treatment is working and catches any signs of failure or cancer early.
Surveillance Protocols and Follow-up Recommendations
When atypical endometrial hyperplasia (AEH) is diagnosed, a careful watch plan is needed. This plan helps catch any signs of endometrial cancer early. It’s key to manage AEH and stop it from turning into endometrial cancer.
Monitoring After AEH Diagnosis
After finding AEH, it’s important to keep a close eye on the endometrium. We suggest a follow-up plan with regular visits and tests. This helps track the endometrium’s health.
Key components of monitoring after AEH diagnosis include:
- Regular pelvic exams to check for any changes in the reproductive area
- Transvaginal ultrasound to watch the endometrium’s thickness and look
- Endometrial biopsy to check for any cell changes or cancer signs
Post-treatment Surveillance Strategies
After treating AEH, it’s vital to keep watching to make sure it doesn’t come back or turn into cancer. We advise a post-treatment plan with regular check-ups and tests.
Post-treatment surveillance strategies may include:
- Regular visits with a healthcare provider to watch for any signs of return or growth
- Imaging studies like ultrasound or MRI to check the endometrium for changes
- Endometrial biopsy to look for any cell changes or return
Long-term Risk Management Approaches
Managing AEH’s long-term risk needs a full plan. This includes lifestyle changes, reducing risk factors, and ongoing checks. We suggest patients with AEH history live a healthy life. This includes eating well and exercising regularly to lower cancer risk.
Long-term risk management approaches include:
Risk Factor | Management Strategy |
Obesity | Weight loss through diet and exercise |
Hormonal imbalance | Hormonal therapy or other treatments to balance hormone levels |
Family history | Regular surveillance and genetic counseling |
Conclusion: Navigating the Complex Landscape of Endometrial Pathology
It’s key to know the difference between atypical endometrial hyperplasia and endometrial cancer. This knowledge helps in managing these conditions better and improving patient care. We’ve talked about the main differences, risk factors, and how to treat them.
Knowing the difference between these two conditions is vital for the right treatment. Healthcare providers can use specific features and markers to plan the best treatment. This way, they can target the treatment more effectively.
Managing endometrial pathology well means using a complete approach. This includes regular checks and follow-up plans. It’s important to find a balance between treating the condition and preventing it. This ensures patients get the best care possible.
By understanding endometrial pathology, we can help patients better. We aim to provide full support to those dealing with these conditions.
FAQ
What is the difference between atypical endometrial hyperplasia and endometrial cancer?
Atypical endometrial hyperplasia (AEH) is a condition where cells grow abnormally. It’s a step before cancer. Endometrial cancer is a tumor that grows in the uterus. AEH can turn into endometrial cancer.
What are the symptoms of atypical endometrial hyperplasia?
Symptoms of AEH are similar to those of endometrial cancer. They include bleeding that’s not normal, long periods of bleeding, or bleeding in between periods.
How is atypical endometrial hyperplasia diagnosed?
Doctors diagnose AEH by looking at tissue samples from the uterus. They look for signs like crowded glands and abnormal cells.
What are the risk factors for developing atypical endometrial hyperplasia?
Factors that increase the risk of AEH include hormonal changes, obesity, diabetes, and age.
How is atypical endometrial hyperplasia treated?
Treatment for AEH includes hormone therapy, surgery, or watching the condition closely. This helps prevent it from turning into cancer.
What is complex atypical hyperplasia of the endometrium?
Complex atypical hyperplasia is a more serious form of AEH. It has complex gland structures and abnormal cells. It’s at higher risk of becoming cancer.
Can atypical endometrial hyperplasia be prevented?
While AEH can’t be completely stopped, managing risk factors helps. Regular check-ups are also important for early detection and treatment.
What is the significance of nuclear atypia in atypical endometrial hyperplasia?
Nuclear atypia is key in diagnosing AEH. It shows abnormal cell changes that can lead to cancer.
How does endometrial hyperplasia with atypia differ from simple endometrial hyperplasia?
AEH has a higher risk of becoming cancer than simple endometrial hyperplasia. This is because of the abnormal cell changes.
What are the molecular and genetic markers associated with atypical endometrial hyperplasia and endometrial cancer?
Biomarkers and genetic mutations help understand how AEH turns into cancer. They are important for research and treatment.
What is the role of surveillance protocols in managing atypical endometrial hyperplasia?
Surveillance is key in managing AEH. It involves regular check-ups to catch any changes early and prevent cancer.








