Last Updated on November 13, 2025 by
Thrombocytopenia is a condition where you have too few platelets in your blood. This can cause bleeding problems. Normal platelet counts range from 150 to 450 ×10 ³ per μL. We will look at how the World Health Organization (WHO) grades thrombocytopenia. This is key for diagnosing and treating the condition.
The WHO grades thrombocytopenia based on how low the platelet count is. It’s divided into mild (100-150 ×10â¹/L), moderate (50-99 ×10â¹/L), and severe (
It’s key for doctors to know about thrombocytopenia to give the right care. This condition, with low platelet counts, can be mild or severe. It has many causes and effects on health.
Thrombocytopenia means having too few platelets. Platelets should be between 150 × 10â¹/L and 450 × 10â¹/L. If they’re lower, you have thrombocytopenia. The level of platelets shows how severe it is.
The causes of thrombocytopenia include making fewer platelets, losing more, or having them stuck somewhere.
Getting the platelet count right is key to diagnosing thrombocytopenia. Mild thrombocytopenia might not show symptoms, but it can mean there’s something wrong. The grading system helps doctors know how serious it is.
Even mild thrombocytopenia can point to big health problems. Doctors need to check further.
Thrombocytopenia can lead to bleeding problems. The risk of bleeding depends on how severe the thrombocytopenia is. Knowing the causes and how severe it is helps manage it better.
The WHO has updated its thrombocytopenia grading systems over time. This change is due to new clinical evidence and practices. It shows the effort to improve patient care and outcomes in thrombocytopenia.
Thrombocytopenia classification has changed a lot over the years. Early systems were simple and didn’t fully capture the complexity of chronic thrombocytopenia.
As we learned more about blood disorders, the classification systems got better. New lab tests and insights led to more detailed grading. For example, recognizing chronic thrombocytopenia as a unique condition changed how it’s graded and treated.
The development of these systems helped create today’s WHO standards. Knowing how thrombocytopenia classification evolved helps us understand today’s guidelines better.
The current WHO grading system for thrombocytopenia is the result of years of research and practice. It uses a detailed understanding of platelet counts and their clinical effects. This includes the risks of low platelet count.
The WHO now grades thrombocytopenia based on its severity. This grading is key to choosing the right treatment for patients, mainly those with chronic forms.
“The WHO grading system provides a standardized framework for assessing thrombocytopenia, facilitating consistent clinical decision-making across different healthcare settings.”
Using a standardized grading system helps healthcare providers manage thrombocytopenia better. They can tailor treatments to each patient’s needs based on their condition.
It’s key to know the WHO grading criteria for thrombocytopenia to diagnose and manage it well. Thrombocytopenia is when you have too few platelets, leading to bleeding and bruising. The WHO grading helps standardize how severe it is.
The WHO grades thrombocytopenia into four levels based on platelet counts. This system is important for figuring out how serious it is and what treatment to use.
A medical expert says, “The WHO grading system helps doctors quickly see how bad thrombocytopenia is and make the right care choices.”
“Getting thrombocytopenia right is key to managing it well and avoiding problems.”
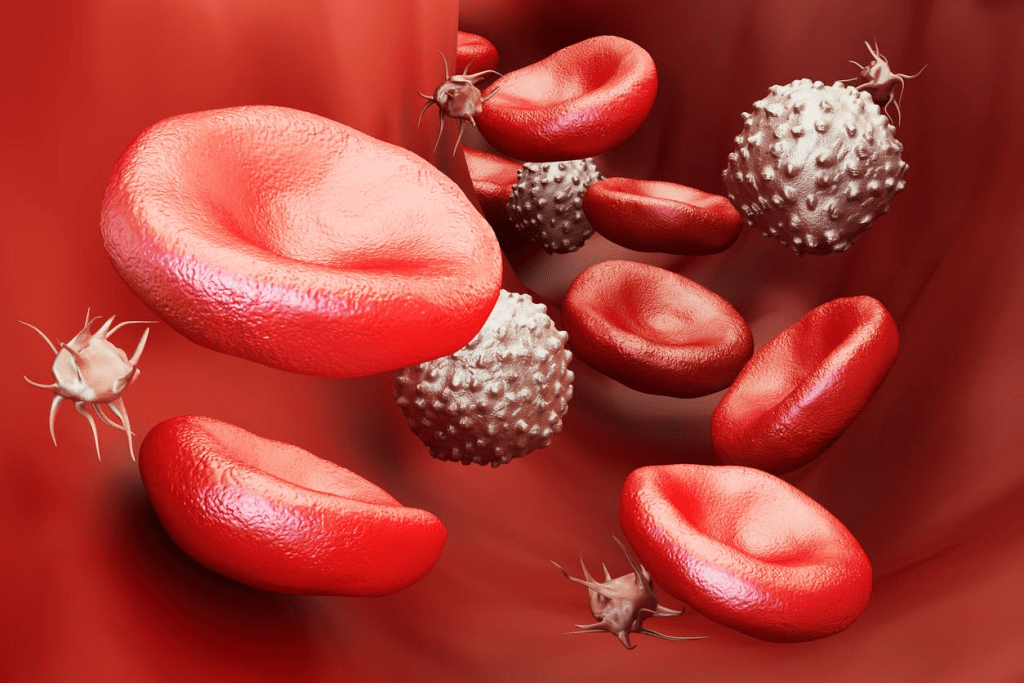
Lab tests, like platelet count, are vital for diagnosing and grading thrombocytopenia. The normal range can vary, but usually, under 150 × 10^9/L is low.
To define low platelet count, doctors use lab tests. The symptoms of thrombocytopenia depend on how bad it is. Common signs include bruising, petechiae, and bleeding that won’t stop.
Knowing these lab values and ranges is key to accurate diagnosis and grading. It helps doctors create the right treatment plans.
When patients have mild thrombocytopenia, with a platelet count of 100-150 ×10â¹/L, doctors must think carefully. This condition is often without symptoms but can signal a problem that needs attention. We will explore the importance of mild thrombocytopenia, including how to assess risks and manage it.
Mild thrombocytopenia might not cause serious bleeding, but it’s important to watch for worsening. A detailed thrombocytopenia workup is key to the cause. This could be something simple or a serious disease.
Understanding mild thrombocytopenia involves looking at:
Managing mild thrombocytopenia means keeping an eye on platelet counts and treating the cause. For symptomatic thrombocytopenia, treatment is needed to avoid complications.
Important management steps include:
In some cases, mild thrombocytopenia might get better once the cause is treated. But it’s important to keep watching to make sure it doesn’t get worse.
When platelet counts drop to 50-99 ×10â¹/L, patients face moderate thrombocytopenia. This condition requires a careful approach. We must balance preventing bleeding with the risks of treatment.
Moderate thrombocytopenia raises the risk of bleeding. This can happen on its own or with minor injuries. It affects patient care, including surgeries and managing other health issues.
Some key implications include:
The risk of bleeding in moderate thrombocytopenia is a big concern. We must assess this risk carefully. We look at the patient’s condition, any other health issues, and medications that affect blood clotting.
Treatment for moderate thrombocytopenia includes:
Understanding the clinical implications and bleeding risks of moderate thrombocytopenia helps us manage it better. This improves patient outcomes.
Severe thrombocytopenia is a serious condition where the platelet count is very low, usually under 50,000/microliter. It is classified as a severe condition. This means there’s a big risk of bleeding, even without any injury. At counts below 10,000/microliter, bleeding can happen on its own. Counts below 50,000/microL increase the risk of bleeding during surgery as outlined in medical literature.
Emergency Management Protocols for Thrombocytopenia
It’s very important to have emergency plans for severe thrombocytopenia. This is to stop life-threatening bleeding. Quick and right action is key to keeping patients safe.
How severe thrombocytopenia is depends on the platelet count. It’s considered a medical emergency. Knowing the risks and acting fast can help avoid serious problems.
Thrombocytopenia is a condition where you have too few platelets. This can make it harder for your blood to clot, leading to more bleeding.
Normal platelet counts usually range from 150 to 450 ×10â¹/L. But these numbers can vary slightly from one lab to another.
The WHO system divides thrombocytopenia into four grades. Grade 1 is 100-150 ×10â¹/L, Grade 2 is 50-99 ×10â¹/L, Grade 3 is 20-49 ×10â¹/L, and Grade 4 is below 20 ×10â¹/L.
Mild thrombocytopenia means your platelet count is between 100-150 ×10â¹/L. It might not cause symptoms, but could show a health issue that needs watching.
For a platelet count of 50-99 ×10â¹/L, managing it carefully is key. It’s about avoiding bleeding risks while considering treatment side effects.
Severe thrombocytopenia, with counts below 20 ×10â¹/L, is very serious. It needs quick and effective treatment to stop severe bleeding.
To diagnose thrombocytopenia, accurate platelet counts are essential. The platelet count is the main lab test used.
Yes, even mild thrombocytopenia can signal a health problem. It’s important to do thorough checks and assessments.
The WHO grading system has changed over time. It now includes the latest research and understanding of thrombocytopenia, leading to the current system.
For severe thrombocytopenia, quick action is needed to prevent serious bleeding. This includes giving platelet transfusions and other supportive care.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!