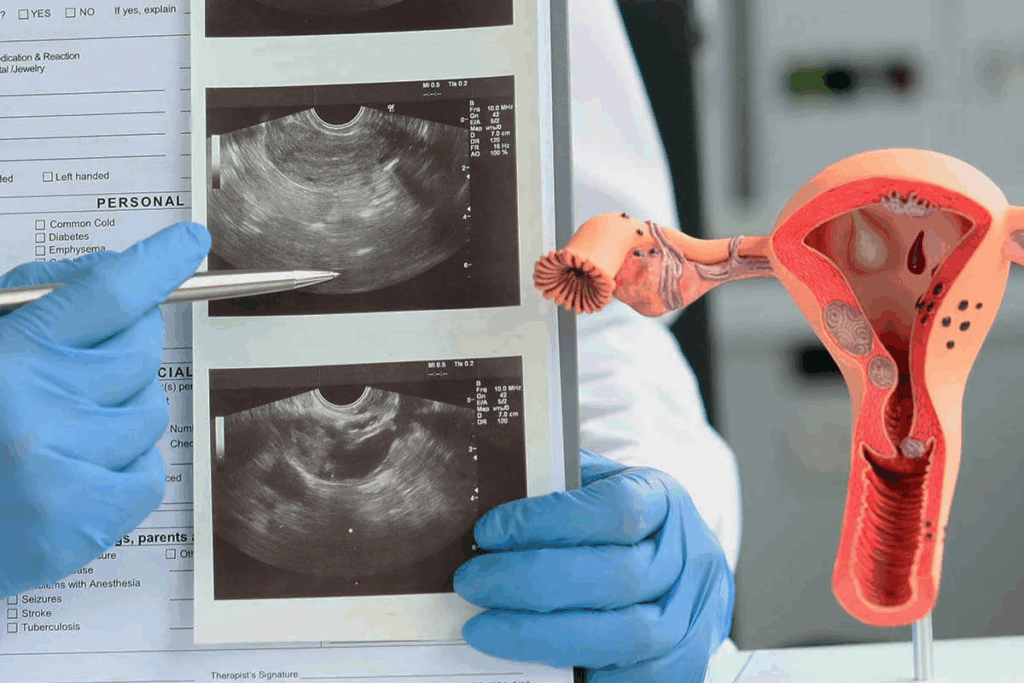
A thick uterine lining, or endometrial hyperplasia, is when the lining of the uterus gets too thick. This is often seen on transvaginal ultrasound. This tool gives a clear view of the uterine lining what does a thick uterine wall mean.
The lining of the uterus is key for getting pregnant and supporting a growing baby. When it gets too thick, it can make it hard to get pregnant. It also raises the risk of miscarriage or cancer. At Liv Hospital, we focus on our patients. We use the latest imaging and medicine to help them.
Key Takeaways
- Endometrial hyperplasia is a condition characterized by the abnormal thickening of the uterine lining.
- Transvaginal ultrasound is a diagnostic tool used to detect endometrial hyperplasia.
- Hormonal imbalance is a common cause of endometrial hyperplasia.
- Abnormal uterine lining thickening can lead to difficulties in conception and increased health risks.
- Patient-centered care is essential for effective management and treatment of endometrial hyperplasia.
Understanding the Uterine Lining
The endometrium is a dynamic layer of tissue that changes a lot during a woman’s menstrual cycle. It’s key for conception and pregnancy. We’ll look at its structure, function, and how it changes.
Structure and Function of the Endometrium
The endometrium has two layers: the basal layer and the functional layer. The basal layer regenerates after each period. The functional layer thickens for pregnancy. If not pregnant, it sheds during menstruation.
The endometrium’s thickness changes with estrogen and progesterone levels. Estrogen makes it thicker during the first part of the cycle. Progesterone prepares it for a fertilized egg after ovulation.
Normal Changes Throughout the Menstrual Cycle
The endometrium changes a lot due to hormone shifts. In the menstrual phase, it sheds, causing bleeding. Then, it regenerates and thickens in the proliferative phase with estrogen.
In the secretory phase after ovulation, it gets thicker and more vascular. This prepares it for implantation. If not, it sheds again, starting a new cycle.
Knowing these changes helps spot problems like an unusually thick endometrium. Ultrasound can detect this.
What Does a Thick Uterine Wall Mean?
A ‘thick uterine wall’ means the lining of the uterus, called the endometrium, is too thick. This is known as endometrial hyperplasia.
Endometrial hyperplasia happens when too many cells grow in the uterine lining. This usually comes from too much estrogen without enough progesterone to balance it.
Definition of Endometrial Hyperplasia
Endometrial hyperplasia makes the endometrium thicker. This can be seen with an ultrasound. When it gets too thick, it’s seen as abnormal based on age, menstrual status, and other factors. It can be simple or complex, with or without atypia, showing different risks for cancer.
“The presence of atypia in endometrial hyperplasia significantly increases the risk of cancer, making accurate diagnosis critical.”
Significance of Endometrial Thickening
Endometrial thickening is important because of its risks and effects on women’s health. Endometrial hyperplasia can lead to endometrial cancer, mainly in postmenopausal women. So, getting it diagnosed and treated right is key to avoiding serious problems.
Knowing the causes, symptoms, and treatments for endometrial hyperplasia is vital. We’ll dive into these to fully understand what a thick uterine wall is and how to handle it.
How Ultrasound Detects Uterine Lining Thickness
Ultrasound is a key tool for checking the uterine lining thickness. It lets doctors look at the uterine lining without surgery. This is important for diagnosing and treating many gynecological issues.
There are two main ways to do an ultrasound: transvaginal and transabdominal. Transvaginal ultrasound gives a clearer view because the probe is closer. It’s great for accurately measuring the uterine lining thickness.
Transvaginal vs. Transabdominal Ultrasound
Transvaginal ultrasound uses a special probe in the vagina. It gives high-resolution images of the uterine lining. This is good for spotting small issues. Transabdominal ultrasound uses a probe on the belly. It shows more of the pelvic area but might not be as detailed for lining thickness.
We usually suggest transvaginal ultrasound for precise uterine lining checks.
What Radiologists Look For During Endometrial Assessment
Radiologists examine the endometrium’s thickness and brightness during an ultrasound. They measure the thickest part of the lining. The brightness of the lining can tell them about its texture and any problems.
They look for any odd thickness or patterns in the lining. This could mean polyps or other growths. They also check if the lining looks right for the patient’s cycle and hormones.
Normal vs. Abnormal Endometrial Thickness
It’s important to know the difference between normal and abnormal endometrial thickness. This is key for correct diagnosis and treatment. The endometrium’s thickness changes throughout a woman’s cycle and life. So, it’s vital to look at these changes when checking thickness.
Normal Measurements by Age and Menstrual Status
Normal endometrial thickness varies a lot. It depends on age, menstrual status, and other factors. For example:
- In premenopausal women, thickness can be between 4 to 14 mm, based on the menstrual cycle stage.
- Postmenopausal women usually have a thinner endometrium, under 5 mm.
- Women on hormone replacement therapy (HRT) might have a thicker endometrium.
These differences show why it’s important to consider individual factors when checking endometrial thickness.
When Thickness Is Considered Abnormal on Ultrasound
Abnormal endometrial thickness can mean different gynecological issues. On ultrasound, a thickness outside the expected range for age and menstrual status is seen as abnormal. For example:
- More than 14 mm in premenopausal women, if it stays the same throughout the cycle.
- More than 5 mm in postmenopausal women.
Such findings might point to conditions like endometrial hyperplasia or cancer. They need more investigation.
Endometrial Echogenicity and Texture Considerations
The echogenicity and texture of the endometrium are also key in ultrasound checks. Echogenicity is how the endometrium looks on ultrasound. Different looks can mean different conditions:
- A homogeneous endometrium looks uniform.
- A heterogeneous look might mean polyps or other issues.
A leading gynecologist says, “Looking at the endometrium’s echogenicity and texture is as important as measuring its thickness. These details together give a full picture of the endometrium’s health.”
“Ultrasound checks of the endometrium are complex. They involve measuring thickness and looking at echogenicity and texture. This detailed look is key for spotting issues early.”
By looking at both thickness and echogenicity/texture, doctors can make better diagnoses. They can then plan the right treatment.
Common Causes of Thick Uterine Lining
Many health issues can make the uterine lining thicker. These include hormonal imbalances and certain medical conditions. Knowing what causes this is key to finding the right treatment.
Hormonal Imbalances Between Estrogen and Progesterone
Too much estrogen compared to progesterone often causes a thick uterine lining. Estrogen grows the endometrium, while progesterone prepares it for pregnancy. Without the right balance, the lining can grow too much.
We’ll look at how treatments and some health conditions can upset this balance. This can make the uterine lining thicker.
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder that can disrupt menstrual cycles. It leads to too much estrogen and a thick uterine lining. Women with PCOS are more likely to develop endometrial hyperplasia.
Obesity and Metabolic Factors
Being overweight can also make the uterine lining thicker. Fat tissue can turn androgens into estrogens, raising estrogen levels. This increases the risk of endometrial hyperplasia and other issues.
We’ll dive into how obesity and metabolic factors affect uterine lining thickness. Maintaining a healthy weight is vital.
Medications and Treatments (Including Tamoxifen)
Some medicines, like tamoxifen for breast cancer, can also thicken the uterine lining. Tamoxifen blocks estrogen in breast tissue but can act like estrogen on the uterus. This can cause endometrial hyperplasia.
We’ll discuss other medicines and treatments that can disrupt hormonal balances. This can lead to a thickened uterine lining. It’s important to monitor and manage these effects carefully.
Cause | Description | Risk Factors |
Hormonal Imbalance | Excess estrogen relative to progesterone | Irregular menstrual cycles, anovulatory cycles |
PCOS | Hormonal disorder causing irregular cycles | Infertility, obesity, insulin resistance |
Obesity | Adipose tissue converts androgens to estrogens | Metabolic syndrome, diabetes, hypertension |
Tamoxifen | Estrogen-like effects on the uterus | Breast cancer treatment, endometrial cancer risk |
Benign Conditions Associated with Thickened Endometrium
Many benign conditions can make the uterine lining thicker. These are common and can affect a woman’s health and well-being. We will look at these conditions and how they relate to a thickened endometrium.
Endometrial Polyps
Endometrial polyps grow on the uterus lining, known as the endometrium. They are usually not cancerous and can be different sizes. These polyps grow because of too many cells in the endometrium, often due to hormones like estrogen.
Characteristics of Endometrial Polyps:
- Typically benign
- Can cause irregular bleeding
- May be associated with infertility
- Often found in women of reproductive age
Uterine Fibroids
Uterine fibroids are non-cancerous growths in or around the uterus. They are also called leiomyomas and can be any size. Fibroids can be inside the uterine wall or on the outside, causing the lining to thicken.
Key Features of Uterine Fibroids:
Feature | Description |
Location | Can occur within the uterine wall or on the outer surface |
Size | Can range from small to large |
Symptoms | May cause heavy menstrual bleeding, pelvic pressure, or infertility |
Adenomyosis
Adenomyosis is when tissue like the uterus lining grows outside the lining, into the muscular walls. This can make the uterine wall thick and often causes heavy or painful periods.
Common Symptoms of Adenomyosis:
- Heavy or prolonged menstrual bleeding
- Severe menstrual cramps
- Pelvic pressure or pain
Knowing about these benign conditions is key to treating a thickened endometrium. We will keep exploring their effects in the next sections.
When Thickened Uterine Lining May Indicate Cancer
A thickened uterine lining can worry you, as it might show a risk of endometrial cancer. Many times, it’s not cancer, but some signs can point to it. These signs and risk factors are important to know.
Endometrial Cancer Risk Factors
There are several factors that raise the chance of getting endometrial cancer. These include:
- Unopposed estrogen exposure, which can happen in women with irregular ovulation or those who haven’t had a period for a while
- Obesity, as extra body fat can cause more estrogen
- Certain genetic syndromes, like Lynch syndrome
- Family history of endometrial or other cancers
- Previous radiation therapy to the pelvis
Knowing these risk factors helps figure out if a thickened uterine lining might be cancer.
Distinguishing Benign vs. Malignant Thickening on Ultrasound
Ultrasound is key in checking if a thickened uterine lining is cancer. Some signs on ultrasound might mean it’s cancer. These signs include:
- Heterogeneous or irregular texture of the endometrium
- Presence of a distinct mass within the endometrium
- Irregular or disrupted endometrial-myometrial junction
- Increased vascularity within the endometrium
Radiologists look at these signs to guess if it’s cancer. They suggest more tests if they think it might be.
But, remember, ultrasound isn’t the only way to know for sure if it’s cancer. More tests, like a biopsy, are usually needed to confirm cancer.
Symptoms That May Accompany a Thick Uterine Lining
A thickened uterine lining can cause several symptoms. One key symptom is abnormal uterine bleeding. This symptom needs further investigation. Symptoms can vary and affect a woman’s life quality.
Abnormal Uterine Bleeding Patterns
Abnormal uterine bleeding is a common symptom of a thick uterine lining. It can show up as:
- Heavy or prolonged menstrual bleeding
- Irregular menstrual cycles
- Intermenstrual bleeding
- Postmenopausal bleeding
These bleeding patterns are not normal. They need a medical check-up to find the cause.
Other Associated Symptoms
Women with a thickened uterine lining may also have other symptoms. These include:
- Pelvic pain or discomfort
- Bloating or abdominal distension
- Infertility or difficulty conceiving
These symptoms can be due to hormonal imbalances, endometrial polyps, or other gynecological issues.
When to Seek Medical Attention
Seek medical help if you notice any unusual symptoms. This includes:
- Unusual or heavy vaginal bleeding
- Severe pelvic pain
- Postmenopausal bleeding
- Difficulty conceiving
If you’re experiencing these symptoms, see a healthcare provider. They can evaluate and diagnose you. Early treatment can greatly improve your outcome.
Diagnostic Procedures Following Ultrasound Detection
Seeing a thickened uterine lining on ultrasound is just the start. More tests are needed to find the cause and the right treatment.
When we spot a thickened uterine lining, we must do more tests. We want to know why it’s thickened and check for serious issues.
Endometrial Biopsy
An endometrial biopsy takes a tissue sample from the uterus lining. It’s checked for abnormal cells or cancer.
This test is done in a doctor’s office and might feel like menstrual cramps. A thin tube is used to get a tissue sample from the uterus.
Hysteroscopy
A hysteroscopy lets a doctor see inside the uterus with a thin telescope. It helps find problems like polyps or fibroids that might cause the lining to thicken.
During hysteroscopy, the telescope is put through the cervix into the uterus. The doctor can see the uterus on a screen and might remove polyps or fibroids if needed.
Additional Imaging Tests
In some cases, more tests are needed to check the uterine lining. These can include:
- Sonohysterography: This fills the uterus with saline before an ultrasound for better views.
- Magnetic Resonance Imaging (MRI): An MRI gives detailed images of the uterus to spot problems like adenomyosis or fibroids.
These tests are key to figuring out why the uterine lining is thick and finding the right treatment. Knowing the cause helps doctors create a treatment plan just for you.
Treatment Options for Thickened Endometrium
There are many ways to treat a thickened endometrium, depending on the cause and how severe it is. We’ll look at the different treatments, focusing on what works best for each case.
Hormonal Treatments
Hormonal therapies are often the first choice for a thickened endometrium, mainly due to hormonal imbalances. Progestins and birth control pills are used to balance hormones and shrink the endometrium. They add progesterone to balance out estrogen, helping the lining of the uterus to return to normal.
Women with Polycystic Ovary Syndrome (PCOS) find hormonal treatments very helpful. These treatments help manage symptoms and reduce the risk of serious problems like endometrial hyperplasia.
Surgical Interventions
When hormonal treatments don’t work or if there’s a risk of cancer, surgery might be needed. A Dilation and Curettage (D&C) is a common surgery that removes the endometrial lining. It helps relieve symptoms and can help diagnose and treat problems.
In some cases, a hysterectomy is recommended for severe symptoms or a high cancer risk. This surgery removes the uterus and can be a lasting solution for managing a thickened endometrium.
Lifestyle Modifications and Prevention Strategies
Medical treatments aren’t the only way to manage a thickened endometrium. Lifestyle changes are also key. Eating well, staying active, and keeping a healthy weight can help balance hormones and prevent thickening.
Women at risk, like those with PCOS or obesity, can greatly benefit from these lifestyle changes. Knowing the risks of certain medicines, like Tamoxifen, and talking to a doctor about safer options is also important.
By understanding the treatment options and making smart choices, women can manage a thickened endometrium and lower the risk of complications.
Conclusion
Knowing about a thick uterine lining seen on ultrasound is key for women’s health. We’ve looked at how the uterine lining changes, its possible causes, and what it means for health.
Ultrasound is important for spotting and measuring the uterine lining’s thickness. A thick lining might mean different things, like harmless growths or serious diseases like cancer.
We talked about how to tell if a thick lining is normal or not, the tests that come after an ultrasound, and treatment choices. These include hormone therapy, surgery, and changes in lifestyle.
In short, a thick uterine lining needs more checks to find out why. By knowing the reasons, tests, and treatments, doctors can help patients get the best care.
FAQ
What does a thickened uterine lining mean on an ultrasound?
A thickened uterine lining, or endometrial hyperplasia, can be normal. But it might also mean health issues like hormonal imbalances or cancer.
What is considered a normal endometrial thickness?
Normal endometrial thickness varies by age and menstrual status. For postmenopausal women, it’s under 5 mm. For premenopausal women, it’s 4-16 mm, depending on the cycle stage.
What causes the uterine lining to thicken?
The uterine lining thickens with hormonal changes, like more estrogen during the cycle. Hormonal imbalances, PCOS, obesity, and some meds can also cause it to thicken.
Can a thickened uterine lining be a sign of cancer?
A thickened uterine lining might mean different things, including cancer. But it’s not a sure sign. Doctors use ultrasounds and biopsies to find out why it’s thickening.
What are the symptoms associated with a thickened uterine lining?
Symptoms include heavy or irregular periods, bleeding between periods, or after menopause. You might also feel pelvic pain or discomfort.
How is a thickened uterine lining diagnosed?
Doctors use ultrasounds, biopsies, and other tests like hysteroscopy to diagnose. They look for the cause of the thickening.
What are the treatment options for a thickened uterine lining?
Treatment depends on the cause. It might include hormonal therapies, surgery, or lifestyle changes.
Can lifestyle changes help prevent or manage a thickened uterine lining?
Yes, staying healthy, managing stress, and avoiding certain meds can help prevent or manage it.
Is a thickened uterine lining a common condition?
Yes, it’s common, mainly in women of childbearing age.
When should I seek medical attention for a thickened uterine lining?
If you have abnormal bleeding, pelvic pain, or other symptoms, see a doctor. They can find the cause and treat it.
References
National Center for Biotechnology Information. Thick Uterine Lining on Ultrasound: Endometrial Hyperplasia. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11989014/








