Can you see endometriosis on ultrasound? This ultimate guide reveals the surprising, critical truth about the limitations of scans for diagnosis. Endometriosis affects about 1 in 9 women. It usually takes 6.4 years to diagnose using old methods. At Liv Hospital, we focus on patient care with specialized imaging protocols and trusted experts.
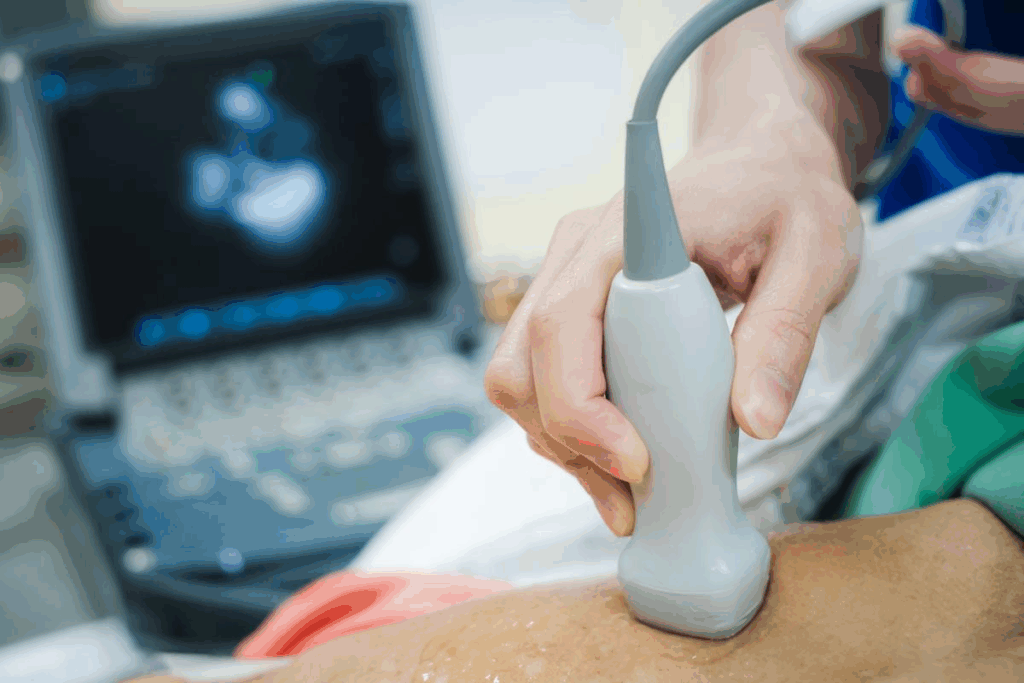
Advanced pelvic ultrasound technology is a non-invasive way to quickly find the cause. It cuts down on delays and risks from surgery. Transvaginal ultrasound can spot deep endometriosis and endometriomas with sensitivity of 88-96% and specificity of 79-94%.
We use this tech to see endometriosis clearly and plan better treatments. With the latest ultrasound tech, we give our patients fast and effective care.
Key Takeaways
- Advanced pelvic ultrasound technology can expedite endometriosis diagnosis.
- Transvaginal ultrasound has high sensitivity and specificity for detecting deep endometriosis.
- Liv Hospital offers patient-centered care through specialized imaging protocols.
- Non-invasive ultrasound reduces diagnostic delays and surgical risks.
- Accurate visualization of endometriosis enables improved treatment planning.
Understanding Endometriosis and Diagnostic Challenges
It’s key to understand endometriosis to tackle its diagnostic hurdles. This condition is complex and painful, impacting many globally.
What is Endometriosis?
Endometriosis happens when uterine lining tissue grows outside the uterus. This causes inflammation, scarring, and painful adhesions. It affects 6% to 10% of individuals of reproductive age.
It can lead to severe pain, infertility, and heavy periods. Symptoms vary widely, making diagnosis tough.
The exact cause of endometriosis is unknown. Hormonal, genetic, and environmental factors are thought to play a role. Knowing these factors helps in finding better ways to diagnose and treat it.
Why Diagnosis is Often Delayed
Diagnosing endometriosis is hard because its symptoms are similar to other conditions. The severity of symptoms doesn’t always match the disease’s extent. This makes diagnosis even more challenging.
The journey to diagnosis can be tough for patients. The average delay between symptom onset and diagnosis is often several years. During this time, patients may see many doctors and undergo many tests. We need to improve our understanding of endometriosis to reduce this delay and offer better care.
By recognizing the complexities of endometriosis and its diagnostic challenges, we can improve diagnostic methods and patient outcomes. Ultrasound’s role in detecting endometriosis is key. Ongoing research aims to make ultrasounds more accurate.
Types of Ultrasound Used to Detect Endometriosis
Ultrasound technology is key in diagnosing endometriosis. Various types of ultrasound are used to see the reproductive organs. They help find signs of endometriosis.
Transabdominal Ultrasound
Transabdominal ultrasound scans the pelvic area from the abdomen. It gives a wide view of the pelvic organs. But, it might miss small endometriotic lesions.
Limitations: It’s not as good for detailed looks at the uterus and ovaries. This is true, mainly for women with a higher body mass index (BMI).
Transvaginal Ultrasound (TVUS)
TVUS is more precise than transabdominal ultrasound for the uterus and ovaries. It uses an ultrasound probe in the vagina. This gives clearer images of the reproductive organs.
Specialized Endometriosis Protocols
Special ultrasound protocols for endometriosis are available at big medical centers. They focus on the pelvic structures often hit by endometriosis.
Benefits: They help find deep infiltrating endometriosis and endometriomas better.
Can You See Endometriosis on Ultrasound? The Short Answer
Ultrasound technology has made big strides in spotting endometriosis. But, how well it works depends on the type of endometriosis and the ultrasound method used. Seeing endometriosis on an ultrasound isn’t always easy. It depends on several things, like the ultrasound type and the endometriosis’s details.
Detection Rates by Ultrasound Type
Ultrasound types differ in their ability to find endometriosis. Transvaginal ultrasound (TVUS) is great for spotting endometriomas and deep endometriosis. Research shows TVUS is very accurate in finding deep endometriosis.
How well ultrasound finds endometriosis also depends on the type. For example, endometriomas, which are cysts related to endometriosis, are easier to spot than superficial peritoneal endometriosis.
Sensitivity and Specificity Statistics
Ultrasound’s sensitivity and specificity in finding endometriosis are key. For deep endometriosis and endometriomas, TVUS has a sensitivity of 88-96% and specificity of 79-94%. These numbers show TVUS is a reliable tool for diagnosing some endometriosis types.
It’s important for both doctors and patients to understand these numbers. High sensitivity means most endometriosis cases are correctly identified. High specificity means the test is good at ruling out endometriosis in those who don’t have it.
Endometriomas: The Most Detectable Form on Ultrasound
Endometriomas are the most visible form of endometriosis on ultrasound. They are also known as chocolate cysts. These cysts form when endometrial tissue grows in the ovaries.
Characteristic “Ground-Glass” Appearance
Endometriomas look different on ultrasound. They have a “ground-glass” echo pattern. This is because of the hemorrhagic debris inside the cyst.
Differentiating from Other Ovarian Cysts
It’s important to tell endometriomas apart from other ovarian cysts. Look for low-level internal echoes and no significant vascularity. Sometimes, you’ll see “shading” or a gradual change in the cyst’s appearance.
- Low-level internal echoes: Show the presence of hemorrhagic content.
- Absence of significant vascularity: Helps rule out malignant or highly vascular lesions.
- “Shading”: Suggests the presence of old blood products.
Diagnostic Accuracy for Ovarian Endometriosis
Ultrasound is very good at detecting endometriomas. Studies show it has high sensitivity and specificity. This is key for managing and treating patients with suspected endometriosis.
Knowing how to spot endometriomas on ultrasound helps doctors better care for patients. It improves the detection and management of ovarian endometriosis.
Deep Infiltrating Endometriosis and Ultrasound Detection
Ultrasound is a big help in finding deep infiltrating endometriosis. This serious form of endometriosis goes deep into the pelvic area. It can hurt important parts like the bowel, bladder, and uterosacral ligaments.
Finding deep infiltrating endometriosis needs a lot of skill and special tools. We’ll look at how to spot it and how good these methods are.
Specialized Techniques for Deep Endometriosis
There are special ultrasound methods for spotting deep infiltrating endometriosis. These methods check the pelvic area carefully. They look at the back, front, and sides of the pelvis.
Transvaginal ultrasound with a special endometriosis setting is key. It lets us see the pelvic area well and find deep endometriosis spots.
Visualizing Uterosacral Ligament Involvement
The uterosacral ligaments often have deep infiltrating endometriosis. Seeing if these ligaments are affected is very important. It helps plan the right treatment.
We use a transvaginal ultrasound gently. This lets us check the ligaments for signs of endometriosis. Signs include thickening, bumps, or tenderness.
Sensitivity of 88-96% with Expert Protocols
Experts say ultrasound can spot deep infiltrating endometriosis 88-96% of the time. This shows how important it is to have skilled people doing these scans.
Ultrasound Technique | Sensitivity for Deep Endometriosis |
Transvaginal Ultrasound with Specialized Protocol | 88-96% |
Standard Transvaginal Ultrasound | Significantly lower than specialized protocol |
Using these advanced ultrasound methods helps us find and treat deep infiltrating endometriosis better. This means better care for our patients.
Superficial Endometriosis: Why It’s Hard to See on Ultrasound
Superficial endometriosis is hard to spot on ultrasound because it’s so subtle. This type of endometriosis affects the peritoneal surface and can spread out. But, it often slips past standard ultrasound scans.
Limitations of Ultrasound for Peritoneal Disease
Ultrasound has a hard time showing superficial endometriosis. Ultrasound waves struggle to provide clear images of the peritoneal surface, where these lesions are found. Even skilled sonographers might miss them.
Some main issues include:
- The subtlety of superficial lesions, which can be very small or flat.
- The location of these lesions on the peritoneal surface, which can be hard to see.
- The similarity in appearance between endometriosis lesions and normal peritoneal tissue.
Visualization with Fluid in Pouch of Douglas
Fluid in the pouch of Douglas can help see superficial endometriosis better. Fluid acts as a natural contrast agent, making it easier to spot the peritoneum and any issues. But, this method isn’t always reliable because fluid levels vary.
When fluid is there, it can:
- Highlight adhesions or scarring associated with endometriosis.
- Outline the edges of lesions, making them more visible.
Why Routine Ultrasound Has Only 25% Sensitivity
Routine ultrasound exams can only spot superficial endometriosis about 25% of the time. This low rate is because of ultrasound’s limits and the tiny size of these lesions.
The reasons for this low rate include:
Factor | Impact on Detection |
Lack of Specific Protocols | Routine ultrasounds are not optimized for endometriosis detection. |
Operator Dependence | The skill and experience of the sonographer play a significant role. |
Lesion Characteristics | Small or flat lesions are harder to detect. |
In conclusion, while ultrasound is great for many gynecological issues, it’s not the best for superficial endometriosis. We need better ultrasound tech and more training for sonographers to find these lesions more often.
The Role of Expert Sonographers in Endometriosis Detection
Expert sonographers play a big role in finding endometriosis through ultrasound. They have the skills to spot signs of endometriosis that others might miss.
Standard vs. Expert-Guided Ultrasound
Regular ultrasound tests are done by sonographers who might not know much about endometriosis. But, expert sonographers are trained to find endometriotic lesions.
Key differences between standard and expert-guided ultrasounds include:
- Detailed examination of the pelvic anatomy
- Use of specialized techniques to visualize endometriotic lesions
- Enhanced ability to detect deep infiltrating endometriosis
How Specialized Training Improves Detection to 78%
Research shows that training sonographers can really help find endometriosis. With the right training, they can spot endometriosis up to 78% of the time.
“Expert sonographers trained in endometriosis-specific techniques can identify disease extending beyond the ovaries,” showing how important training is.
Sonographer Training Level | Detection Rate |
Standard Training | Lower detection rate |
Specialized Training | Up to 78% |
Finding an Endometriosis Imaging Specialist
Looking for a precise endometriosis diagnosis? You need a healthcare provider who knows about endometriosis imaging. Ask your doctor for a referral to a specialist who uses advanced ultrasound.
Choosing a specialist means your ultrasound will be done with the utmost care and accuracy. This boosts your chances of getting a correct endometriosis diagnosis.
Anatomical Mapping of Endometriosis with Ultrasound
Ultrasound is key in mapping endometriosis. It helps doctors see where and how bad the lesions are. This info is vital for treatment plans.
Bowel Involvement
Endometriosis can hurt the bowel, causing pain or blockages. Ultrasound spots deep lesions in the bowel. This is important for treatment.
Bowel involvement is a serious complication of endometriosis. Ultrasound finds signs like dark spots or adhesions. These show bowel endometriosis.
Ultrasound Feature | Description | Clinical Significance |
Hypoechoic Lesions | Dark areas on ultrasound indicating possible endometriotic nodules | Suggests bowel wall infiltration by endometriosis |
Adhesions | Presence of fibrotic bands between organs | May indicate chronic inflammation and scarring |
Nodule Location | Rectal or sigmoid colon involvement | Affects surgical planning and treatment approach |
Bladder and Ureter Endometriosis
Endometriosis can hit the bladder and ureters too. Ultrasound spots lesions or thickening in the bladder. Ureteral issues can cause kidney swelling.
Pelvic Sidewall Disease
Endometriosis on the pelvic sidewall is hard to spot but very important. Ultrasound finds lesions or thickening. This might involve ureters or big blood vessels.
Checking the pelvic sidewall well is key for surgery. It makes sure all affected areas get treated.
What to Expect During an Endometriosis-Focused Ultrasound
An endometriosis-focused ultrasound is a key test for many patients. It gives valuable insights into their condition. This special ultrasound shows the reproductive organs in detail and finds any endometriosis-related issues.
Preparation Instructions
To make sure the ultrasound goes well, you need to prepare. Here’s what you can do:
- Hydrate: Drink lots of water before the test. This fills your bladder, making the images clearer.
- Follow Instructions: Your doctor might tell you to eat certain foods or prepare your bowel before the ultrasound.
- Comfortable Clothing: Wear clothes that are easy to move in. This helps the sonographer get a good view of your lower abdomen.
By following these steps, you help make sure the ultrasound gives accurate and helpful information for your diagnosis.
The Examination Process
A skilled sonographer will do the ultrasound. They might use a transvaginal or transabdominal probe, or both, depending on your needs.
- The sonographer will apply gel to your abdomen or use a transvaginal probe. This captures detailed images of your reproductive organs.
- They will look at the images in real-time. They’re looking for signs of endometriosis, like endometriomas or adhesions.
- The whole process usually takes 30-60 minutes, depending on how complex your case is.
The sonographer will make sure you’re comfortable and answer any questions you have.
Understanding Your Results
After the ultrasound, your doctor will look at the images and talk to you about them. If they find endometriosis, they’ll tell you how bad it is.
“The ultrasound findings will guide our treatment decisions and help us develop a personalized plan to manage your symptoms.”
Your doctor might suggest more tests or talk about treatment options. It’s important to follow up with them to understand what’s next in your care.
Knowing what to expect from an endometriosis-focused ultrasound can make you feel more ready and confident during the test.
When Ultrasound Misses Endometriosis: Next Steps
Ultrasound can miss some types of endometriosis. This means doctors need to use other tests to find it. They look for other ways to check for endometriosis because ultrasound can’t find all of it.
The Importance of Clinical Correlation
When ultrasound doesn’t show anything, doctors look at other signs. They use the patient’s symptoms, medical history, and physical exam to decide what to do next.
Key factors to consider in clinical correlation include:
- Severity and duration of symptoms
- Presence of risk factors for endometriosis
- Physical examination findings, such as tenderness or nodularity
Doctors use these signs along with ultrasound results to decide on further tests.
Alternative Imaging Options
For unclear ultrasound results, doctors might use other imaging. Magnetic Resonance Imaging (MRI) is one choice. It’s good at finding deep endometriosis and cysts.
“MRI has emerged as a valuable tool in the diagnosis of endometriosis, particularlly for deep infiltrating disease.”Source: Expert Opinion on Medical Diagnostics
MRI shows detailed pictures of the pelvic area. It helps see how far endometriosis has spread. But, it’s mainly used for tricky cases or when surgery is planned.
Laparoscopy as the Gold Standard
Laparoscopy is the best way to find endometriosis. It lets doctors see the pelvic area directly. They can also take biopsies to confirm the diagnosis.
- Direct visualization of endometriotic lesions
- Ability to perform surgical treatment during the same procedure
- Opportunity for histological confirmation
In summary, when ultrasound can’t find endometriosis, doctors use a detailed plan. This includes looking at symptoms, trying other imaging, and sometimes laparoscopy. This ensures the right diagnosis and treatment.
Conclusion: The Future of Endometriosis Imaging
Medical imaging is getting better, making it easier to find and treat endometriosis. Ultrasound technology is now a key tool in spotting endometriosis. This is thanks to new methods and skilled sonographers.
Studies show ultrasound can really help find endometriosis. Using special ultrasound techniques, doctors can spot it more often. This means we can start treating it sooner, helping patients feel better faster.
Expert sonographers play a big role in finding endometriosis. They know how to look for it, even in hard-to-spot cases. As we keep improving our imaging, we’ll get even better at diagnosing and treating endometriosis.
We’re making great strides in endometriosis imaging. With better ultrasound tech and other tools, patient care will only get better. So, can an ultrasound show endometriosis? Yes, it can, with the right skills and tools.
FAQ
Can endometriosis be detected using ultrasound?
Yes, ultrasound can spot certain types of endometriosis. This includes endometriomas and deep infiltrating endometriosis. It’s best when done by skilled sonographers using special techniques.
What type of ultrasound is best for detecting endometriosis?
Transvaginal ultrasound (TVUS) is better than transabdominal ultrasound for finding endometriosis. This is true, even more so when using special endometriosis protocols.
Can superficial endometriosis be seen on ultrasound?
Superficial endometriosis is hard to find with regular ultrasound. It’s small and on the peritoneal surface. Routine ultrasound can only spot it about 25% of the time.
How accurate is ultrasound in diagnosing endometriomas?
Ultrasound is very good at spotting endometriomas. They look like a “ground-glass” on the screen. Studies show it’s very accurate for finding ovarian endometriosis.
Can ultrasound detect deep infiltrating endometriosis?
Yes, ultrasound can find deep infiltrating endometriosis with the right techniques. It’s about 88-96% accurate. It can even see involvement of the uterosacral ligaments.
What should I expect during an endometriosis-focused ultrasound?
You’ll get a detailed check with transvaginal ultrasound. Sometimes, transabdominal ultrasound is used too. The sonographer will look for signs of endometriosis in the pelvic area.
How can I prepare for an endometriosis ultrasound?
You might need a full bladder for transabdominal ultrasound. Your healthcare provider will give you specific instructions for the transvaginal ultrasound.
What if ultrasound misses endometriosis?
If ultrasound misses endometriosis, it’s important to match the findings with your symptoms. You might need MRI or laparoscopy for a clear diagnosis.
Can ultrasound map the extent of endometriosis in the pelvic region?
Yes, ultrasound can show how far endometriosis has spread. This includes bowel, bladder, and ureter involvement, and pelvic sidewall disease. Expert sonographers are best for this.
Why is it important to see an expert sonographer for endometriosis ultrasound?
Seeing an expert sonographer can greatly improve detection rates. They are trained to spot endometriosis, including deep infiltrating types, better than regular ultrasound.
References
National Center for Biotechnology Information. Endometriosis Diagnosis: Advanced Ultrasound Imaging. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9334891/





